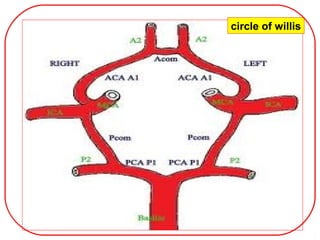
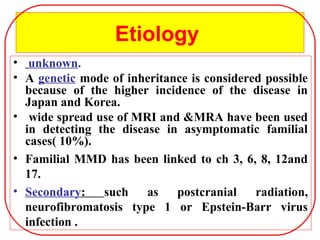
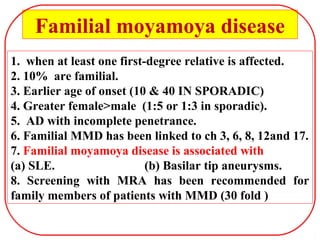
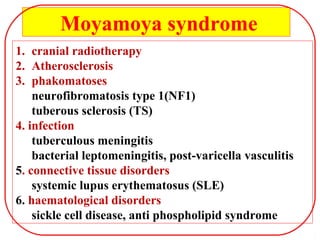
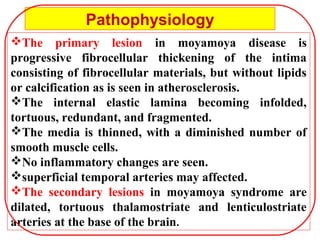
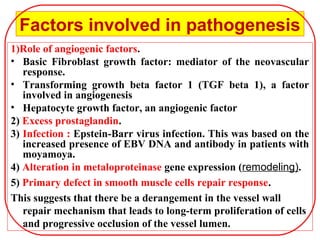
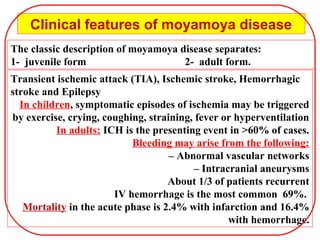
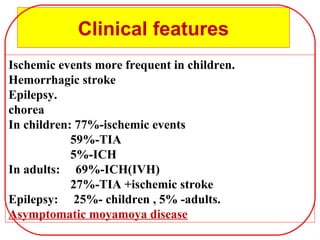
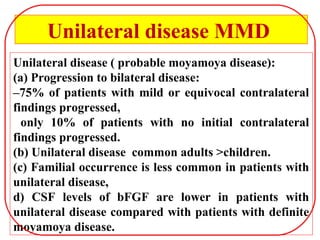
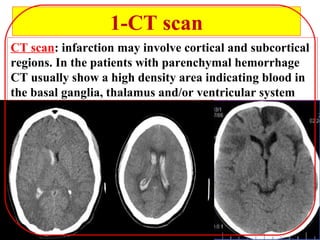
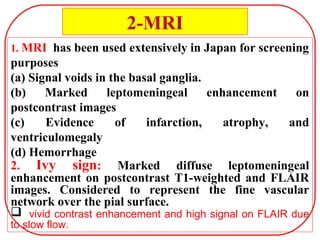
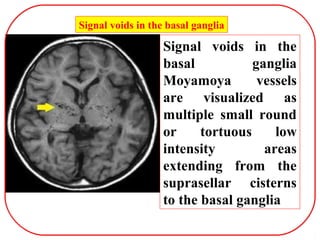
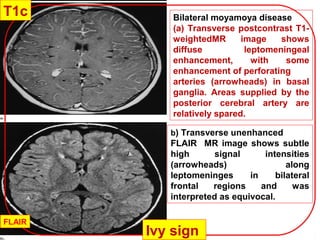
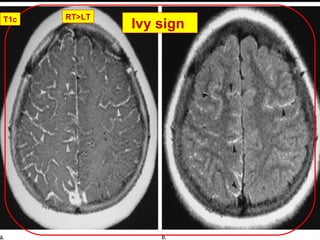
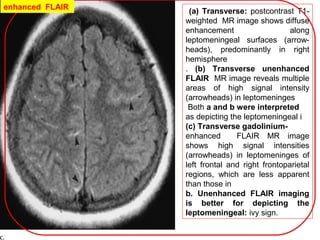
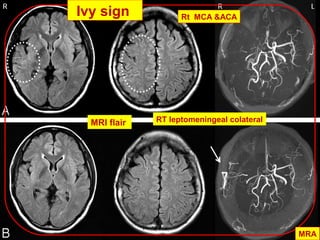
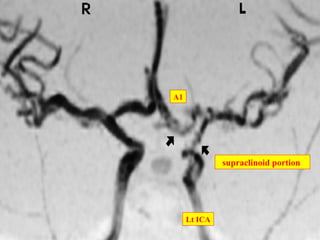
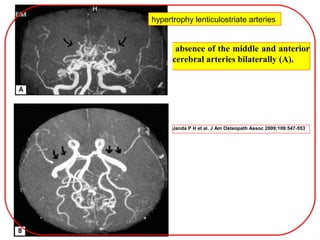
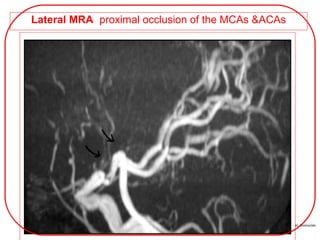
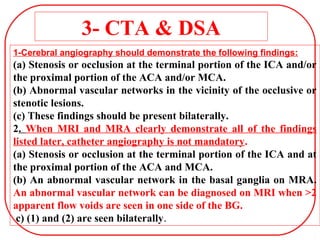
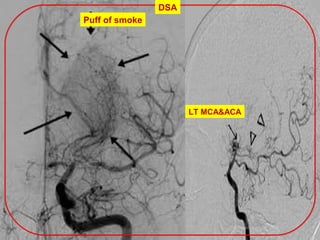
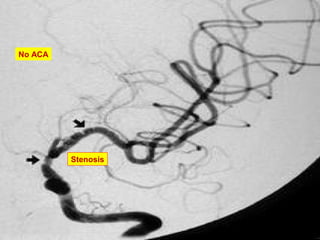
