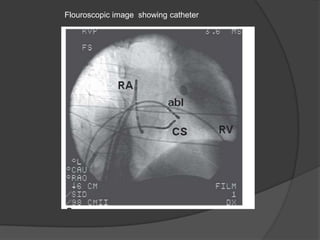
This document discusses the classification and mechanisms of action of various anti-arrhythmic drugs. It describes five classes of anti-arrhythmic drugs based on their effects on cardiac ion channels and muscle fibers. Class I drugs block sodium channels, Class II drugs are beta blockers, Class III drugs prolong the cardiac action potential, and Class IV drugs block calcium channels. The uses, examples and side effects of each drug class are provided. Other therapeutic procedures for treating arrhythmias including defibrillation, cardioversion, catheter ablation, and pacemakers are also briefly mentioned.