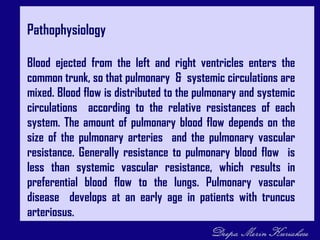
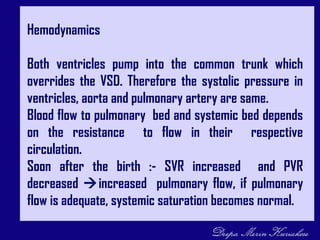
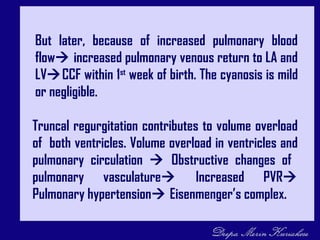
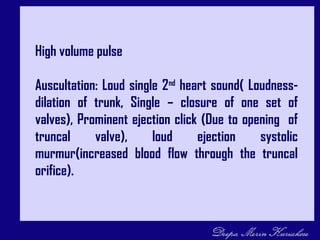
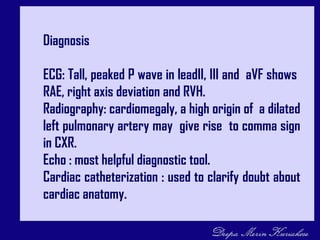
Truncus arteriosus is a congenital heart defect where there is a single arterial trunk exiting the heart, giving rise to the pulmonary artery, aorta, and coronary arteries. This occurs when normal septation of the embryonic bulbar trunk fails to occur. Blood from the two ventricles mixes in the common trunk, resulting in decreased oxygen levels. Surgical repair is needed to separate pulmonary and systemic blood flow and close the ventricular septal defect. Without repair, complications like congestive heart failure and pulmonary hypertension can develop.