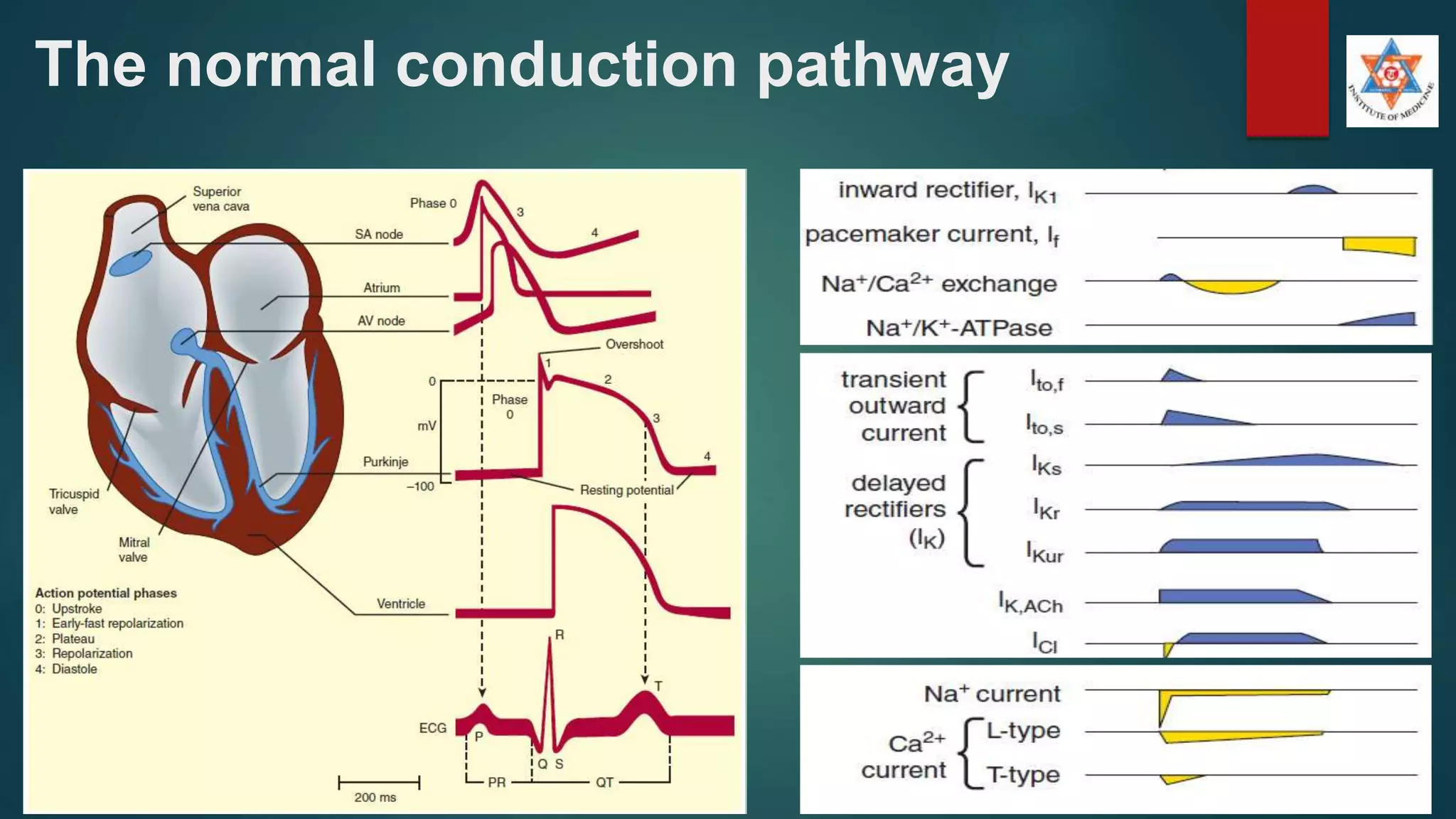
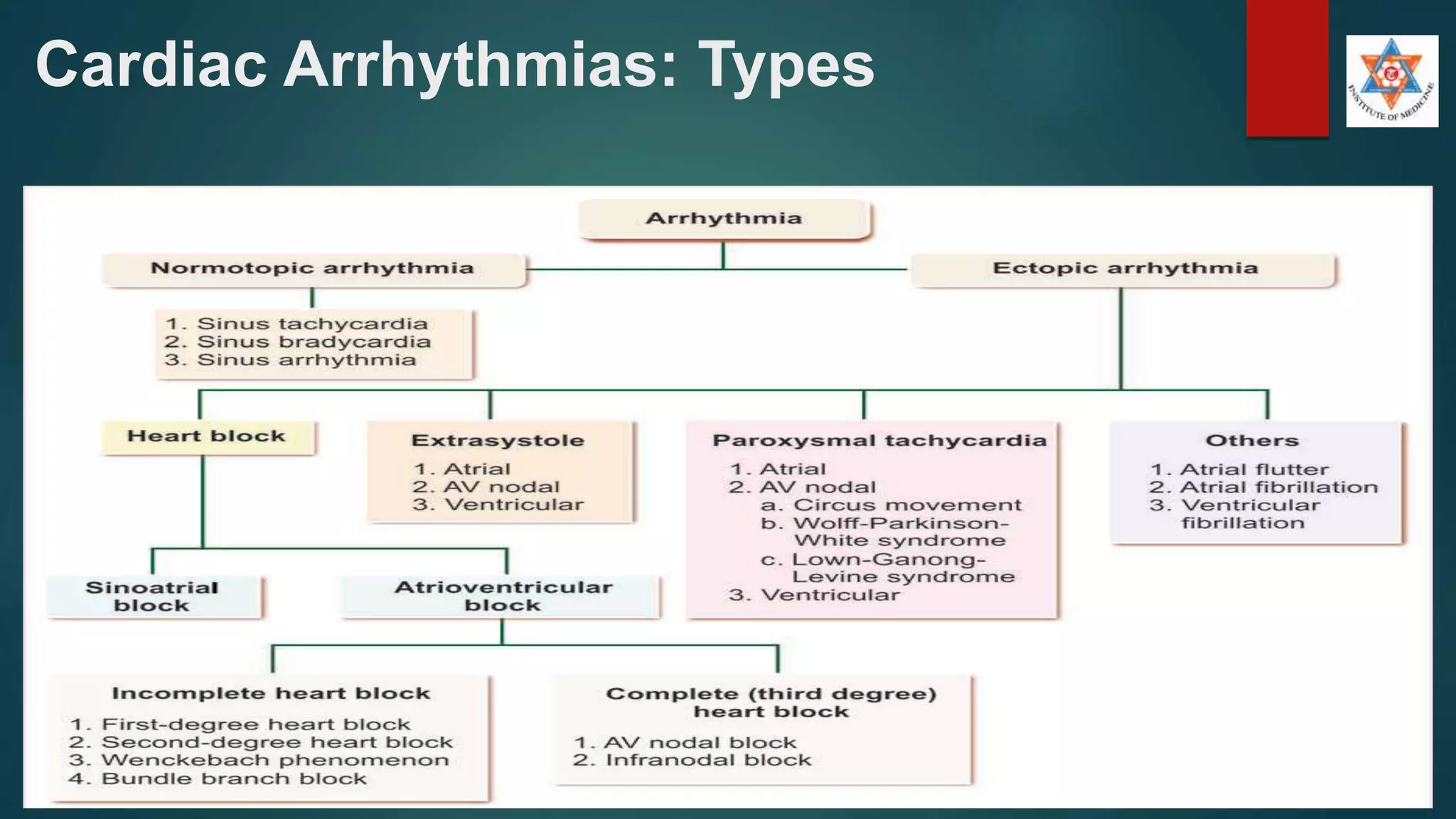
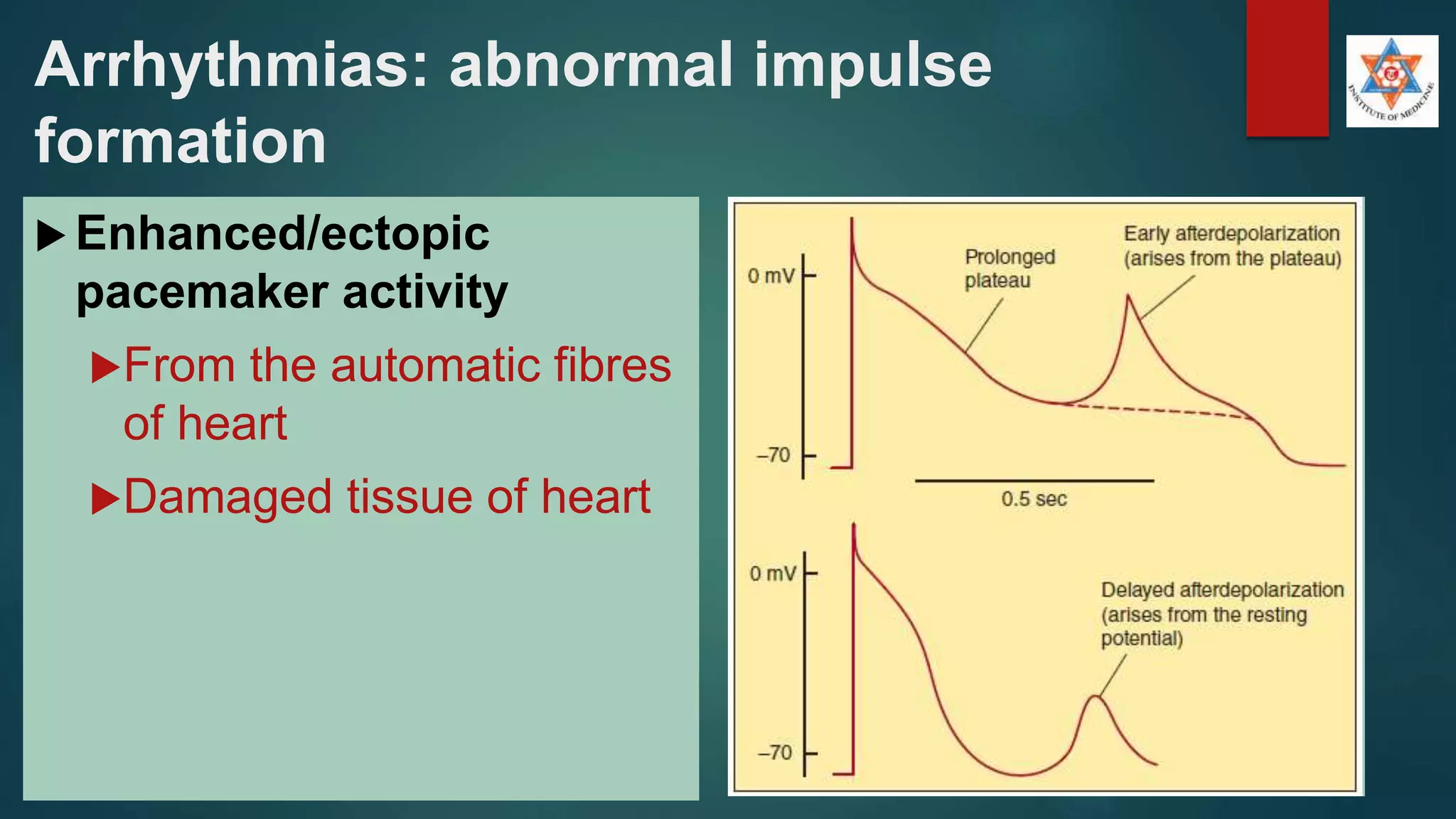
