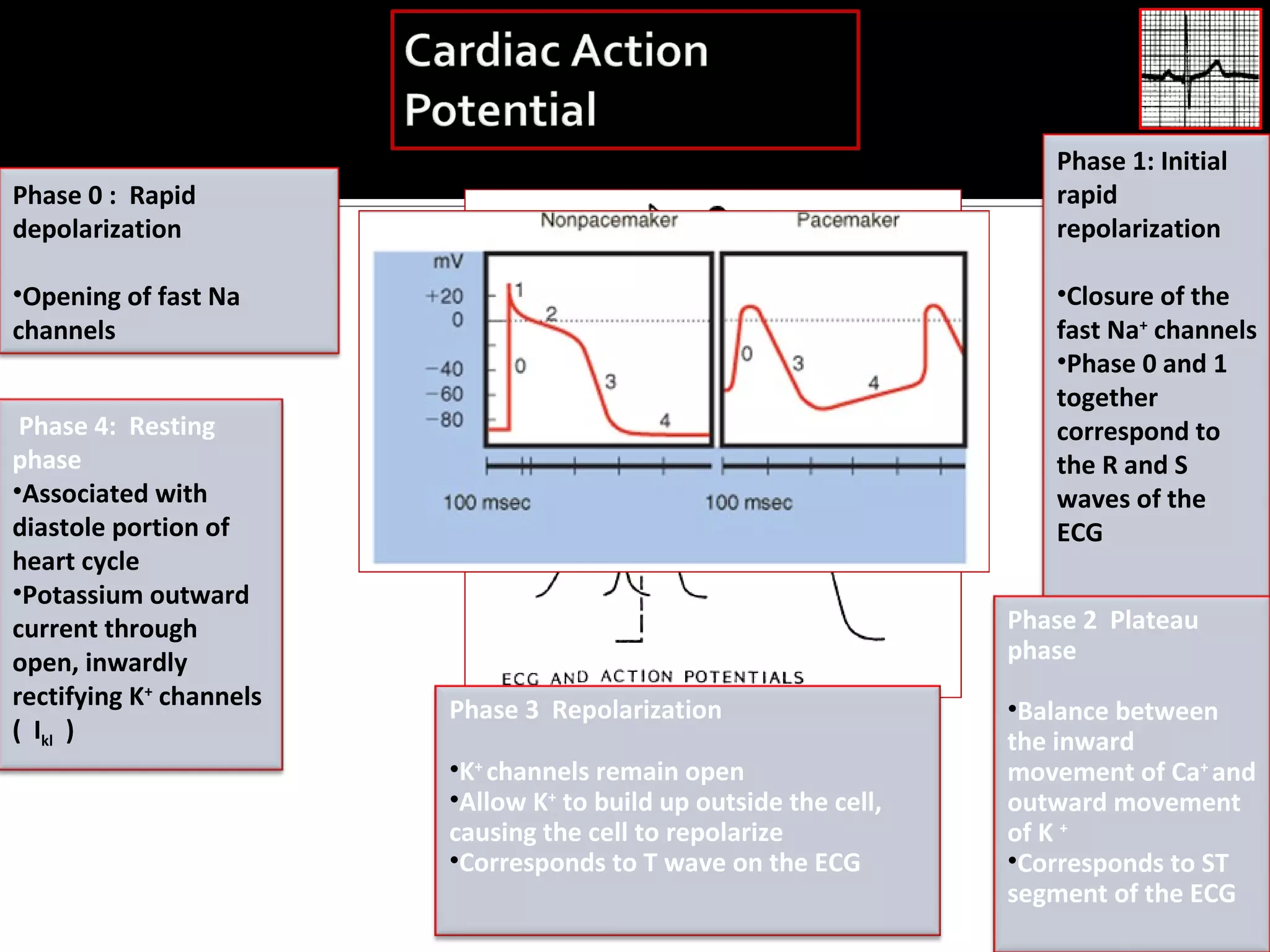
1. Cardiac arrhythmias can be caused by disorders of impulse formation, disorders of impulse conduction, or a combination of the two. Disorders of impulse formation include abnormalities in automaticity and triggered activity.
