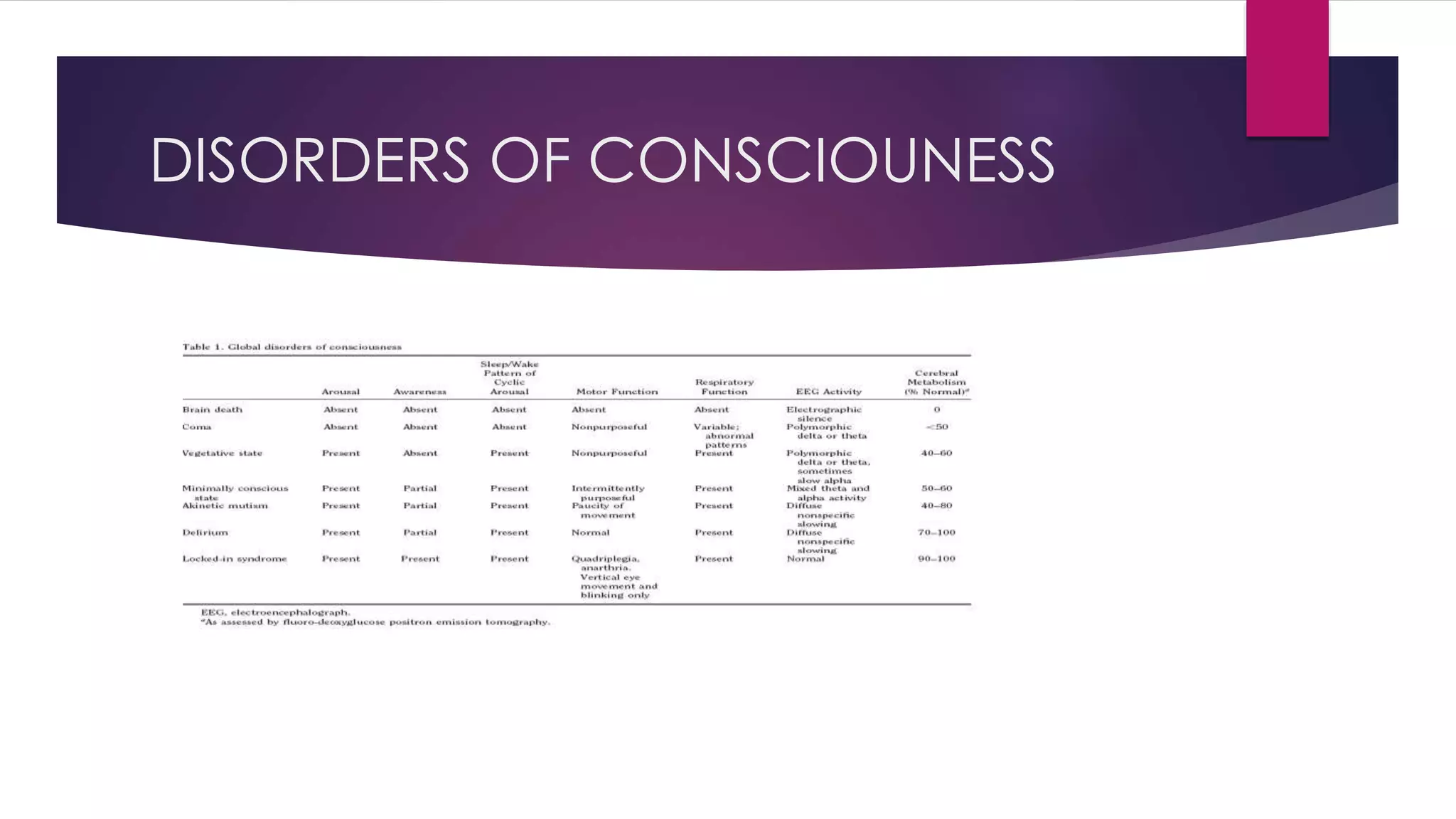
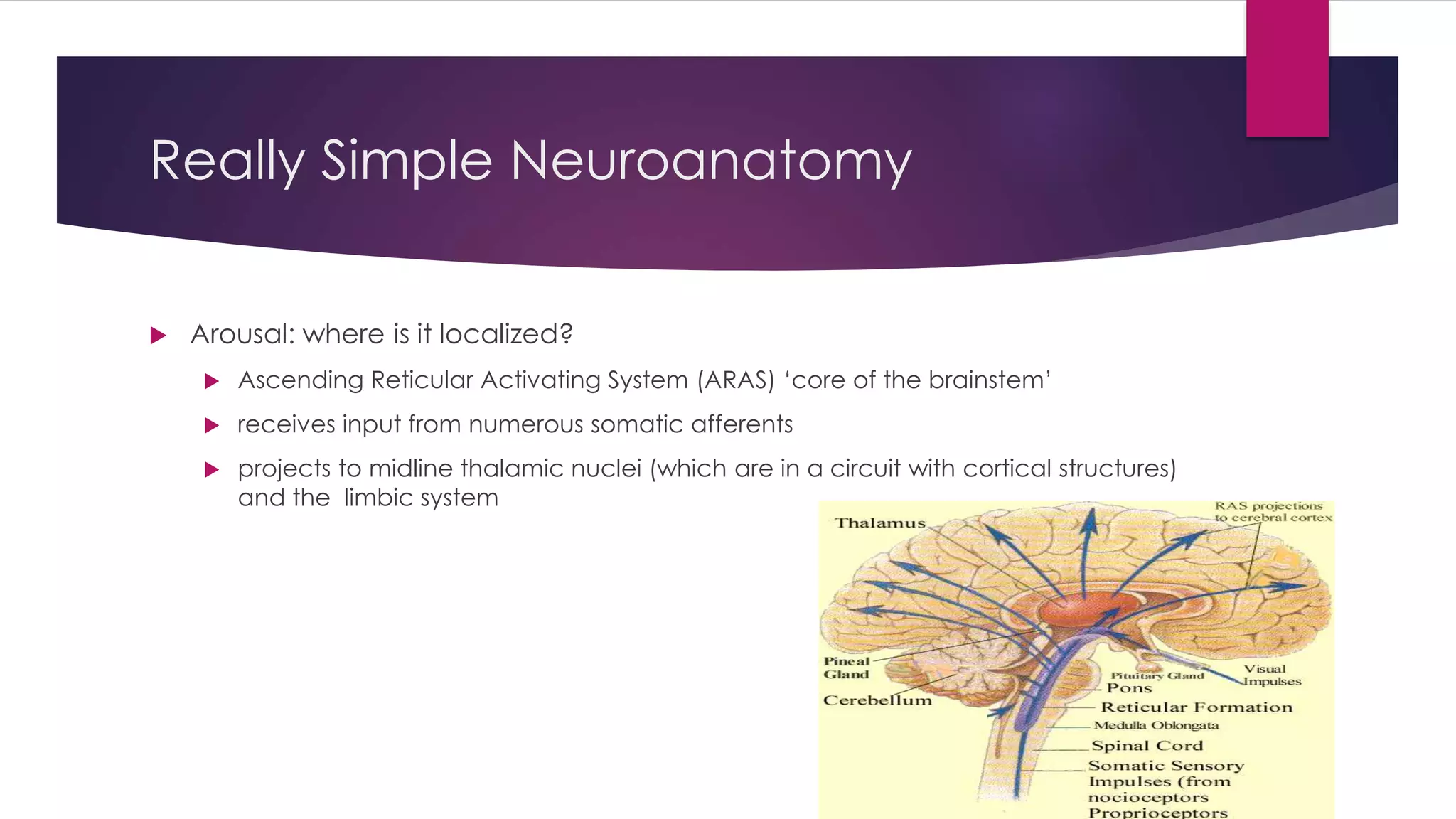
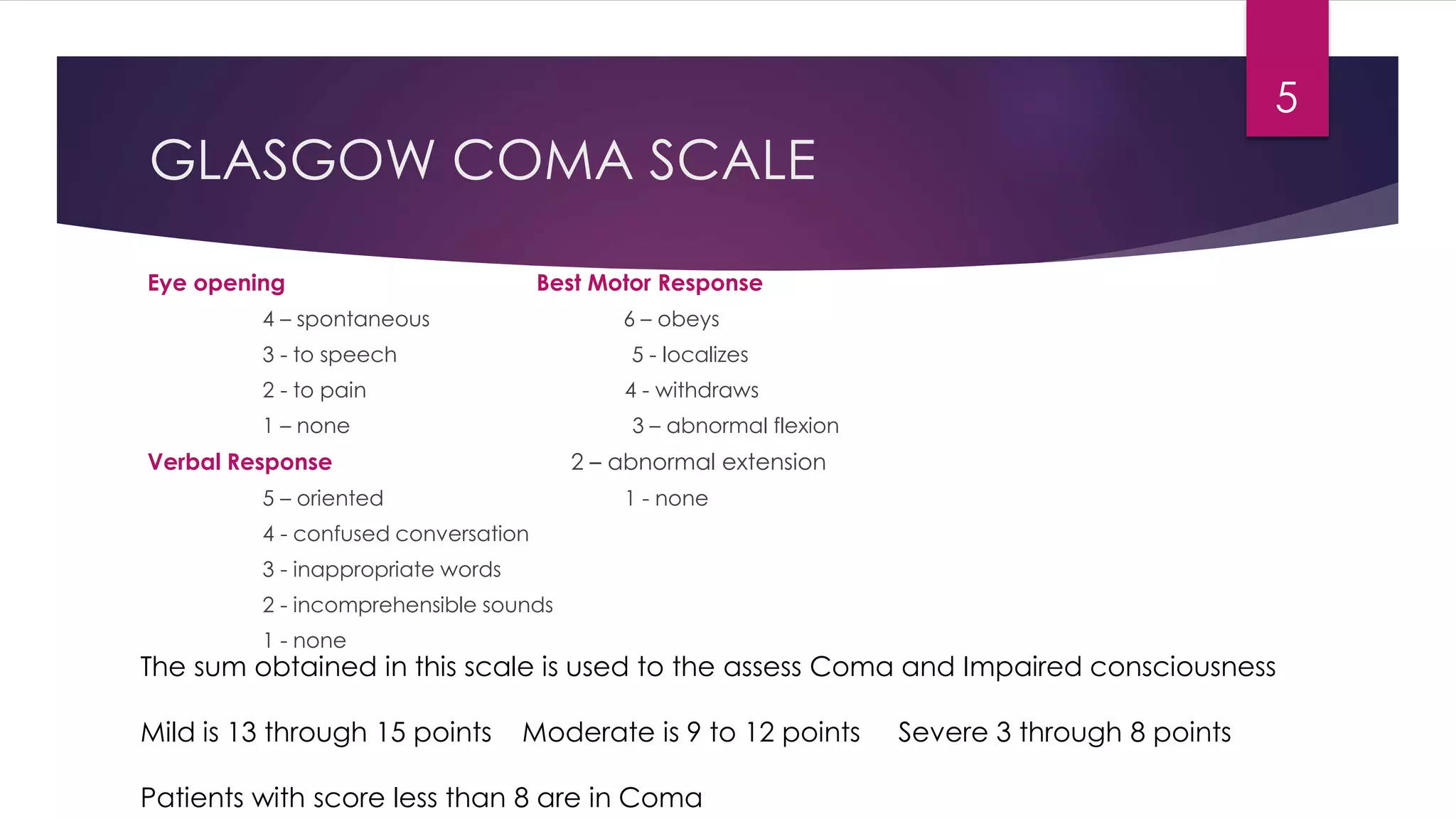
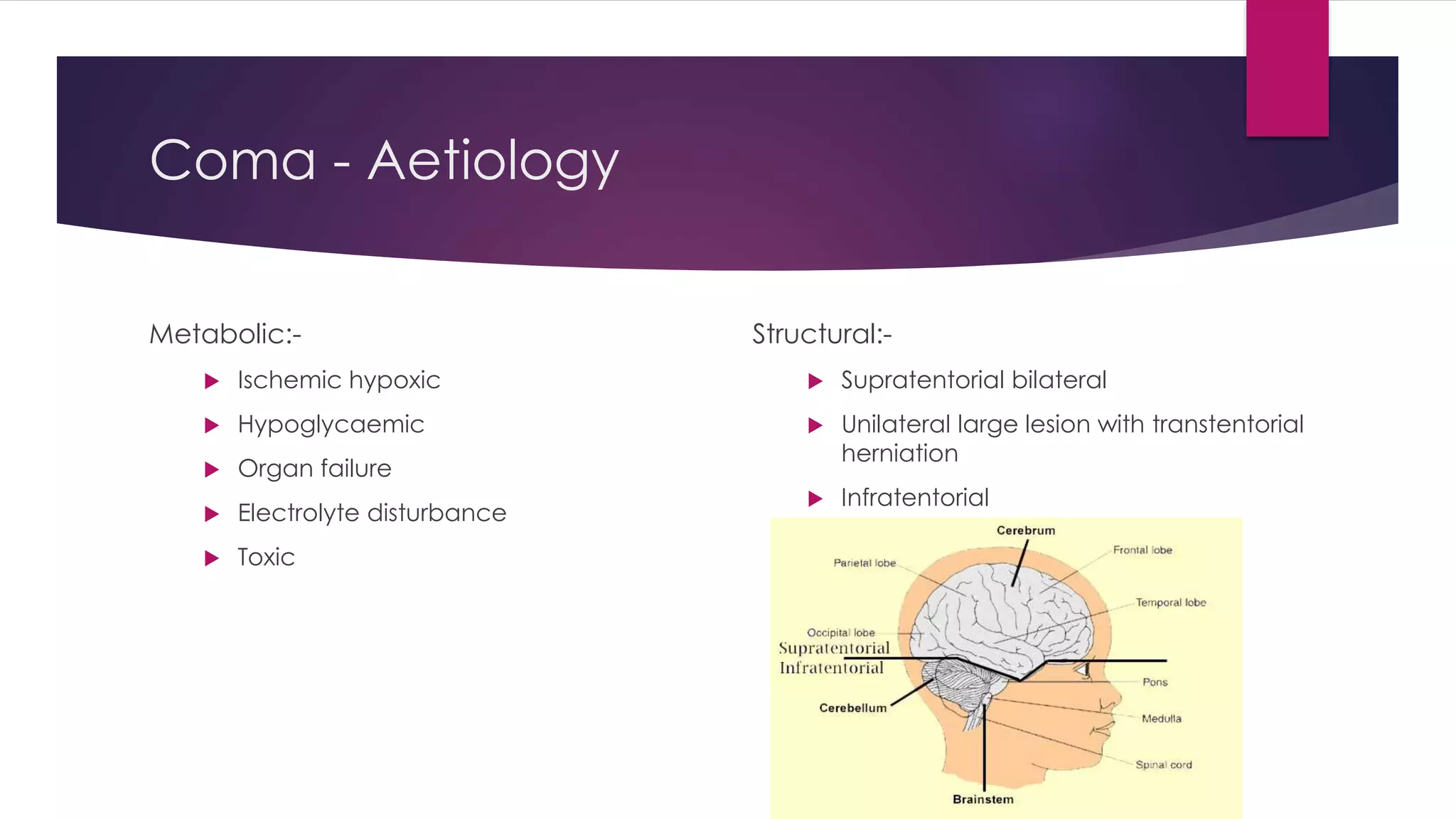