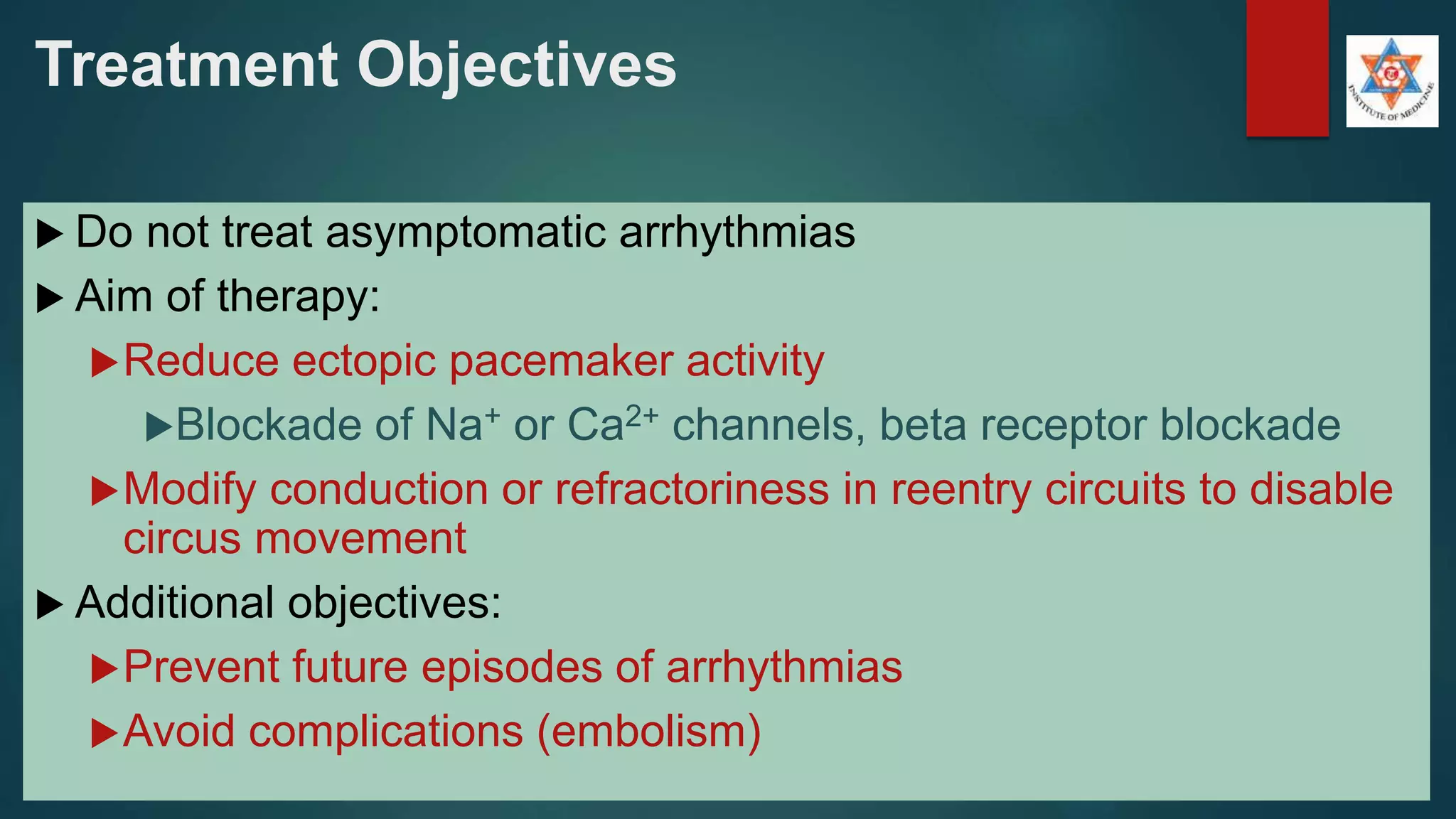
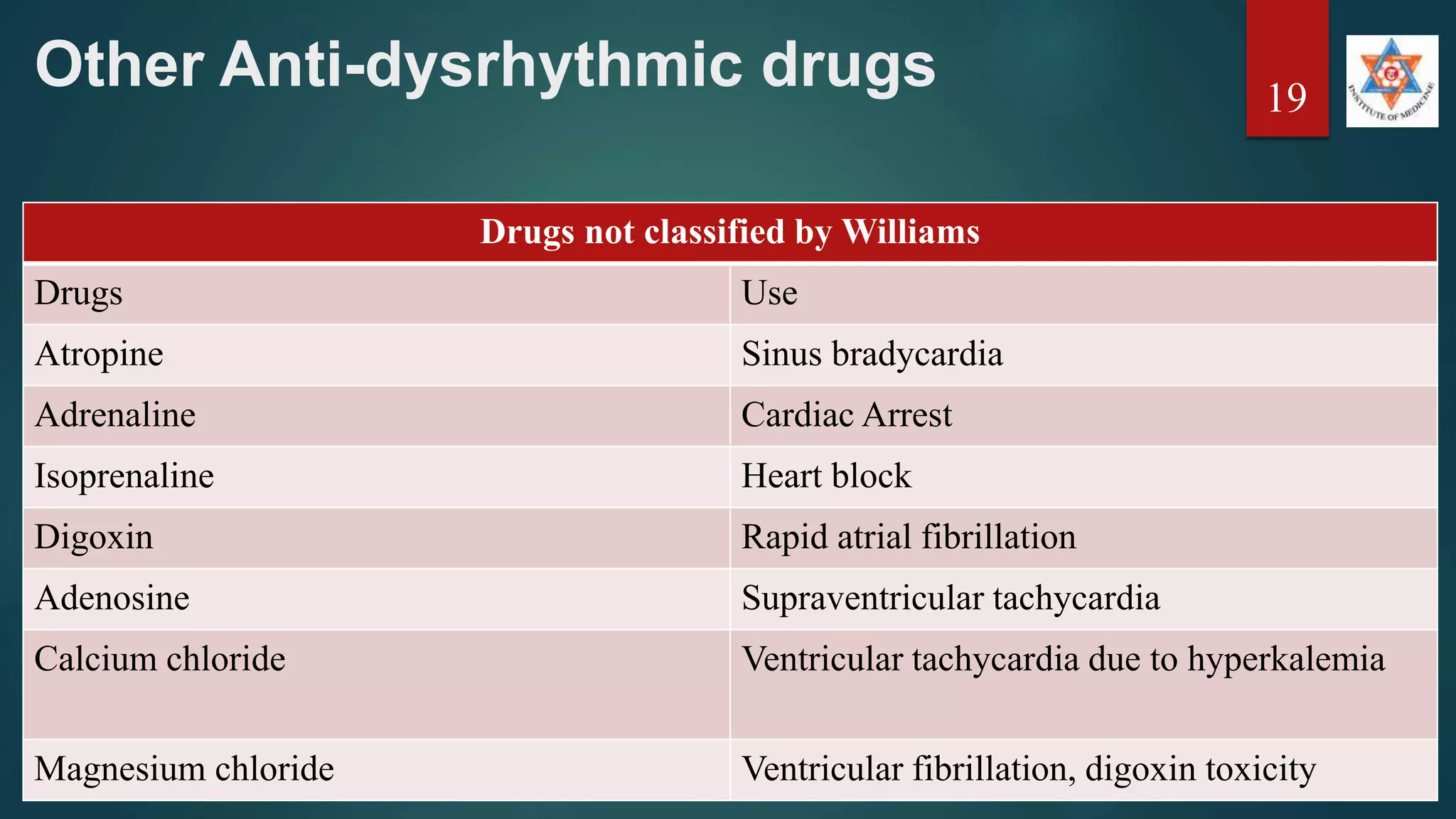