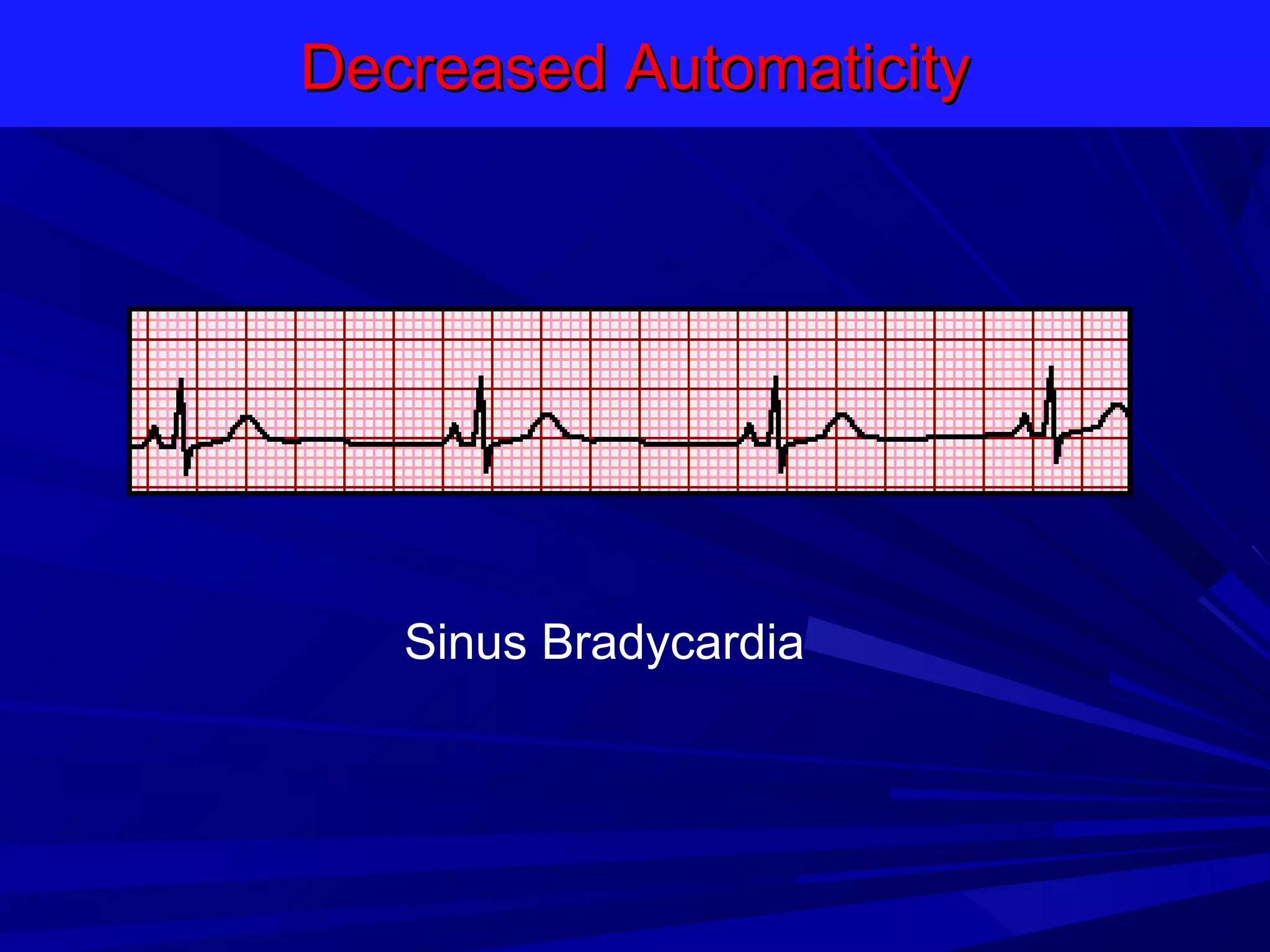
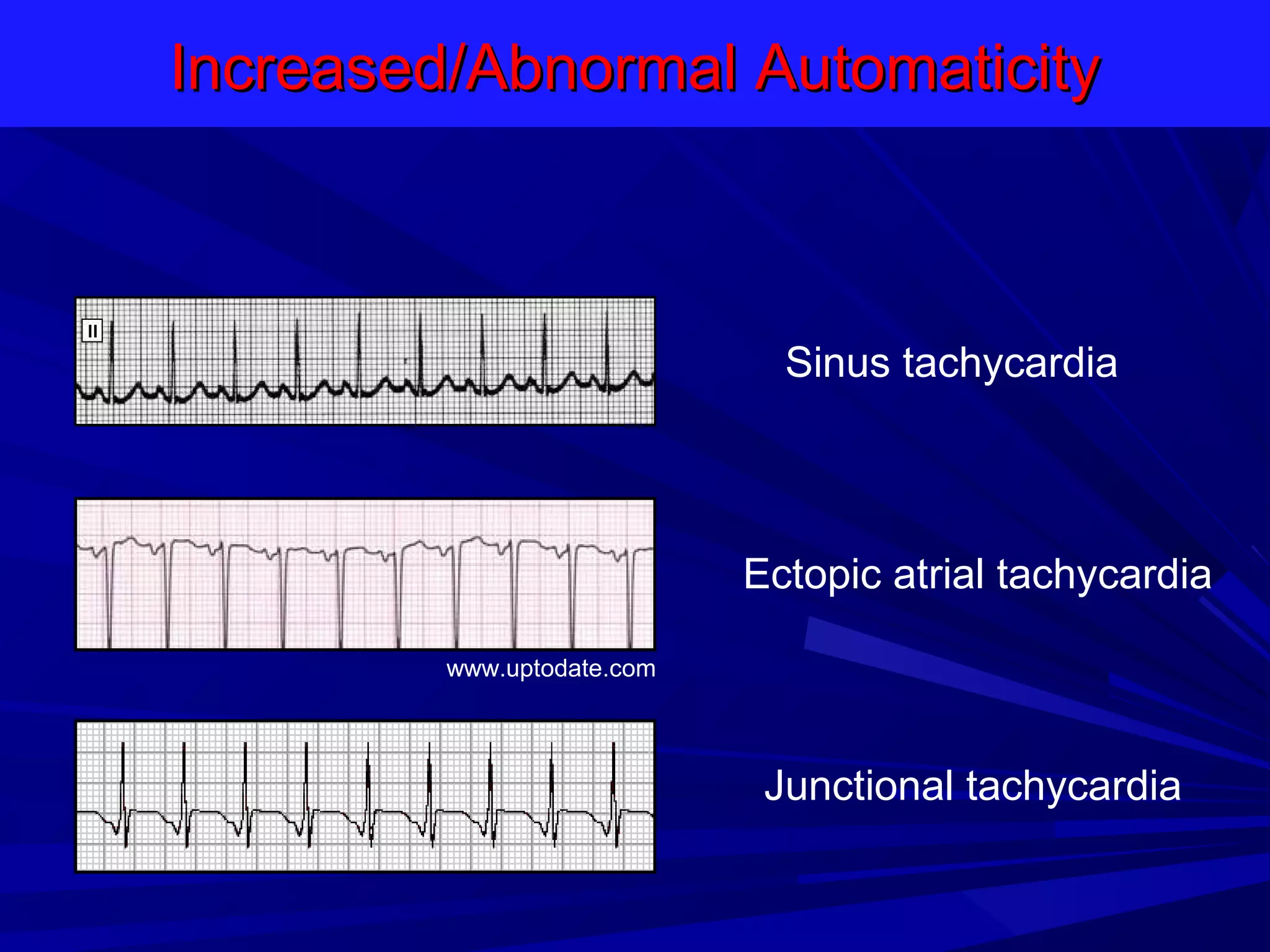
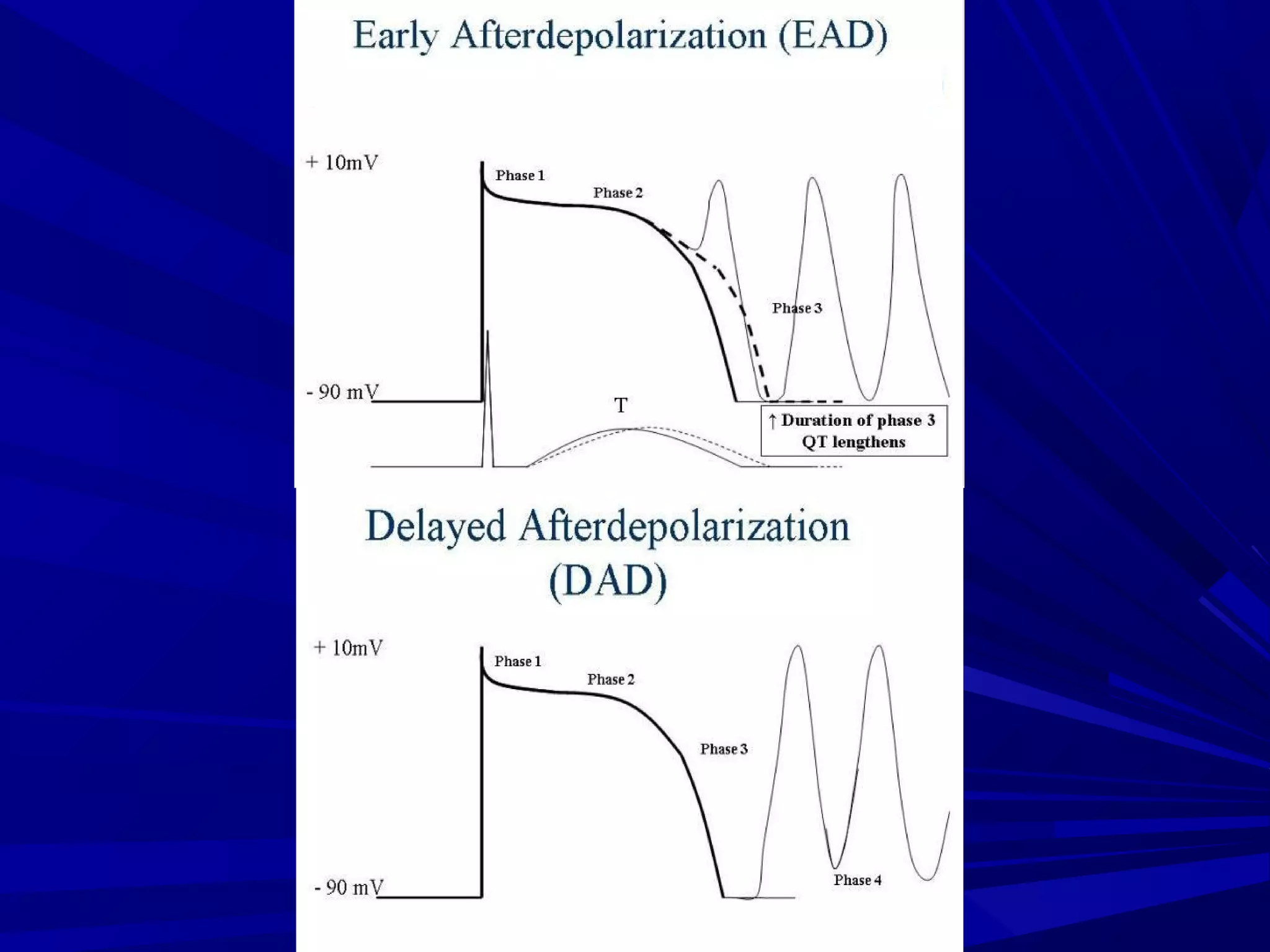
