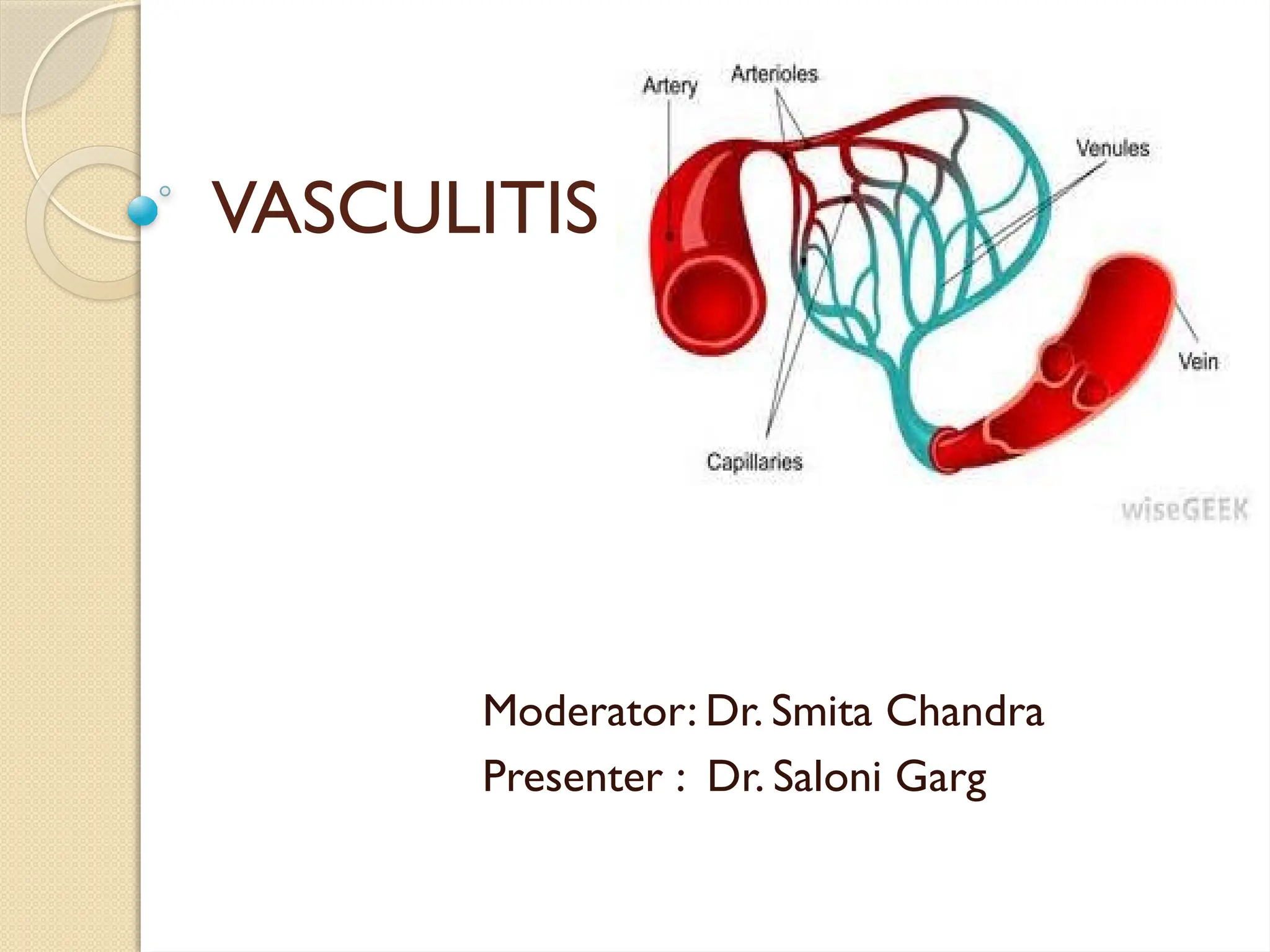
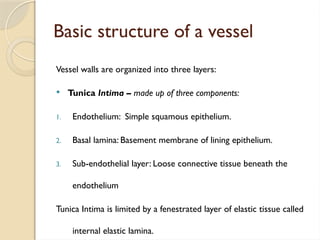
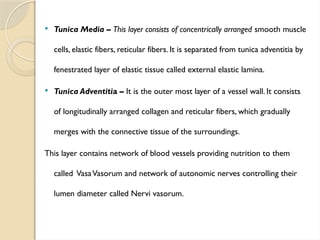
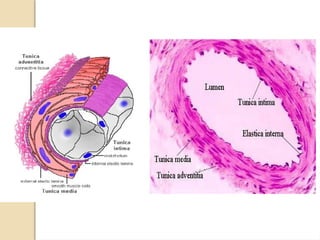
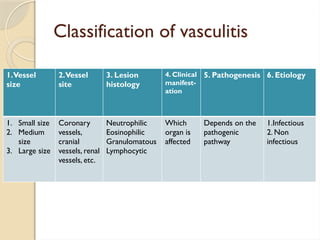
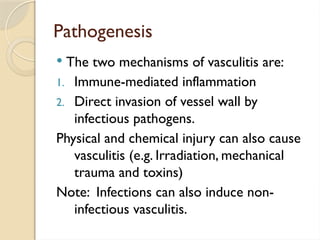
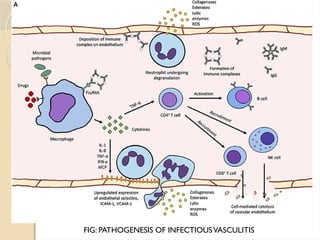
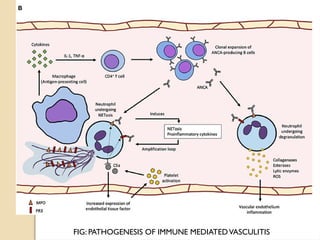
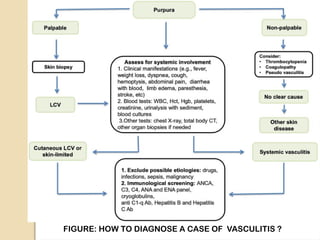
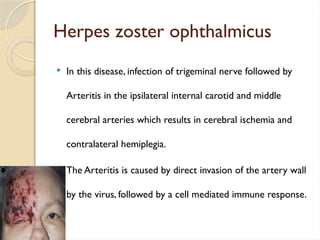
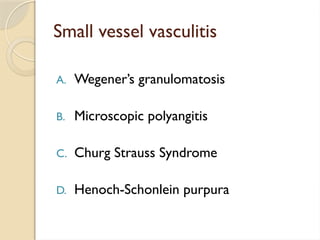
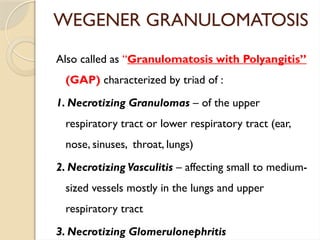
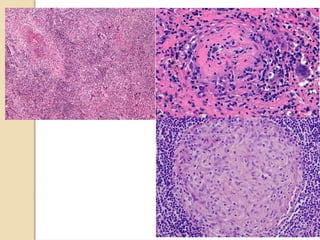
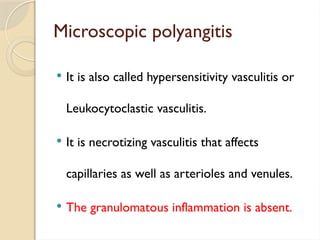
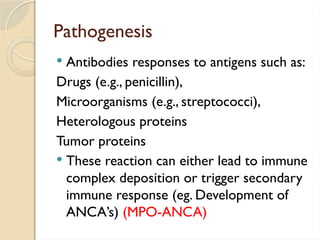
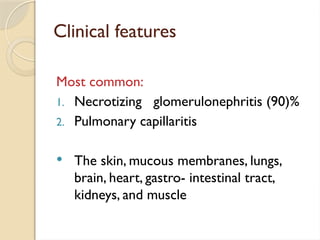
