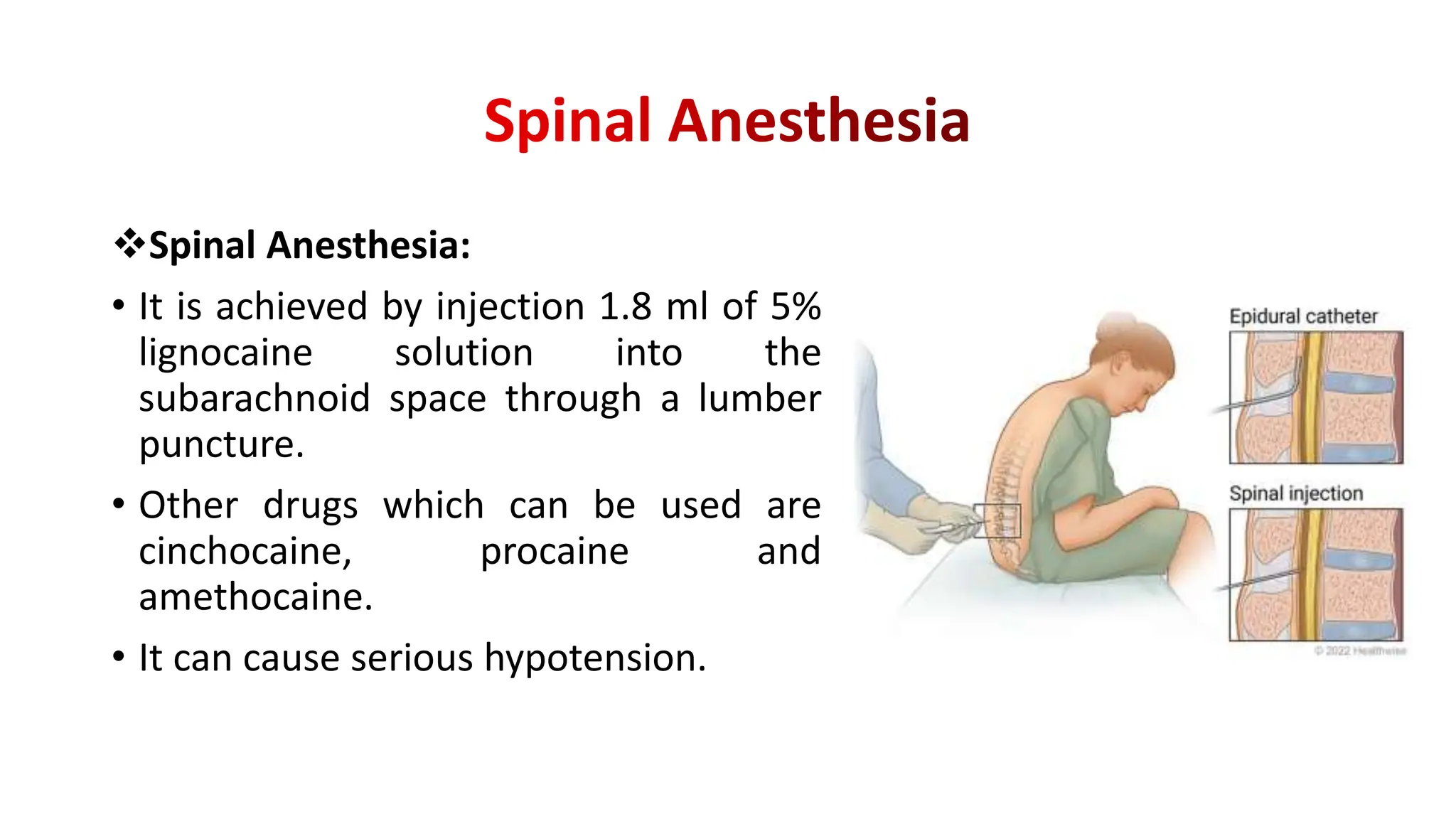