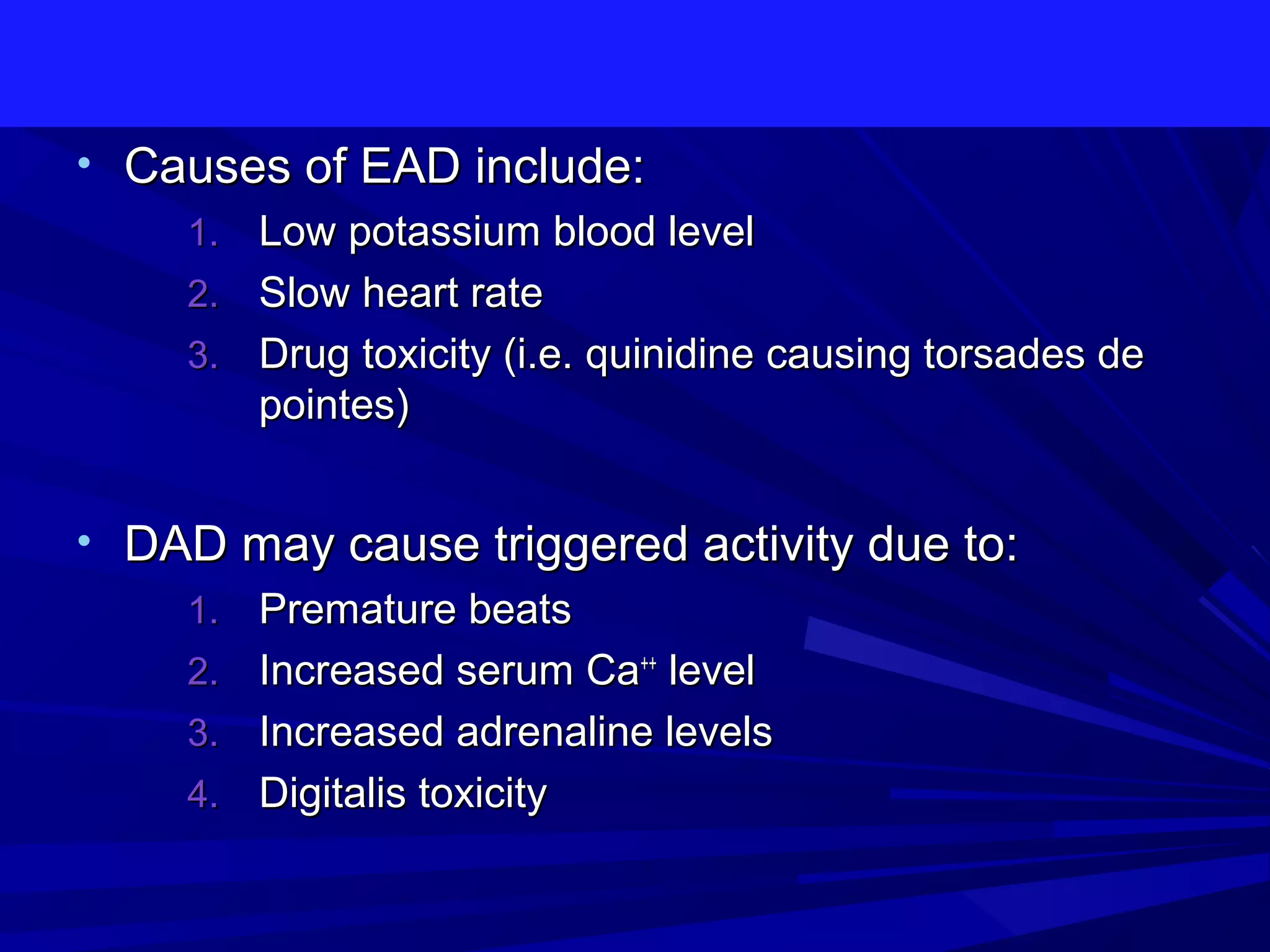
2. Abnormal automaticity occurs when an ectopic pacemaker fires at an inappropriate rate, taking over control of the heart rhythm from the normal sinus node. Triggered activity is initiated by afterdepolarizations following an action potential.
