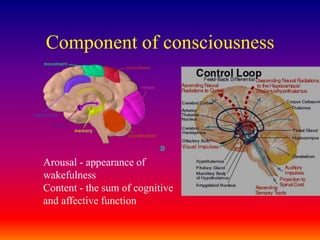
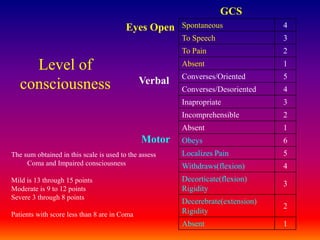
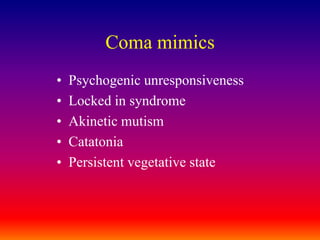
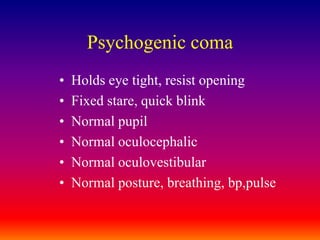
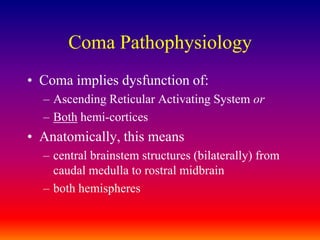
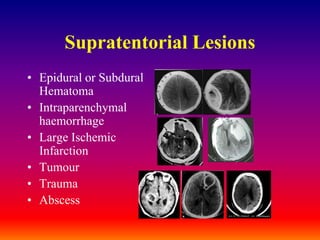
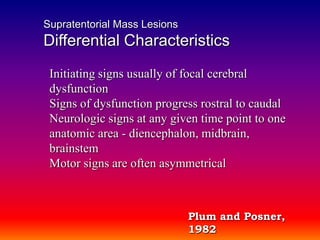
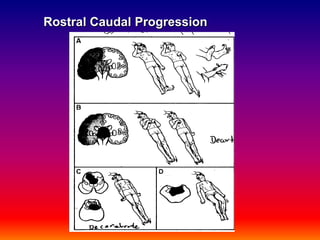
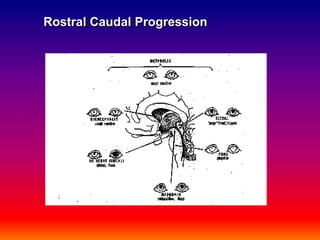
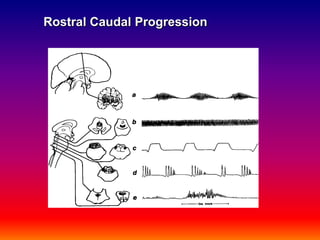
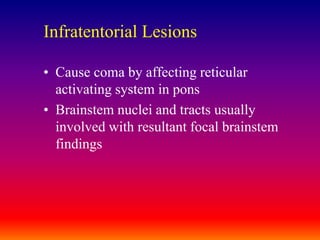
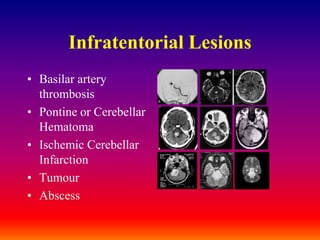
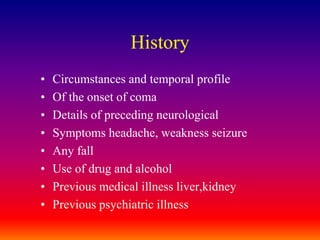
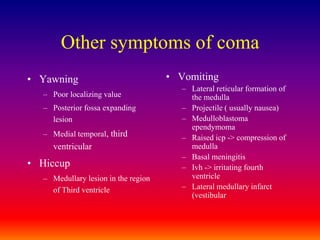
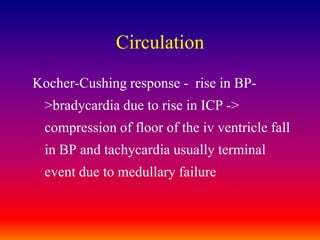
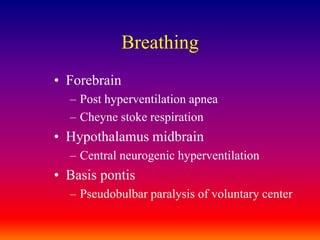
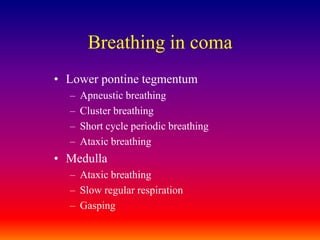
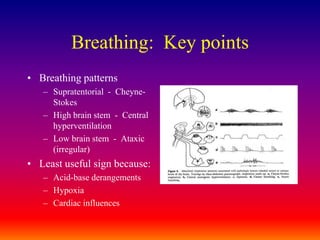
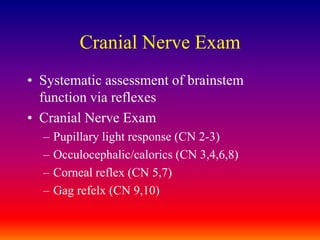
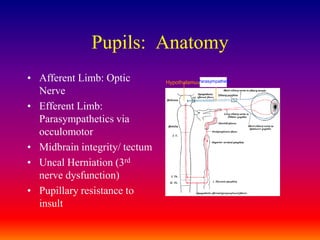
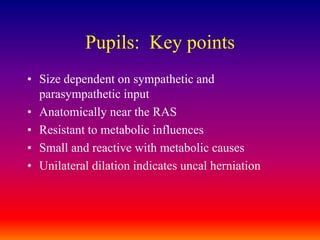
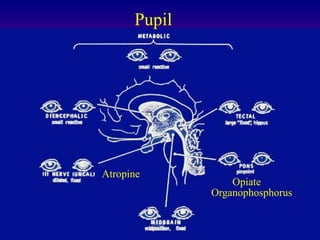
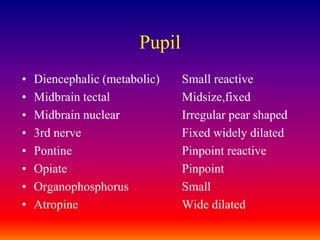
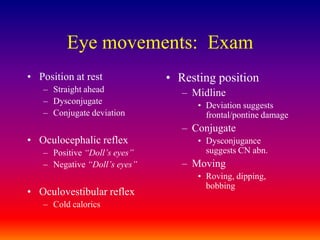
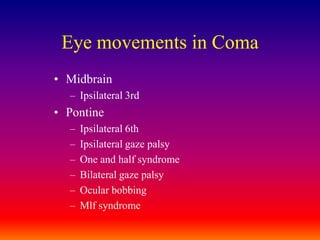
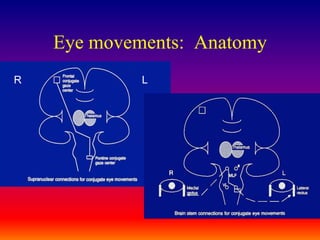
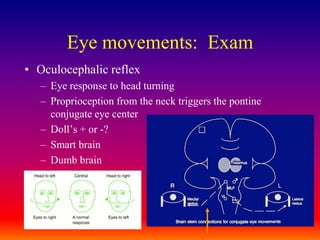
