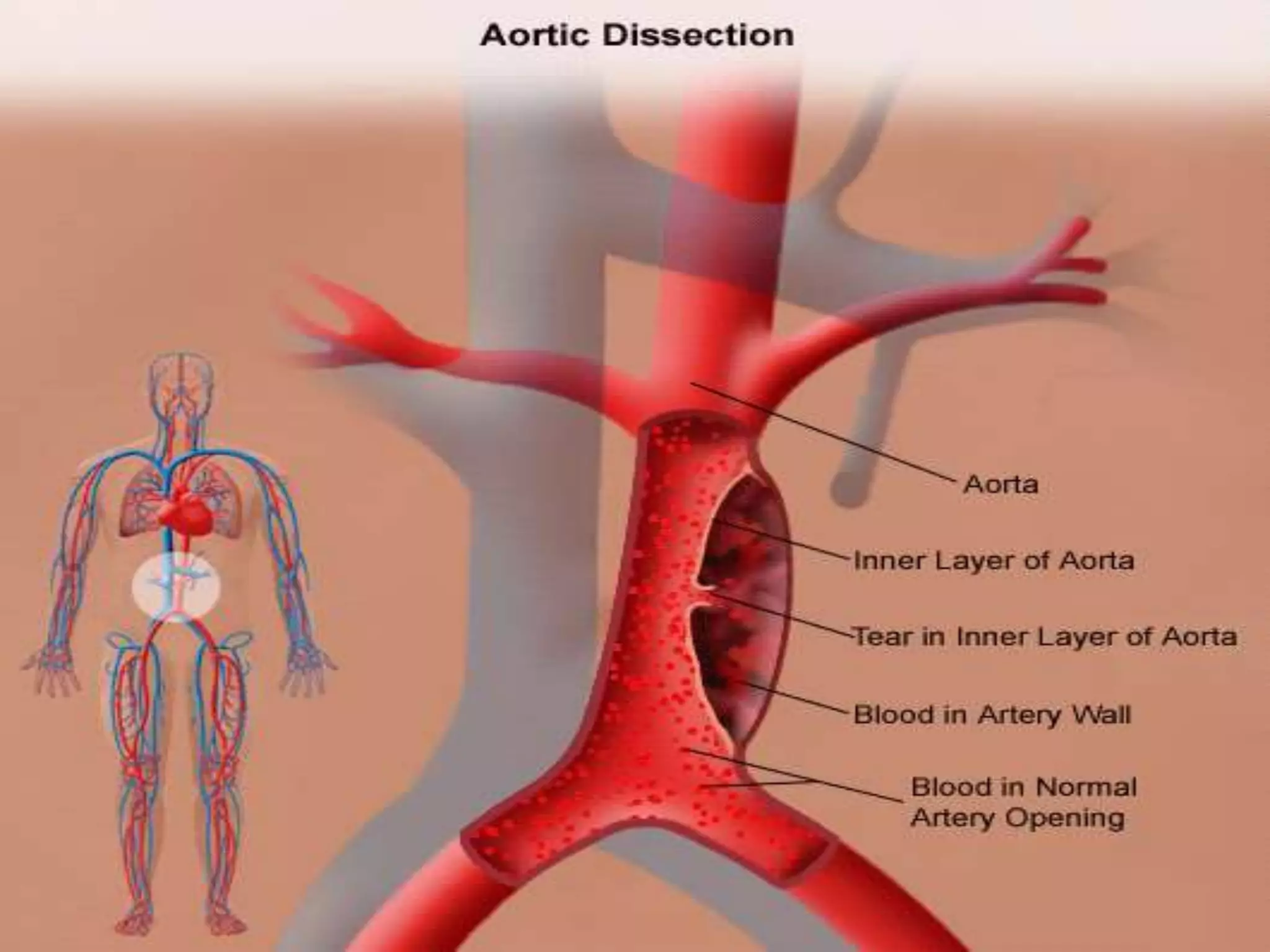
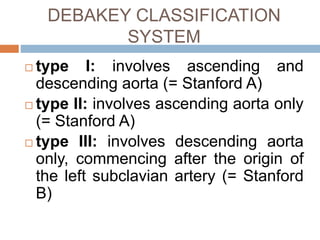
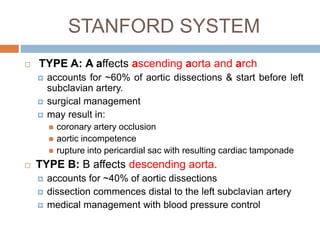
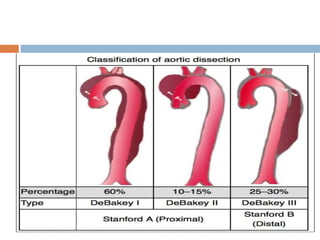
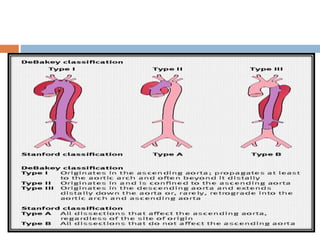
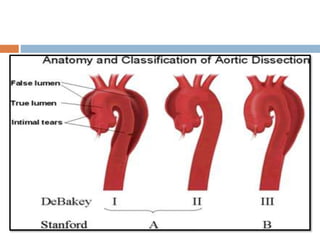
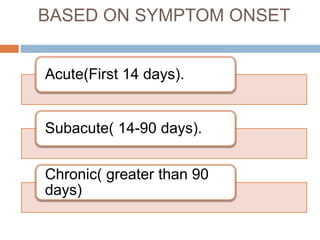
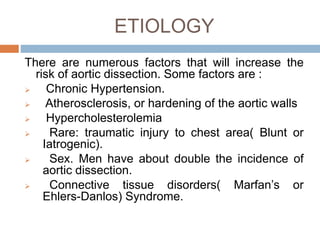
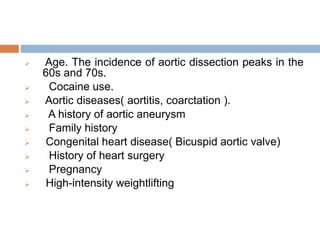
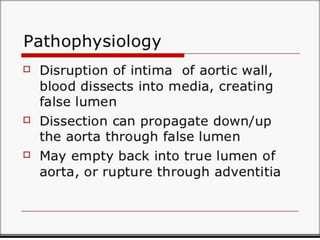
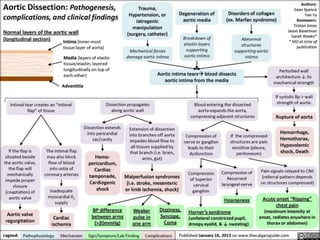
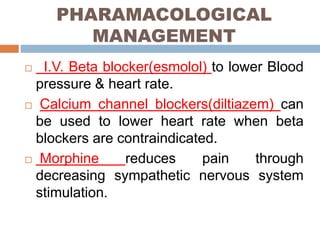
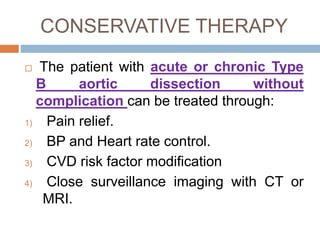
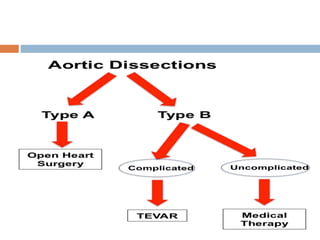
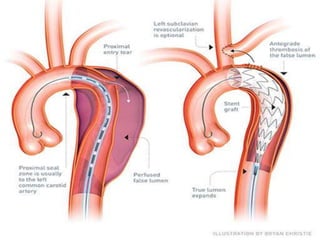
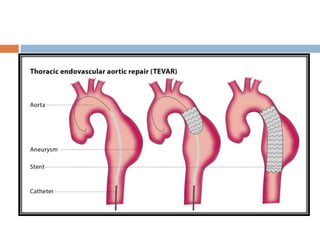
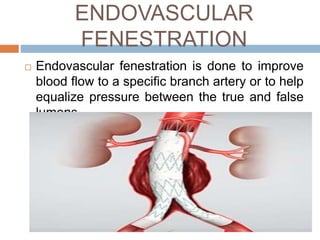