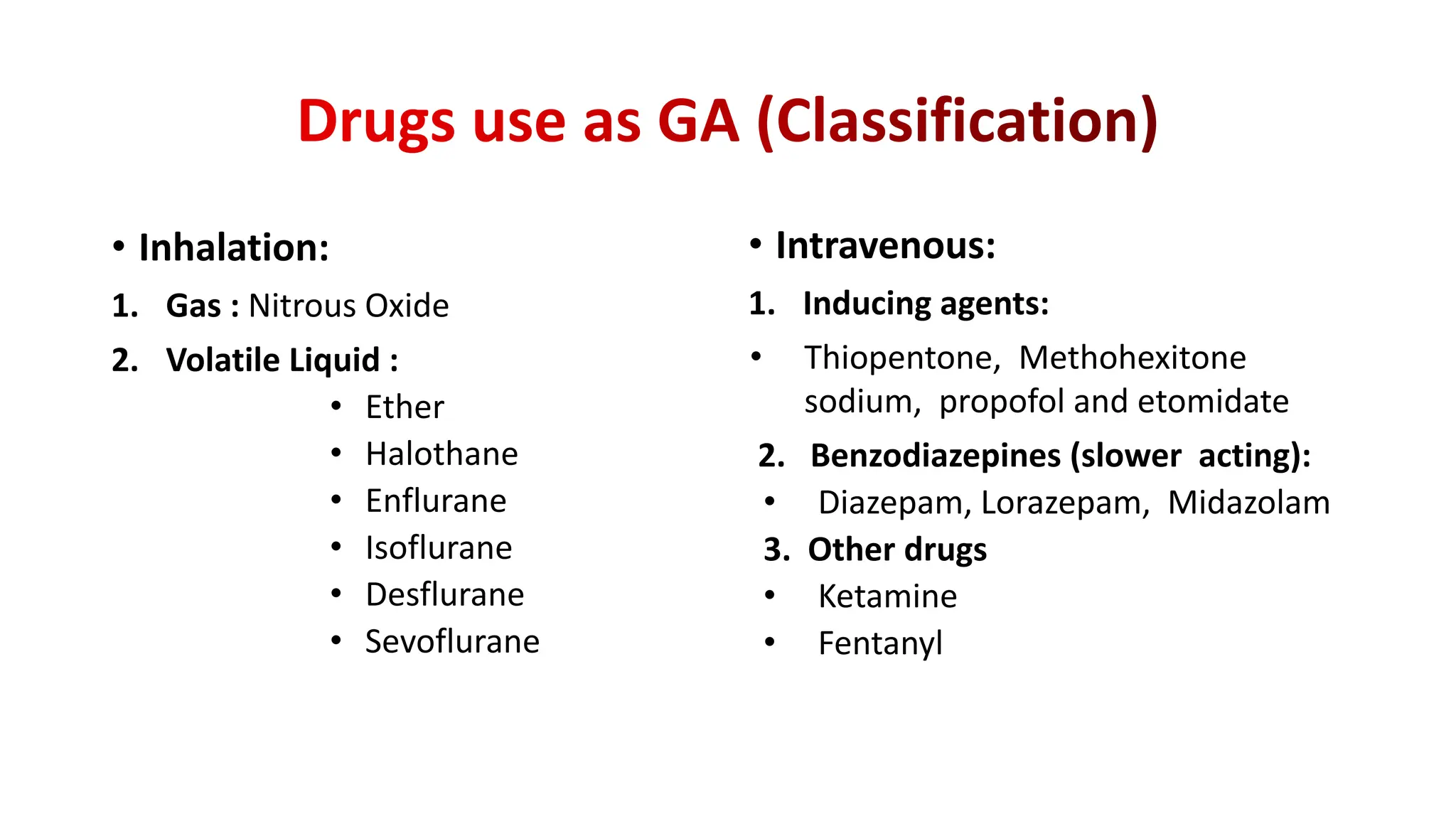