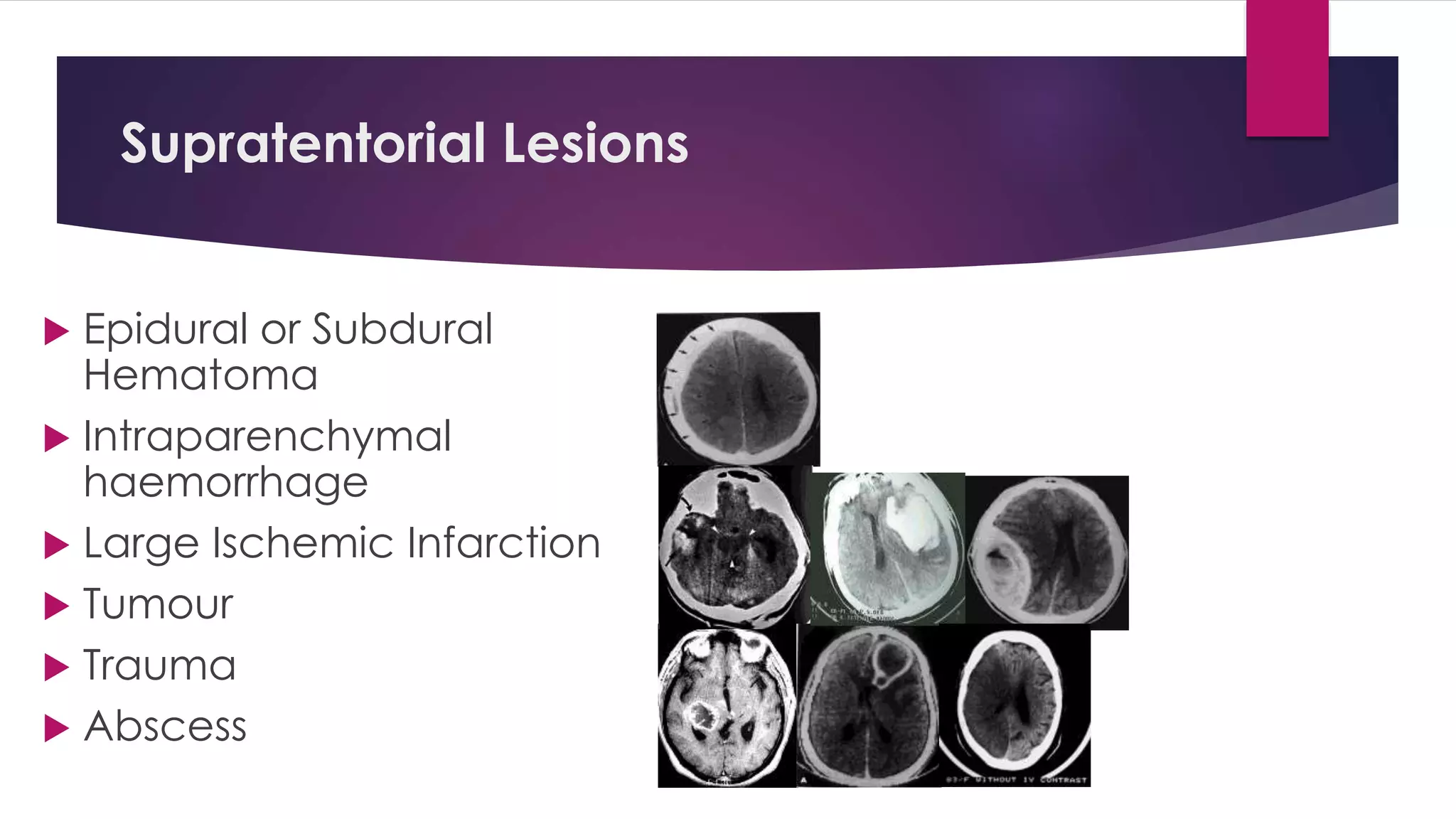
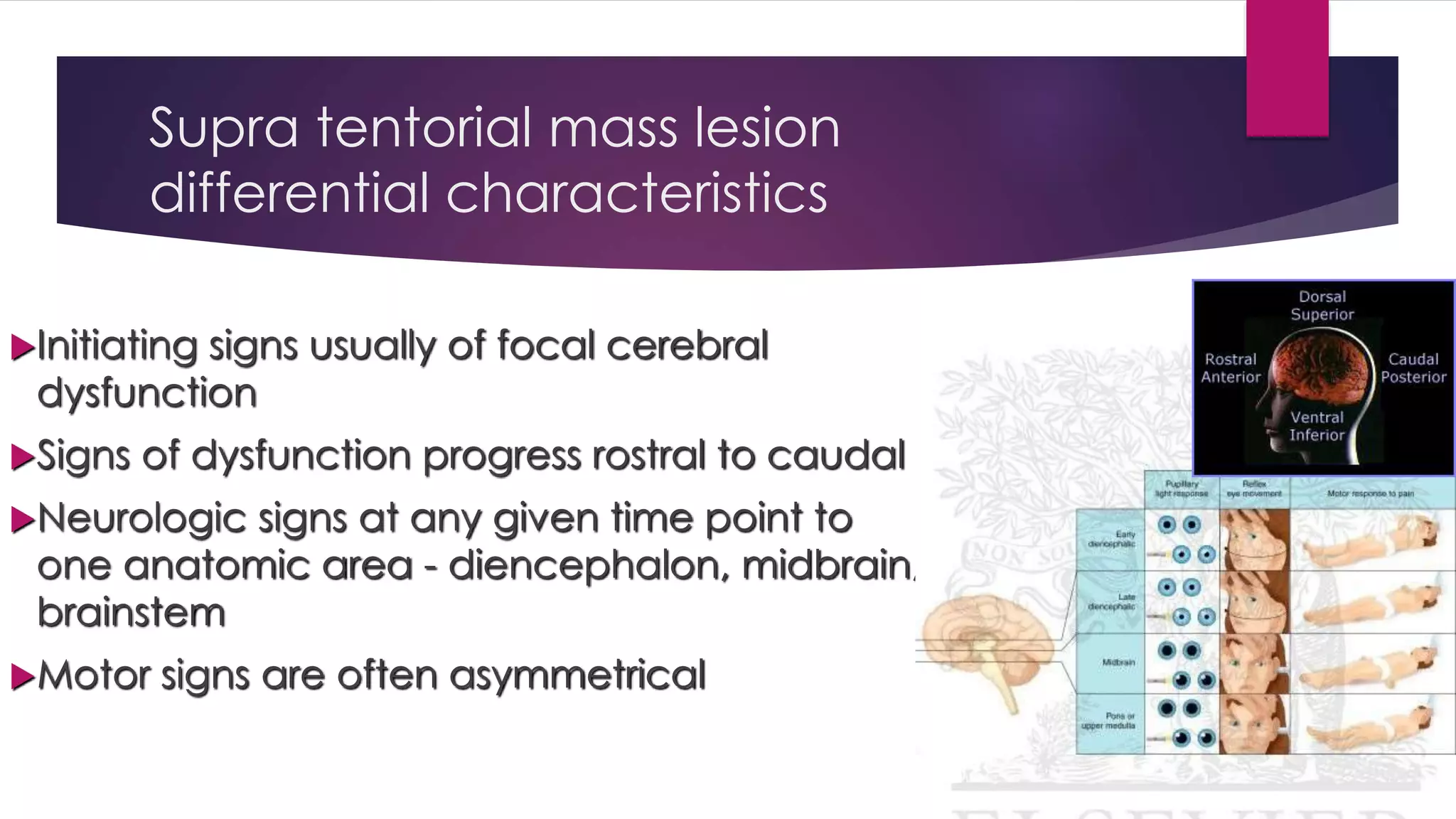
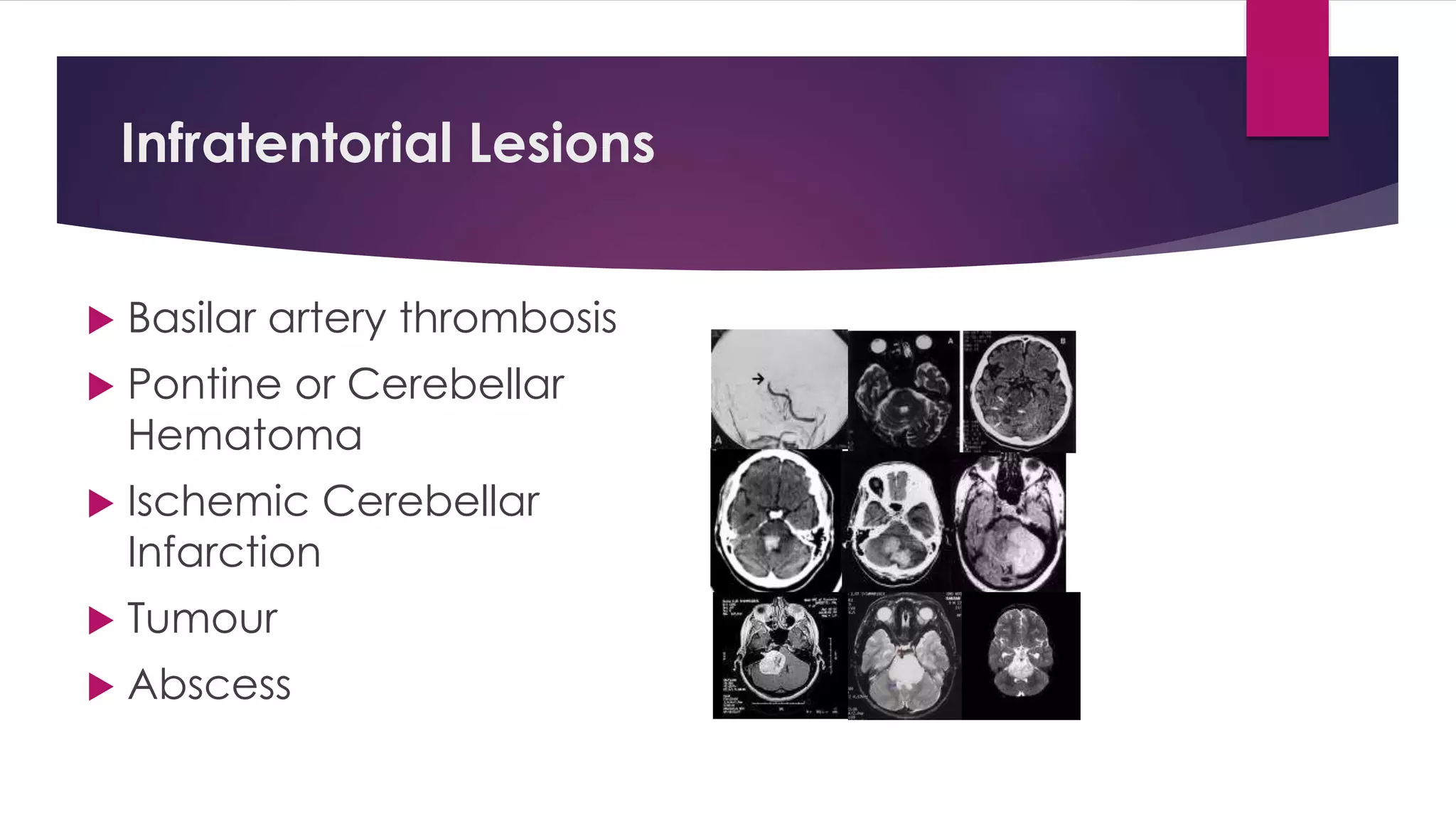
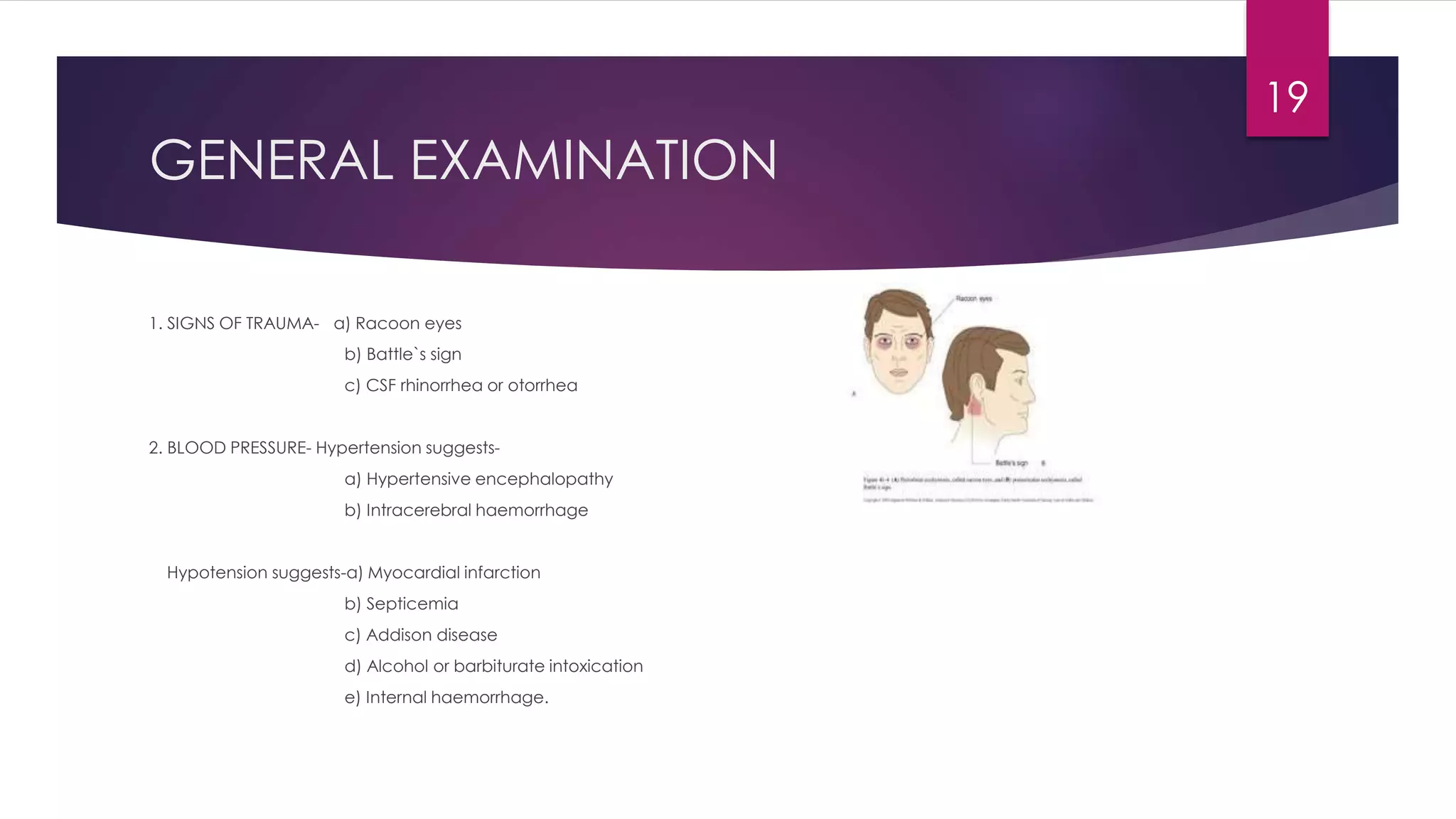