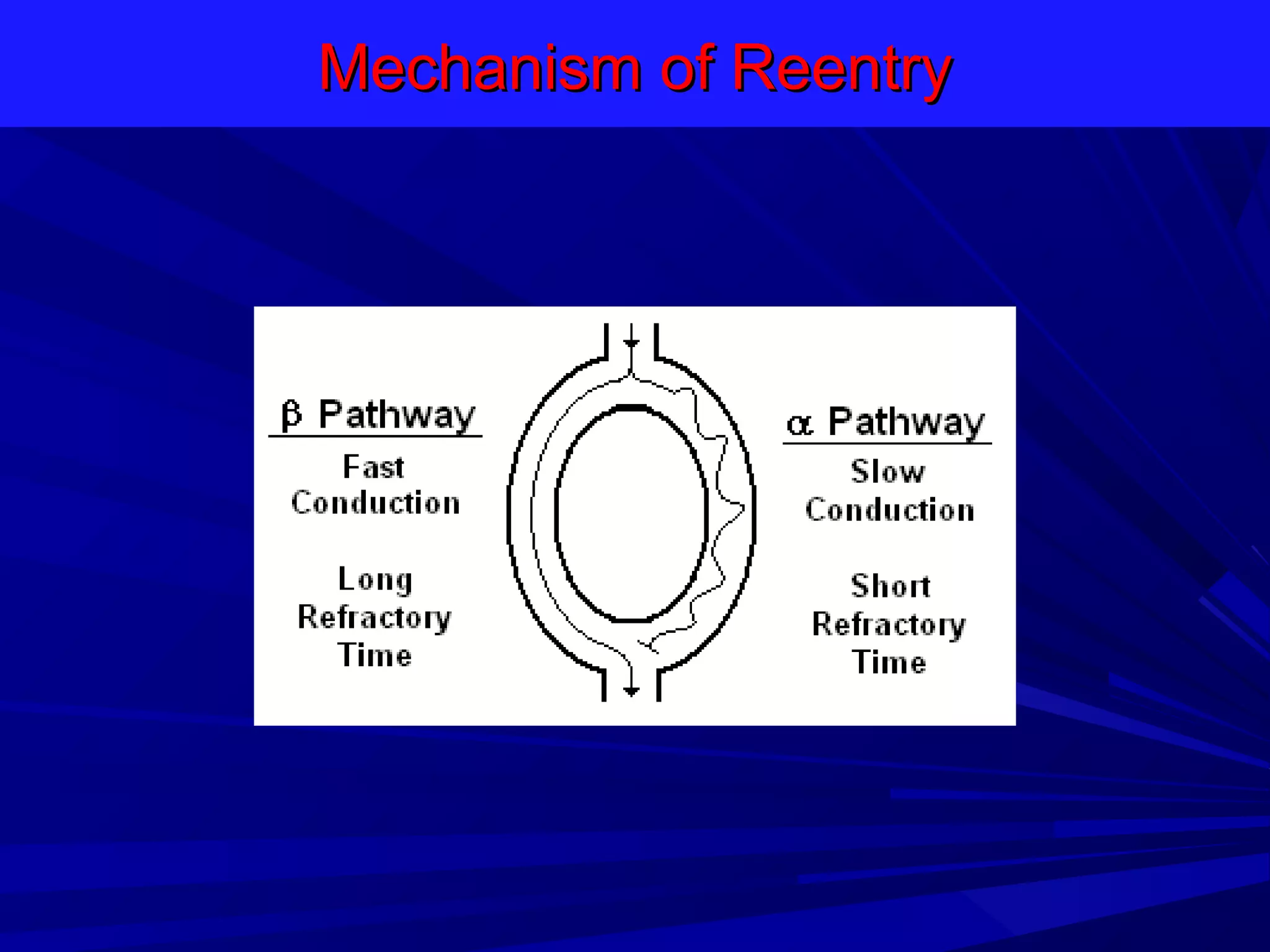
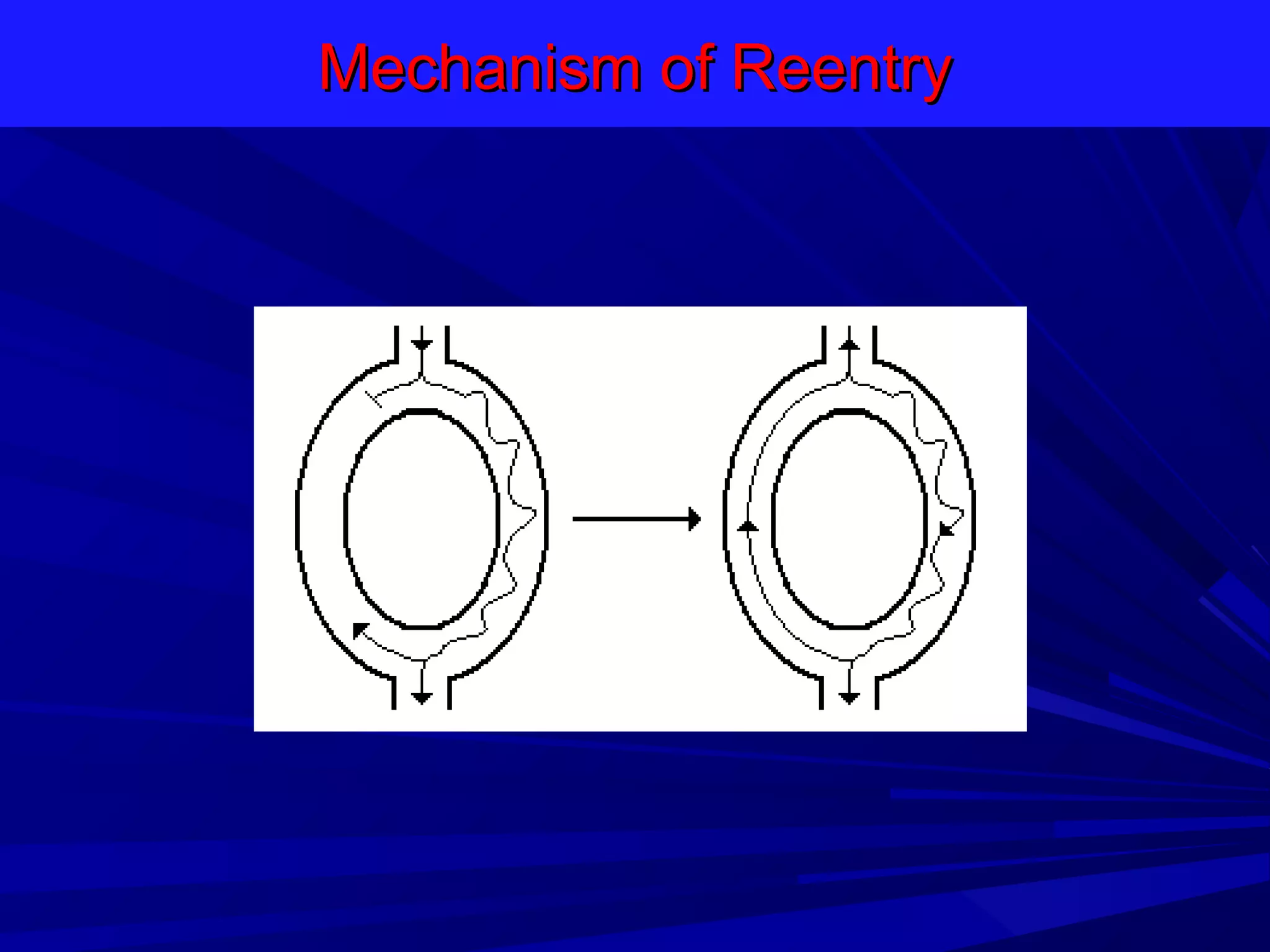
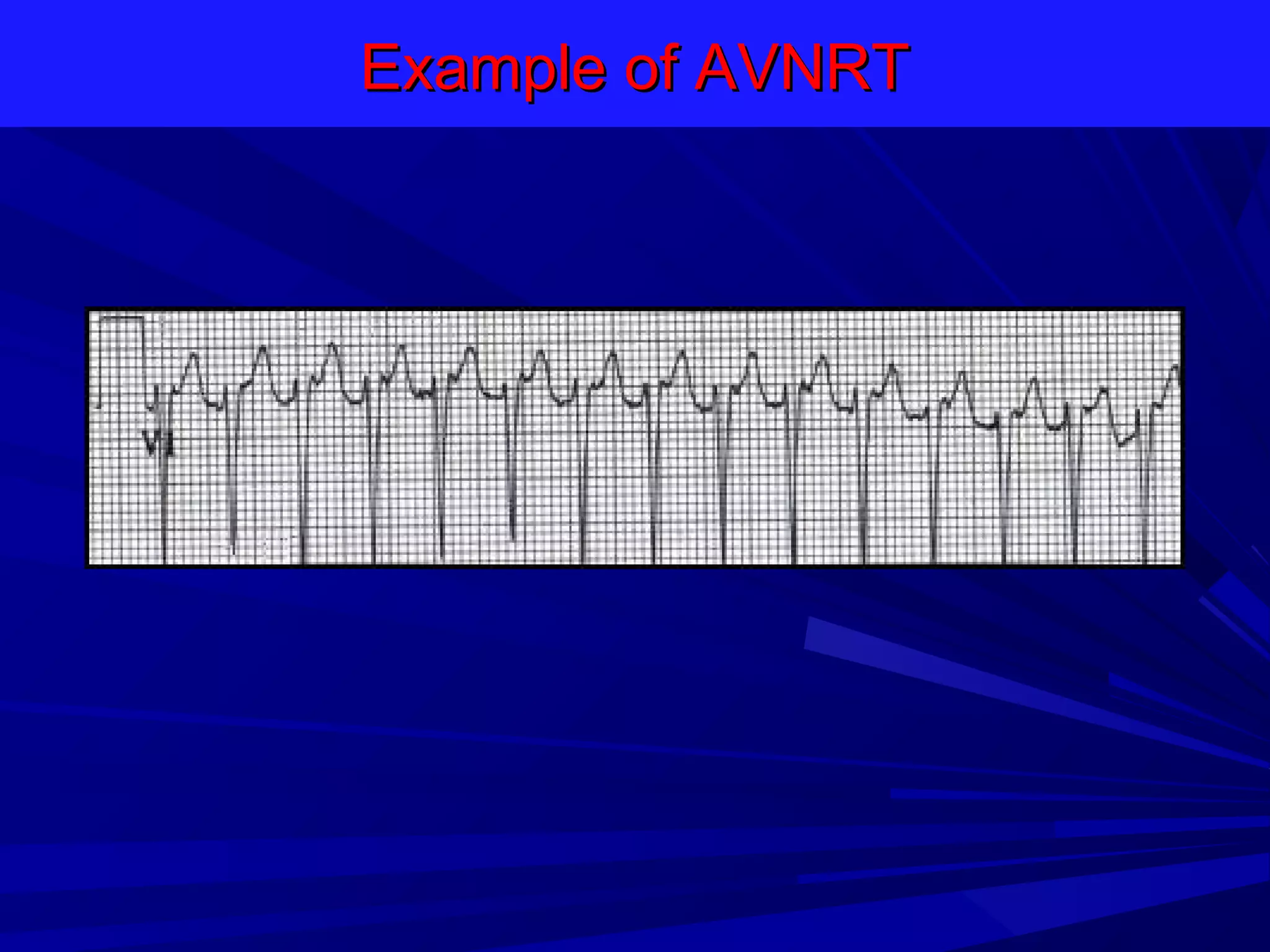