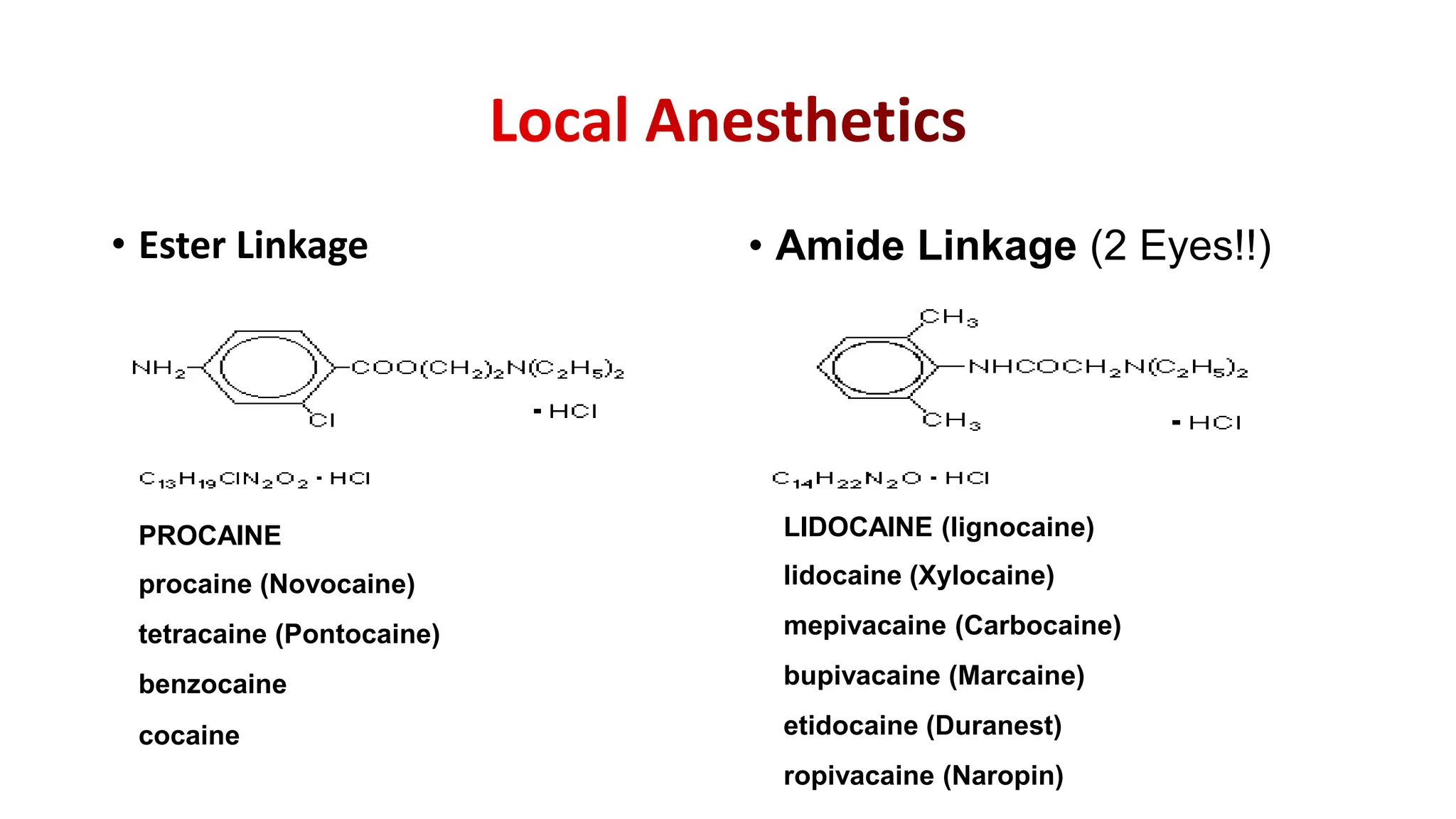