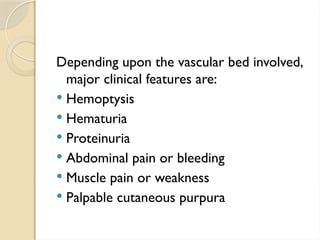
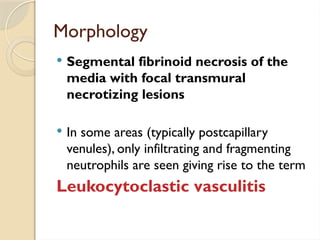
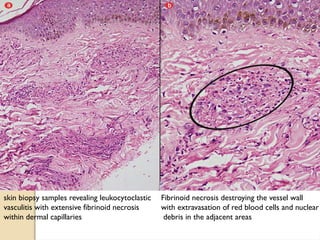
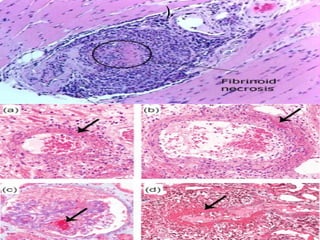
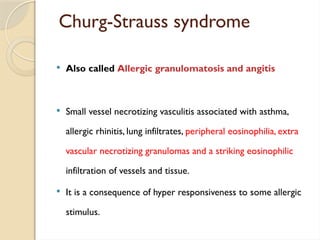
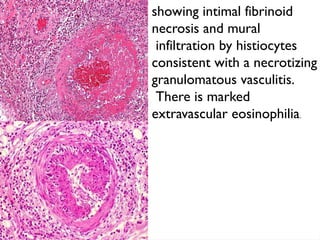
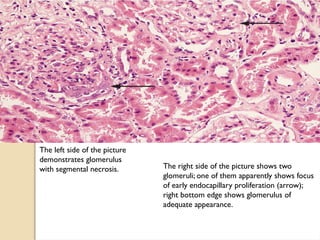
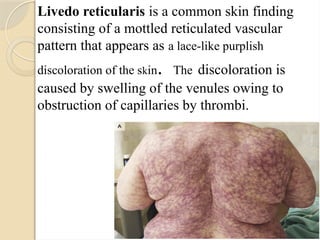
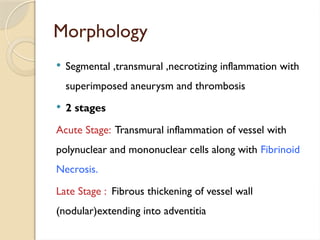
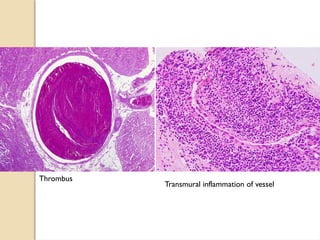
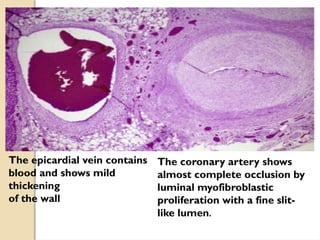
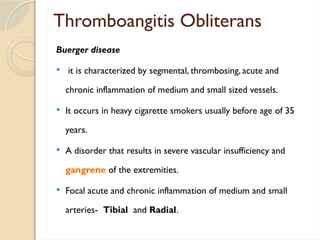
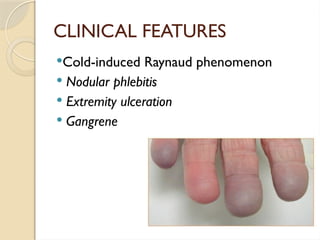
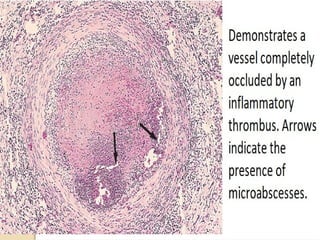
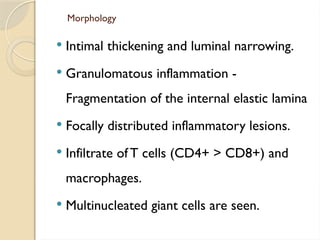
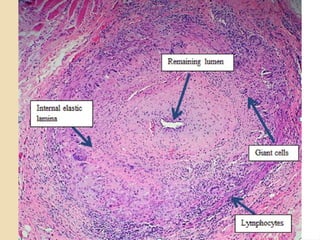
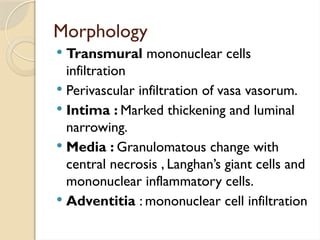
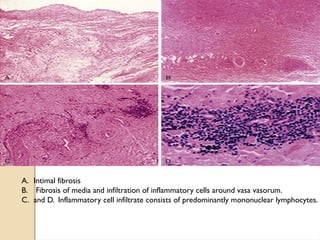
The document provides a detailed overview of vasculitis, including the structure of blood vessels and the various forms of vessel inflammation, characterized by immune-mediated damage or infectious pathogens. It classifies vasculitis based on vessel size, site, histology, and pathogenesis, discussing specific types such as granulomatosis with polyangiitis and polyarteritis nodosa, along with their clinical presentations and diagnostic approaches. Additionally, it highlights the roles of immune complexes, ANCA-mediated responses, and the involvement of various pathogens in the development of vasculitis.