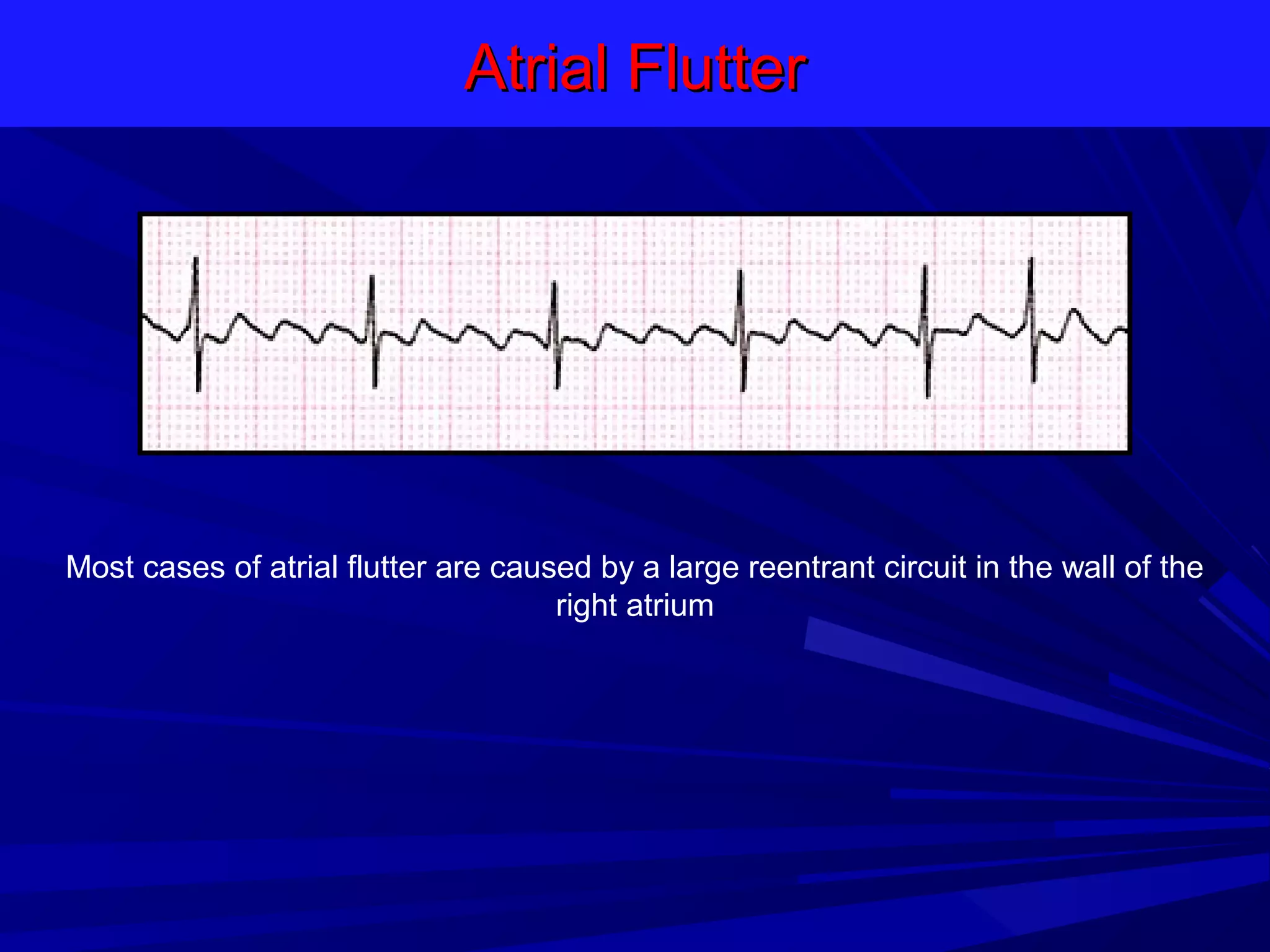
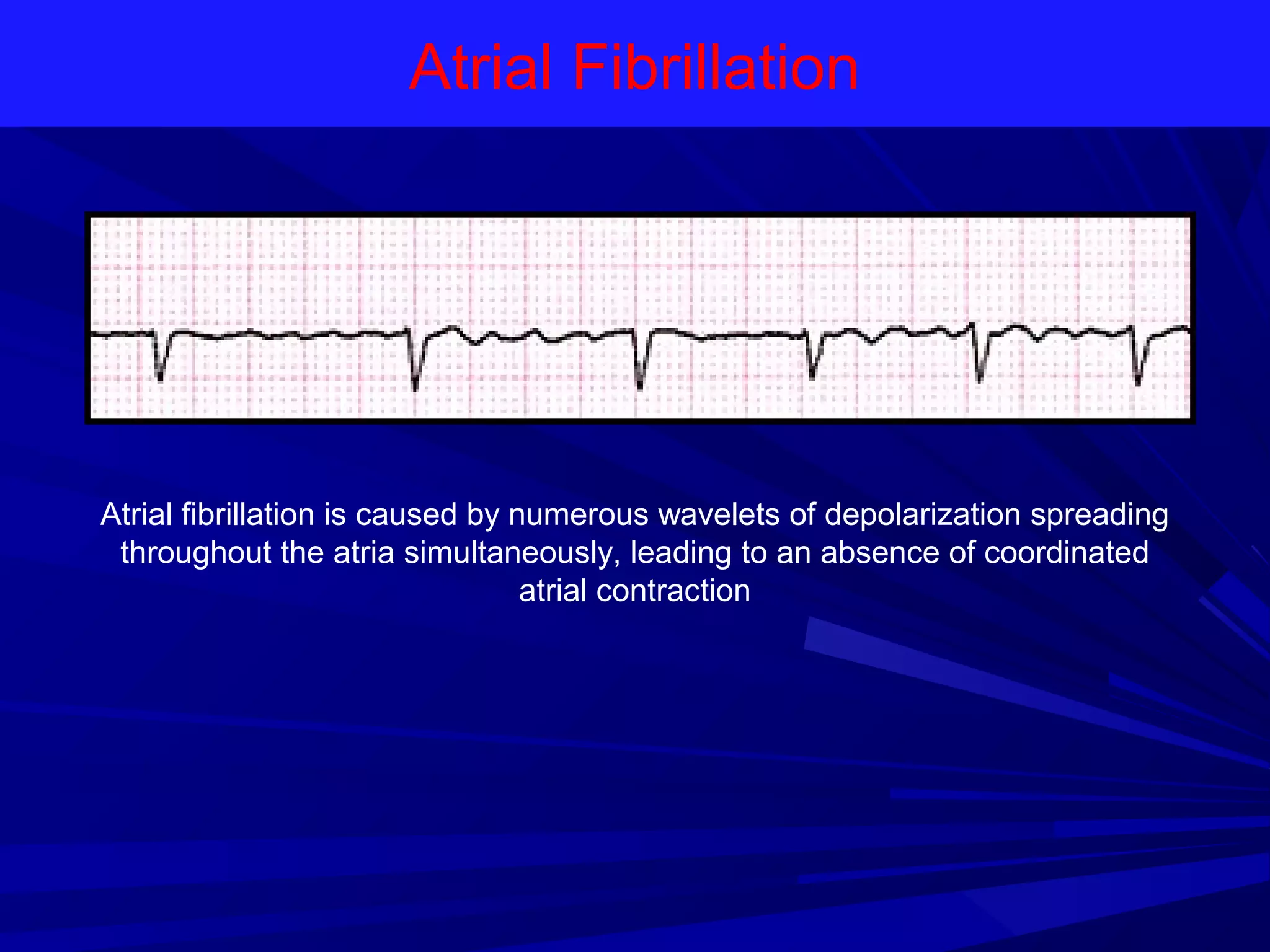
3. Disorders of impulse conduction include conduction block and reentry, which is when an impulse circles back and reactivates tissue that is still recovering, leading to sustained, rapid rhythms. Common reentrant arrhythmias include atrial flutter, at