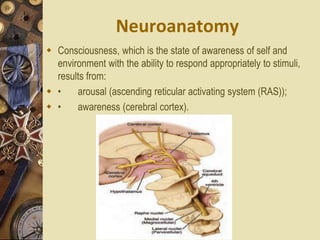
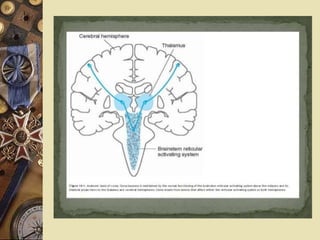
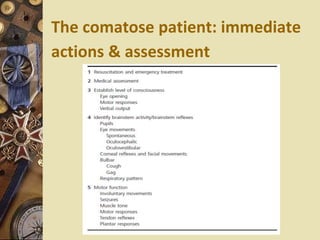
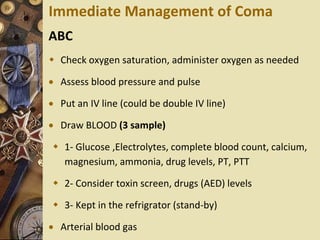
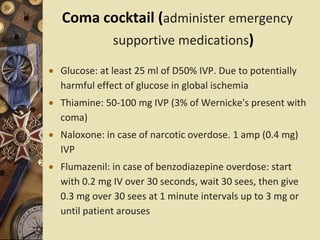
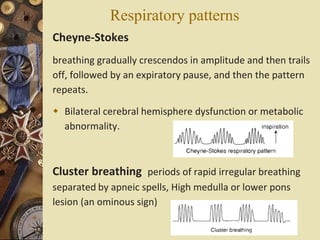
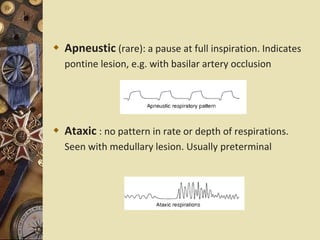
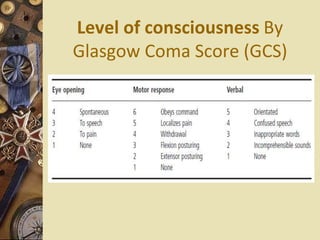
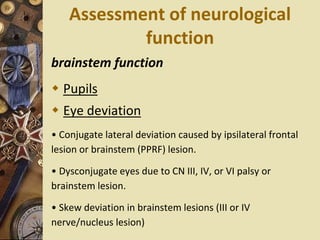
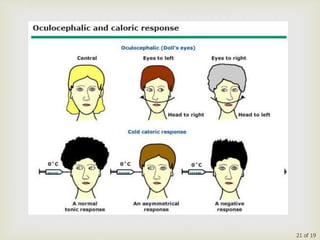
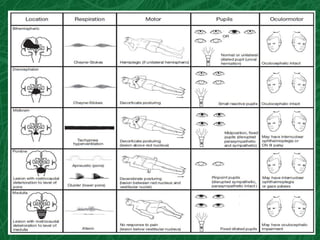
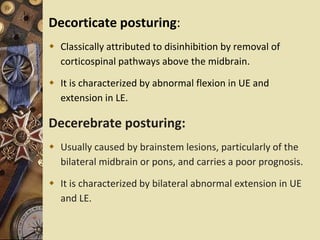
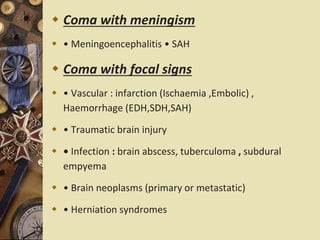
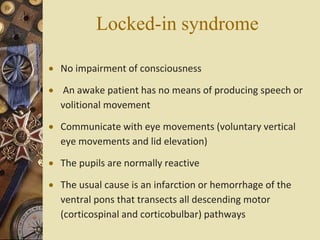
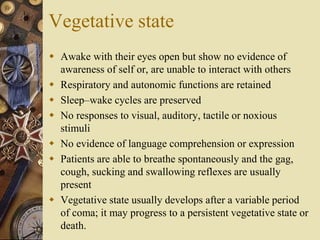
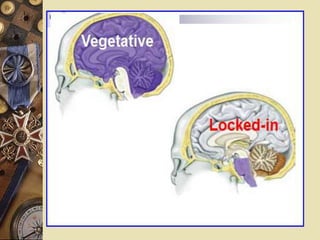
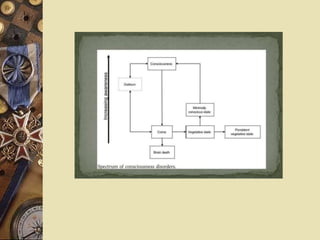
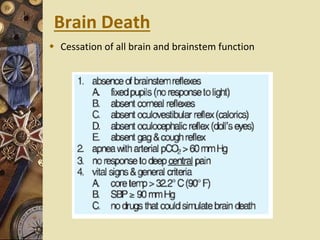
This document provides information about coma, including its neuroanatomical basis, causes, definitions of related states, assessment, and differential diagnosis. Coma results from dysfunction of the brainstem reticular activating system, thalamus, or diffuse lesions in both cerebral hemispheres. Immediate management of coma involves assessing ABCs and administering supportive medications. A thorough neurological exam evaluates level of consciousness, brainstem reflexes, motor function, and more to localize lesions and distinguish structural from toxic/metabolic causes. Pseudocoma conditions like locked-in syndrome or catatonia can mimic true coma and require different management.