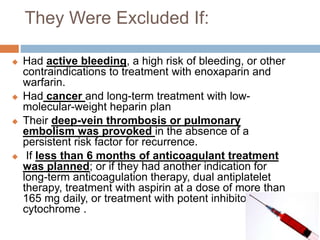
The document reports on a study comparing the efficacy and safety of oral apixaban with conventional anticoagulant therapy in treating acute venous thromboembolism. The findings indicate that apixaban is as effective as traditional treatment but with a significant reduction in major bleeding incidents. This suggests that apixaban may offer a simpler and safer alternative for patients requiring anticoagulation.