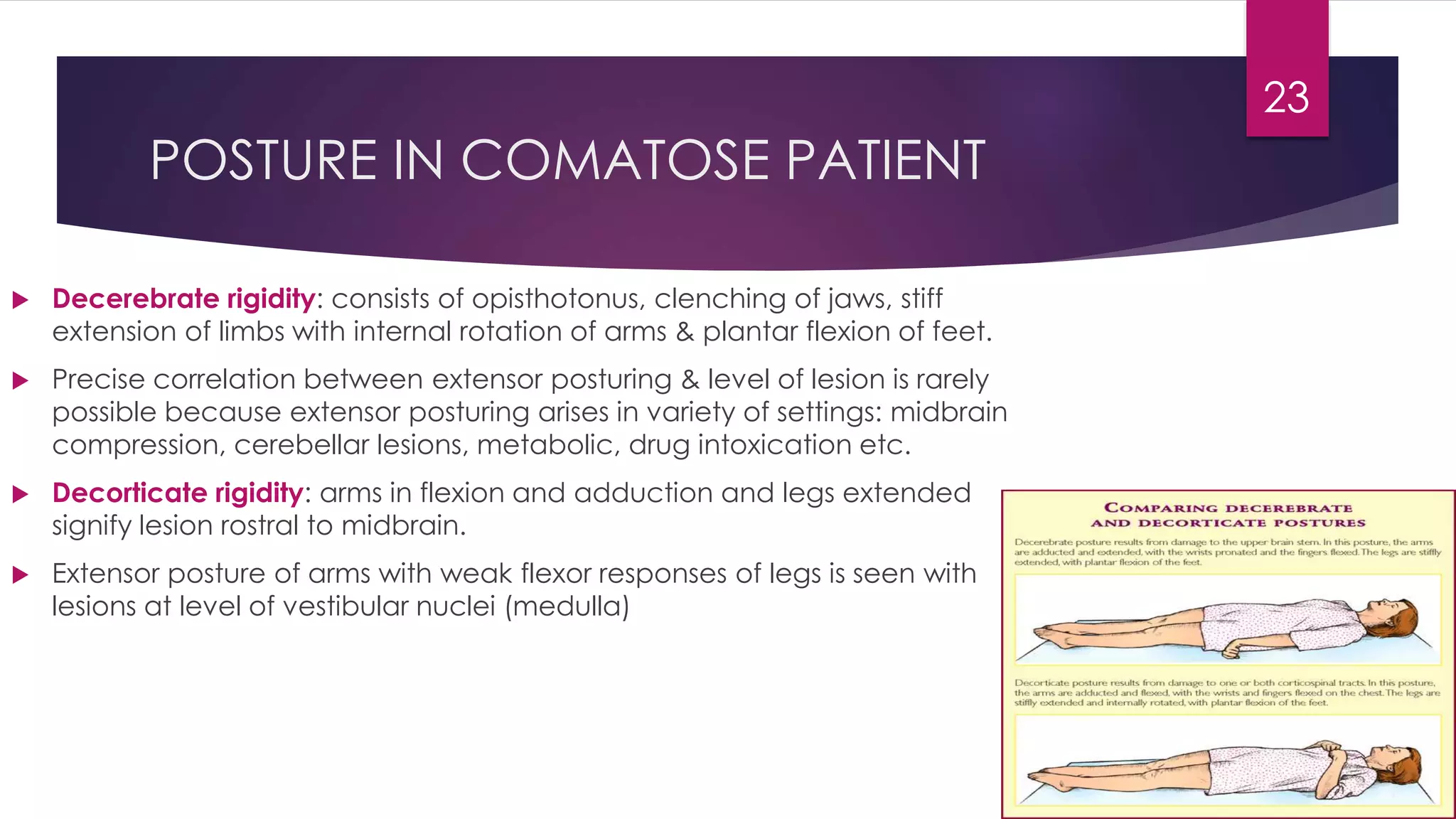
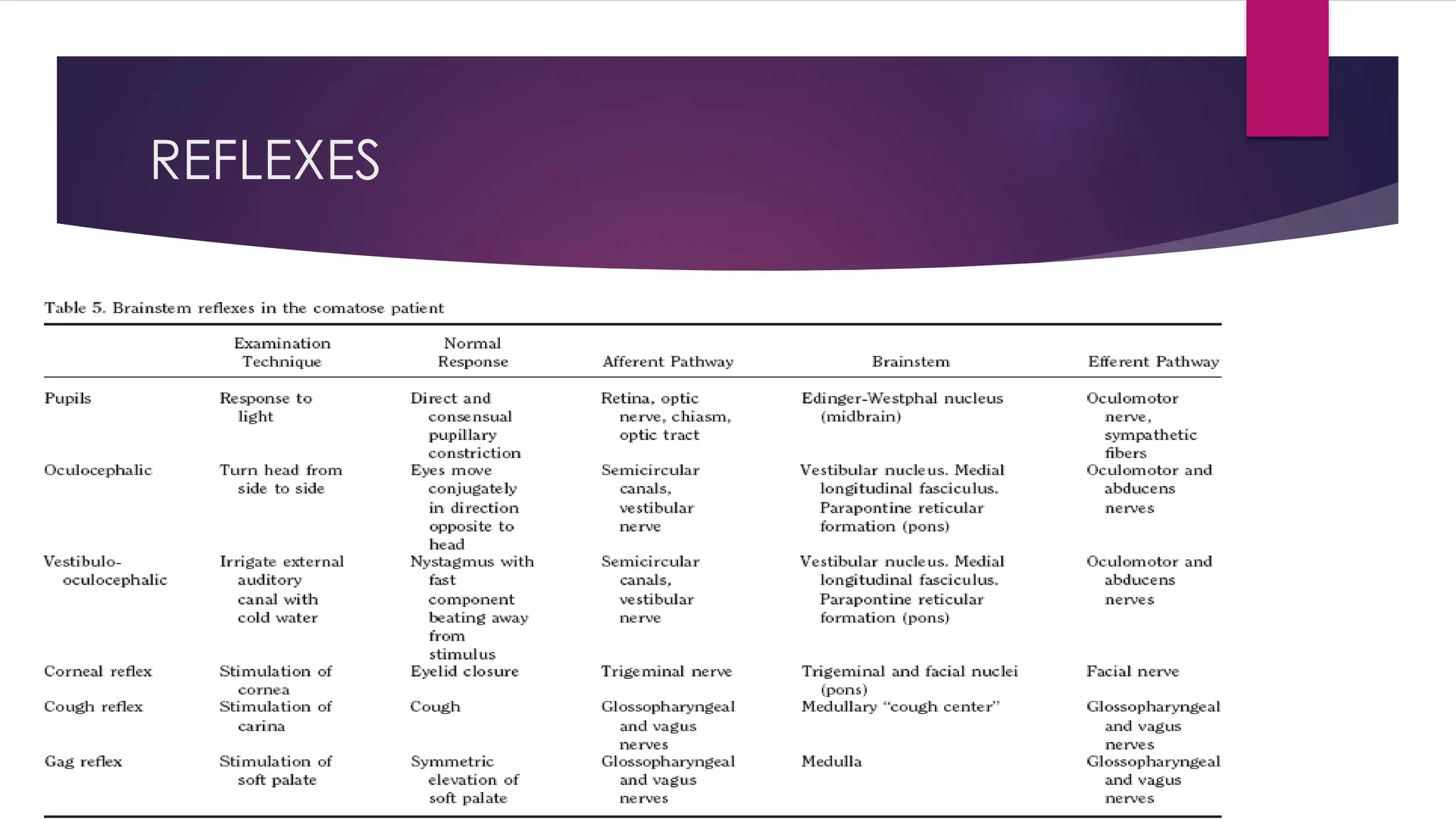
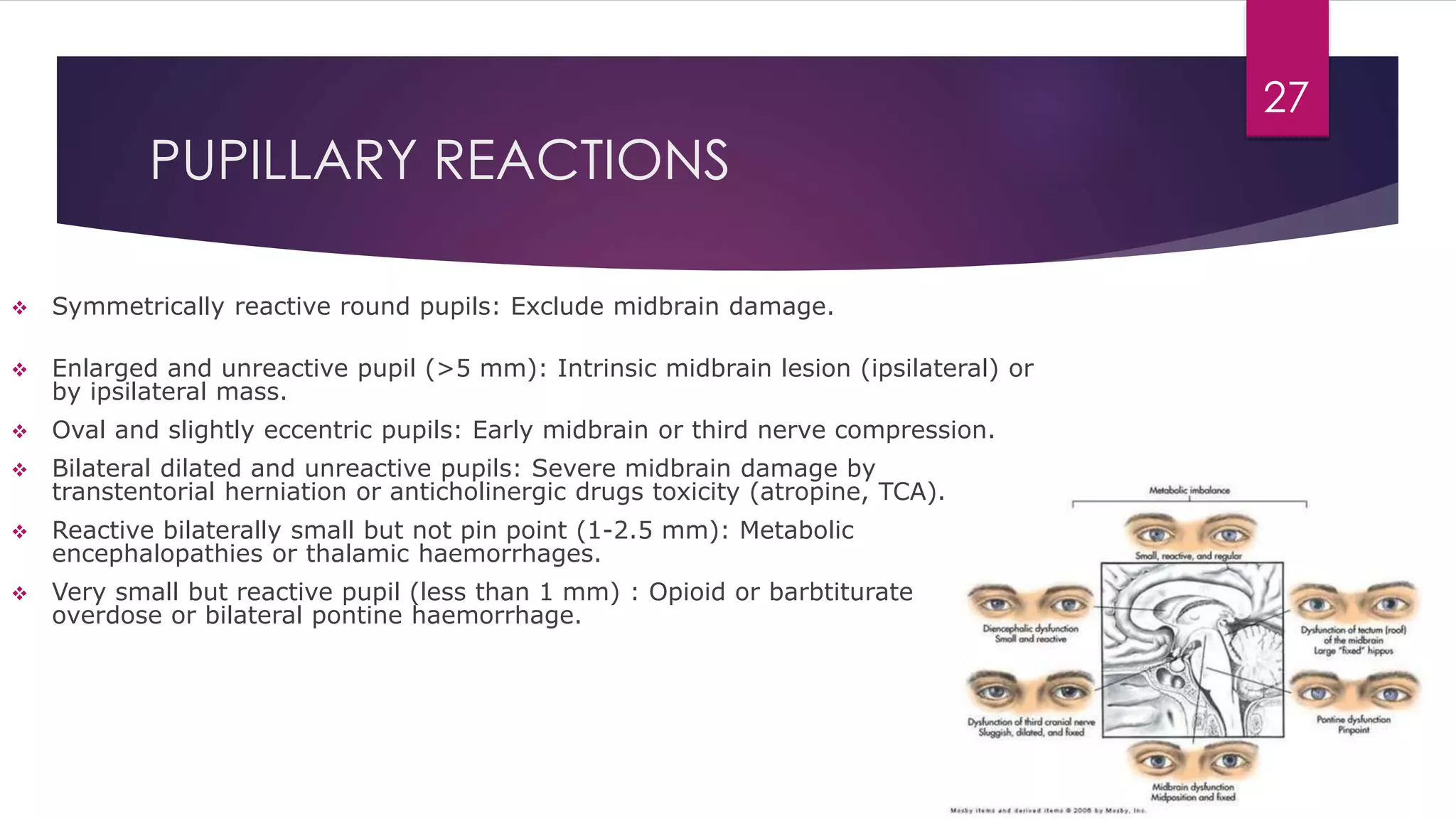
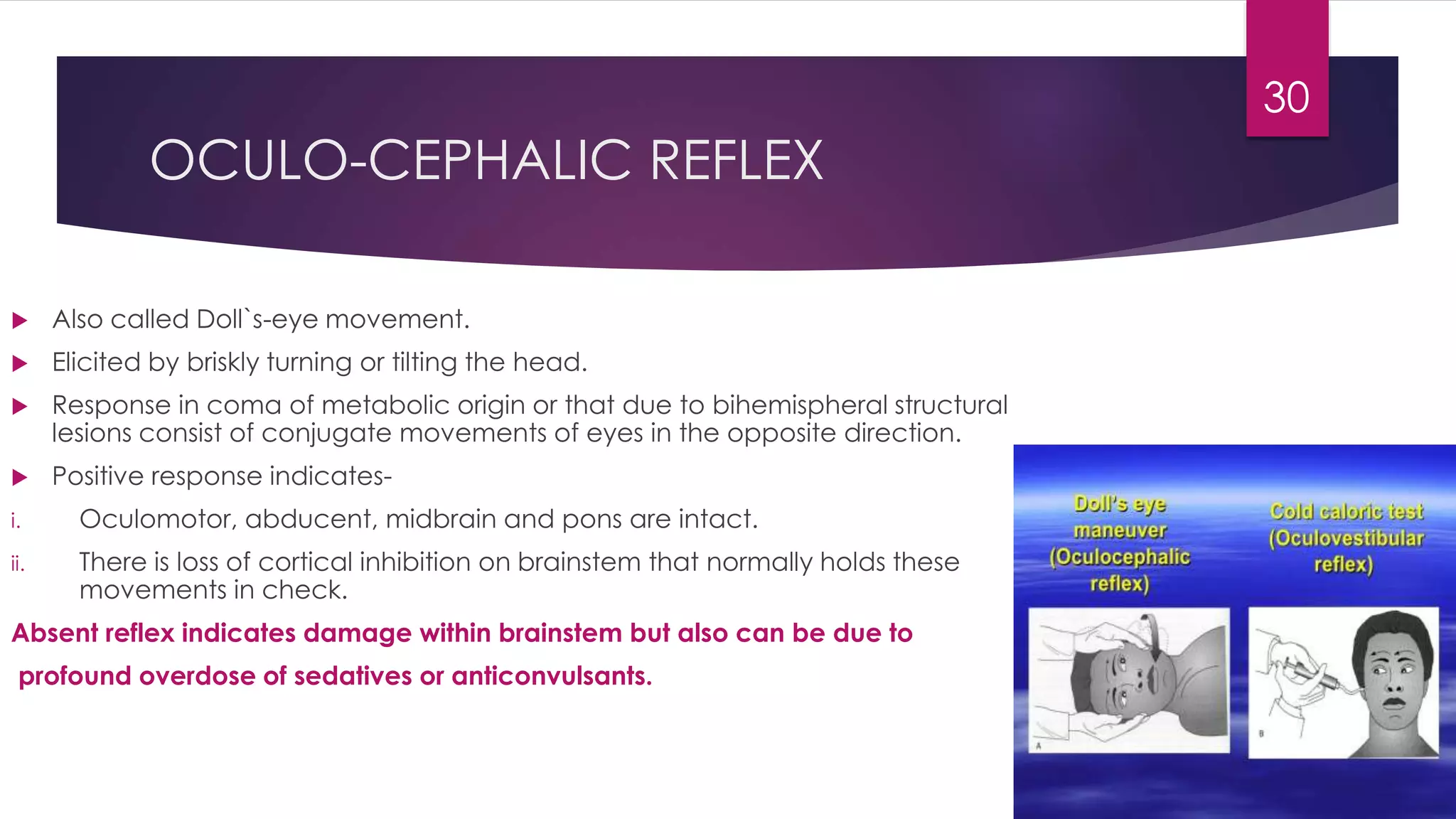