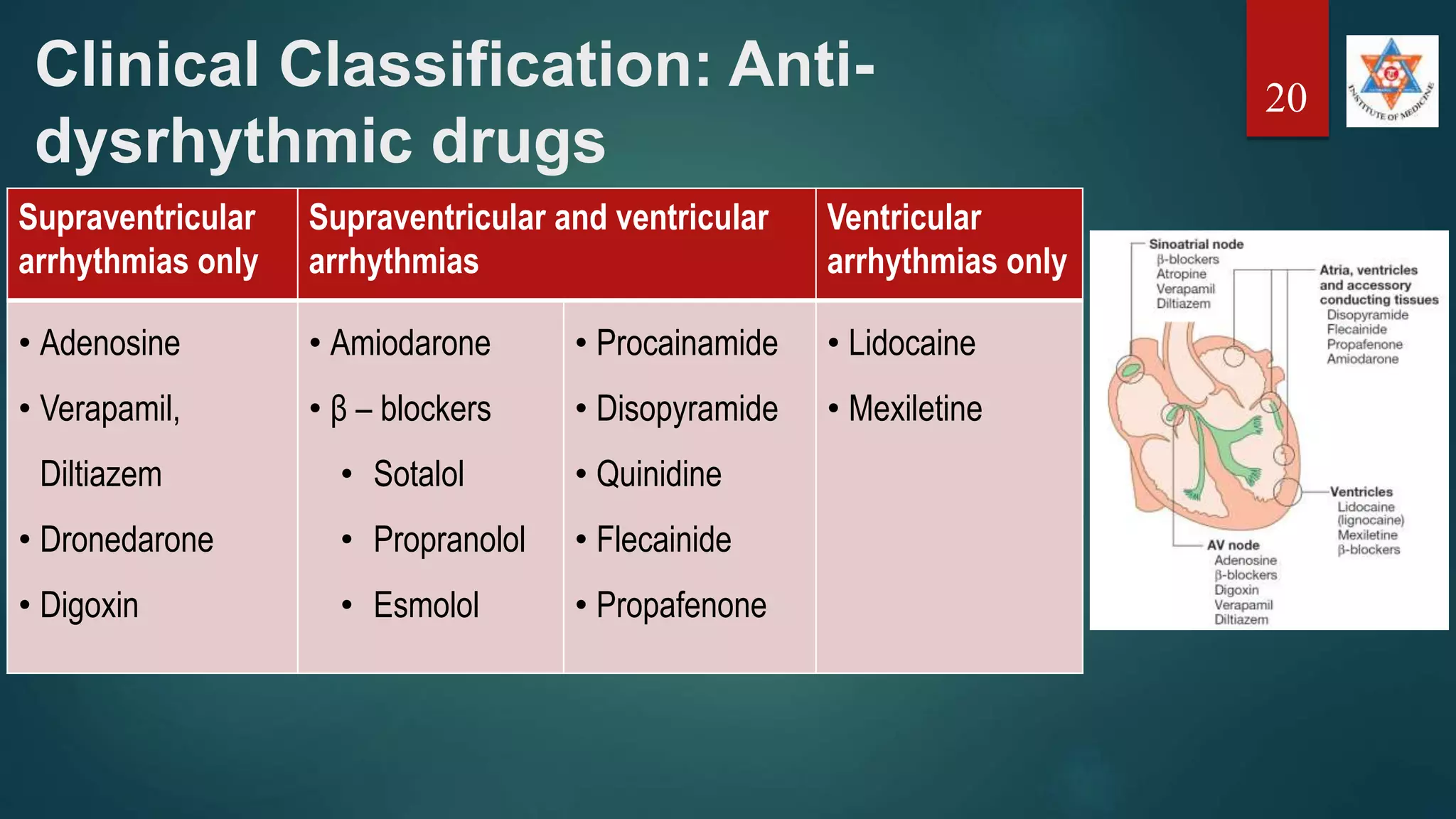
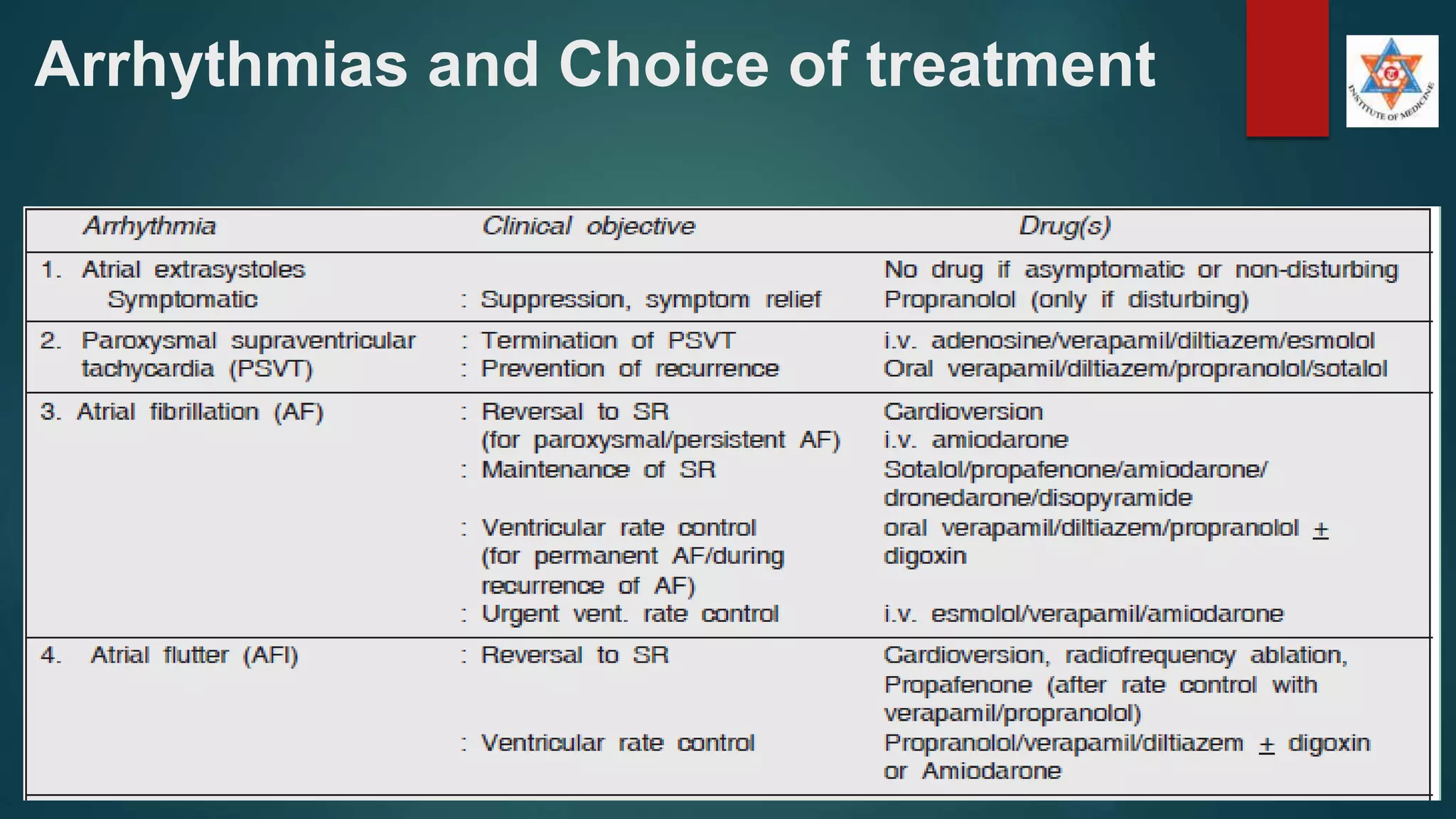
The document covers the topic of cardiac arrhythmias, providing definitions, mechanisms, clinical presentations, and treatment options, particularly pharmacotherapy. It emphasizes that arrhythmias can range from asymptomatic to life-threatening and highlights the importance of non-pharmacological treatment alongside drug therapy. The document also categorizes antiarrhythmic agents and discusses the drugs used for managing various types of arrhythmias.