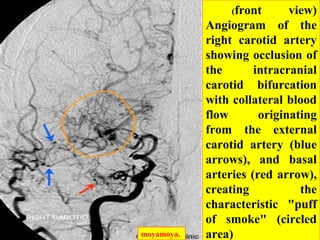
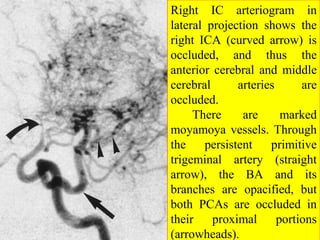
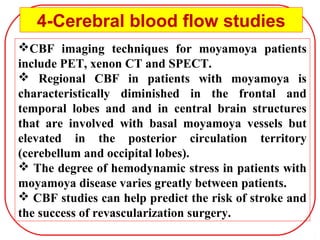
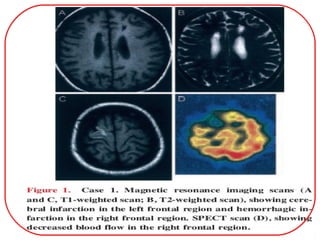
This document provides an overview of Moyamoya disease. It defines Moyamoya disease as a progressive stenosis of the intracranial arteries, typically the internal carotid arteries and proximal middle and anterior cerebral arteries, accompanied by a compensatory network of collaterals at the brain's base. The cause is unknown but genetic factors are believed to play a role. Clinically, it can present with transient ischemic attacks, strokes, or hemorrhage. Diagnosis is based on neuroimaging findings on MRI, MRA, CTA or DSA showing the characteristic vascular changes. Treatment involves medical management as well as surgical revascularization procedures. Prognosis depends on the extent of vascular involvement and collateral formation.