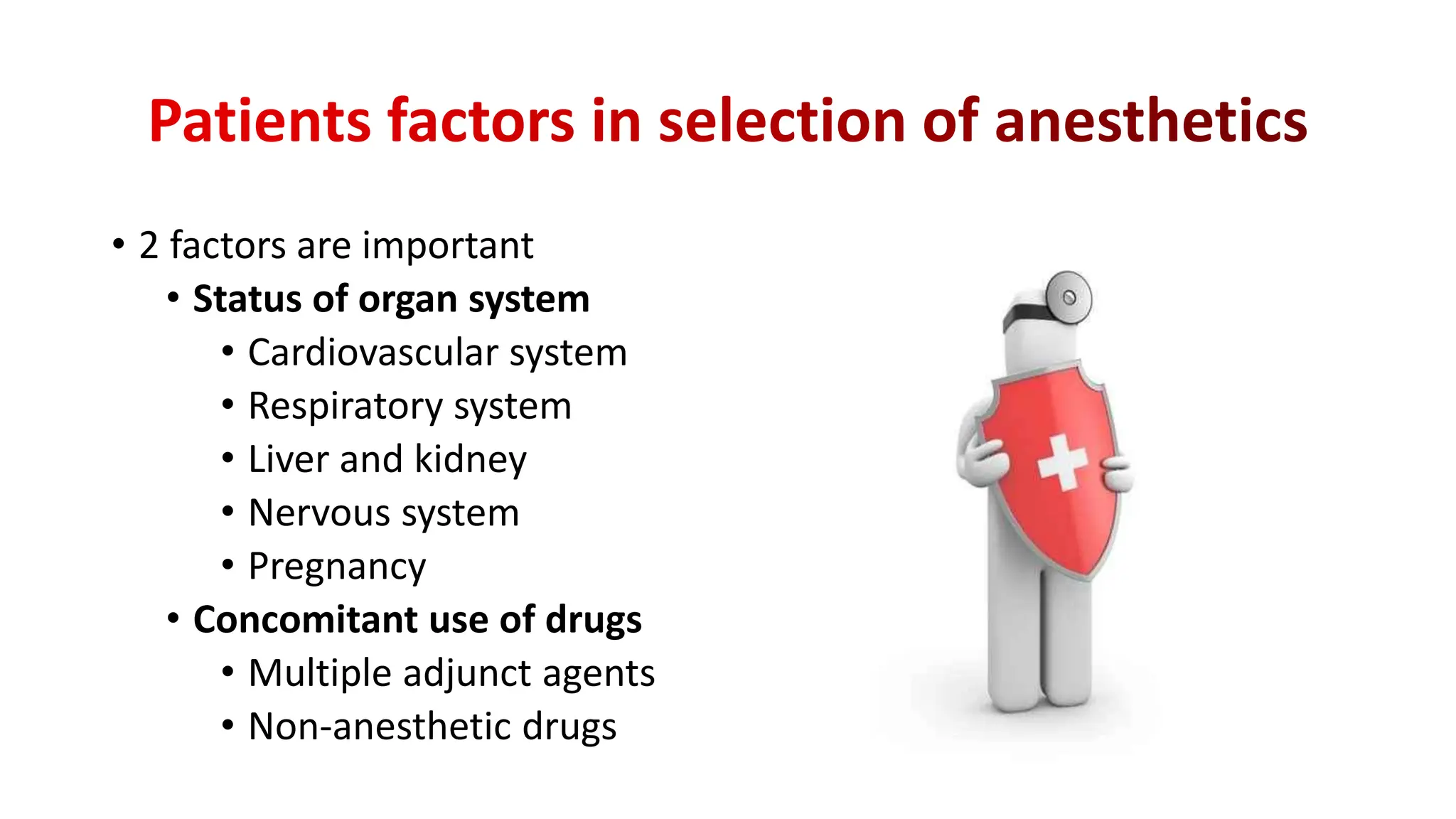