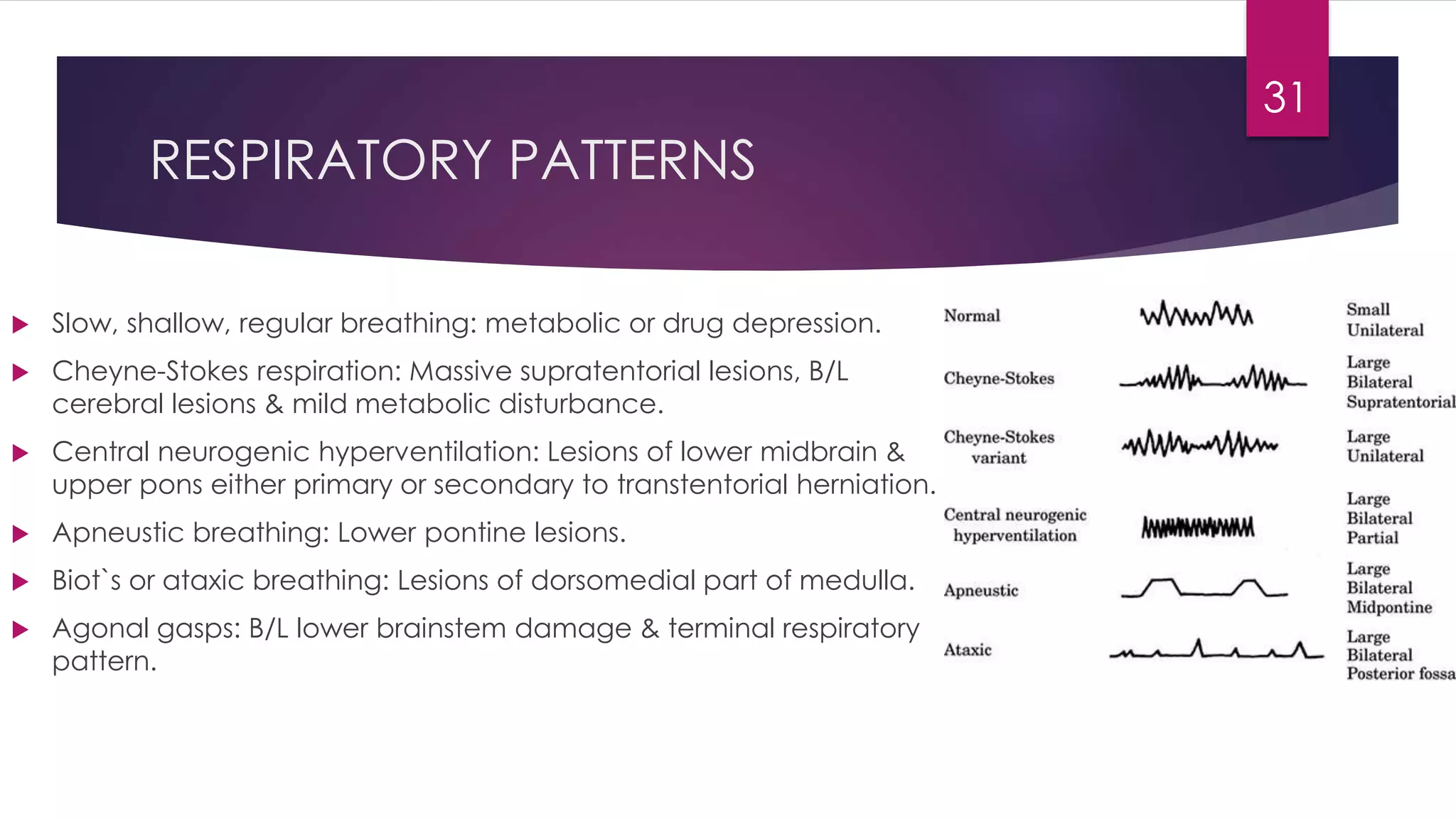
This document discusses the evaluation and management of coma. It begins by defining coma as prolonged unresponsiveness. It then describes the anatomy of arousal centered around the ascending reticular activating system. Assessment of coma involves the Glasgow Coma Scale and examining for signs of increased intracranial pressure. Common causes of coma include metabolic derangements, structural lesions of the brainstem or supratentorial regions. Management involves stabilizing ventilation, circulation, controlling seizures, reducing intracranial pressure and maintaining temperature. Detailed neurological examination can help localize lesions through assessment of reflexes, eye movements, respiratory patterns and posture.