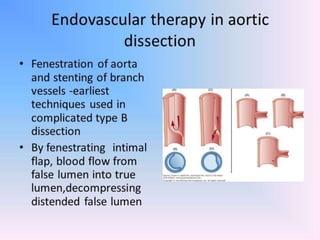
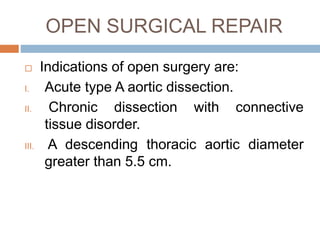
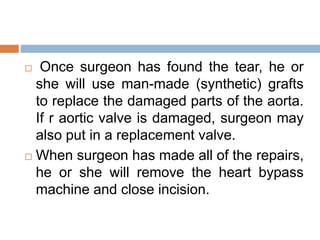
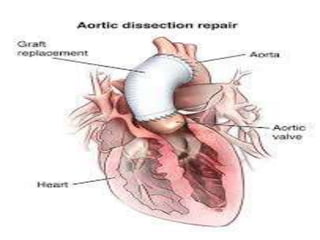
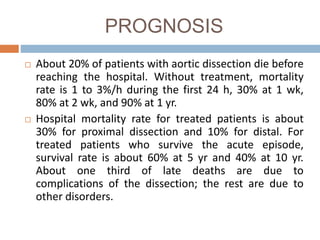
An aortic dissection occurs when blood tears the inner layer of the aorta, separating it from the middle layer. It is classified by location and timing of symptoms. Risk factors include hypertension, connective tissue disorders, and family history. Treatment depends on location but may include surgery, endovascular stent grafting, or medical management of blood pressure. Prognosis depends on type and treatment, with mortality rates declining with advances in surgical and endovascular techniques.