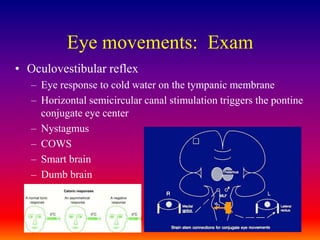
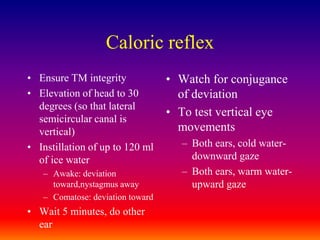
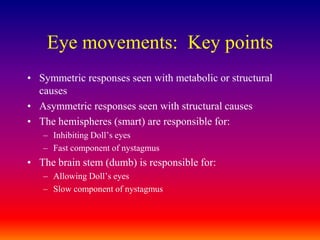
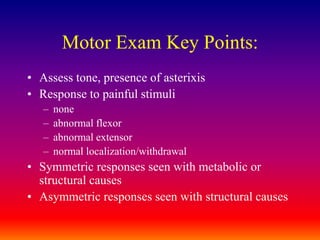
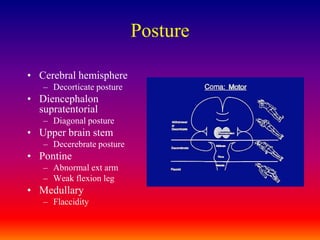
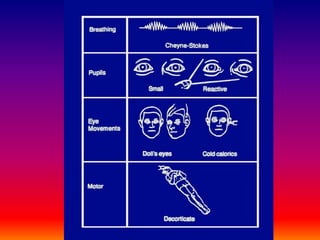
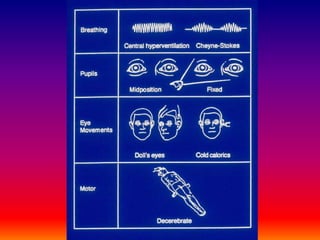
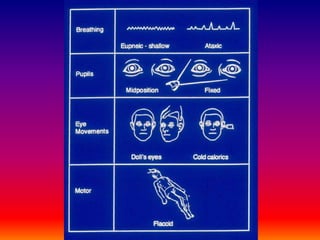
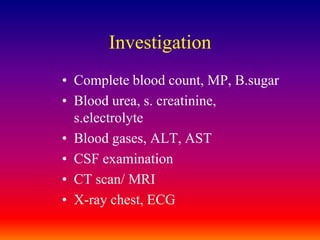
The document provides guidance on approaching and managing a comatose patient. It outlines that the primary objectives are to stabilize, evaluate, and treat the patient by taking an organized sequential approach that prioritizes the airway, breathing, circulation, treating metabolic causes of coma like hypoglycemia, and evaluating for increased intracranial pressure or mass lesions. Secondary objectives include understanding the signs and symptoms of different causes of coma and developing a differential diagnosis. The document then provides detailed information on assessing different aspects of the comatose patient including their level of consciousness, neurological exam findings, breathing patterns, eye movements, motor response, and appropriate investigations.