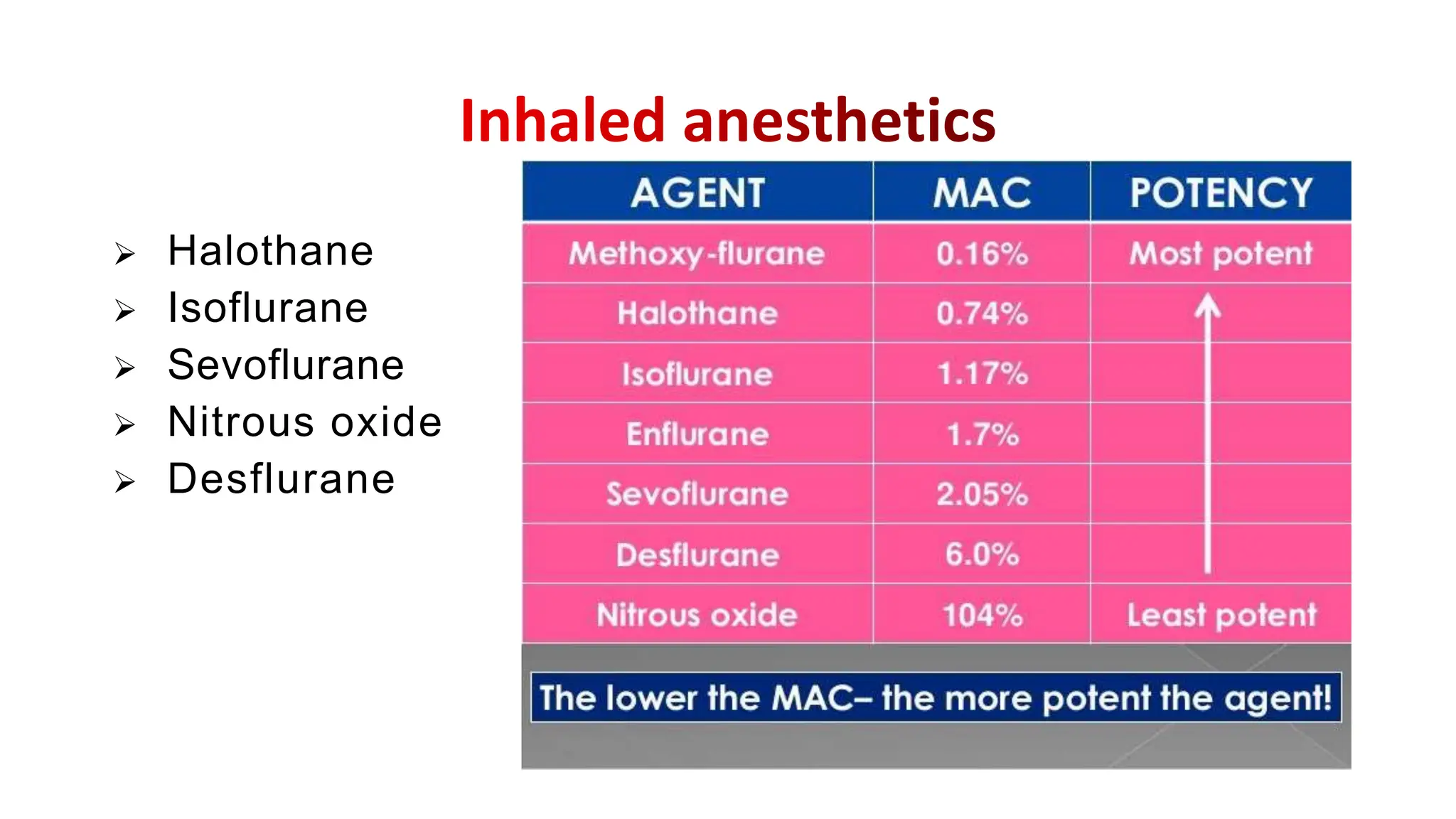
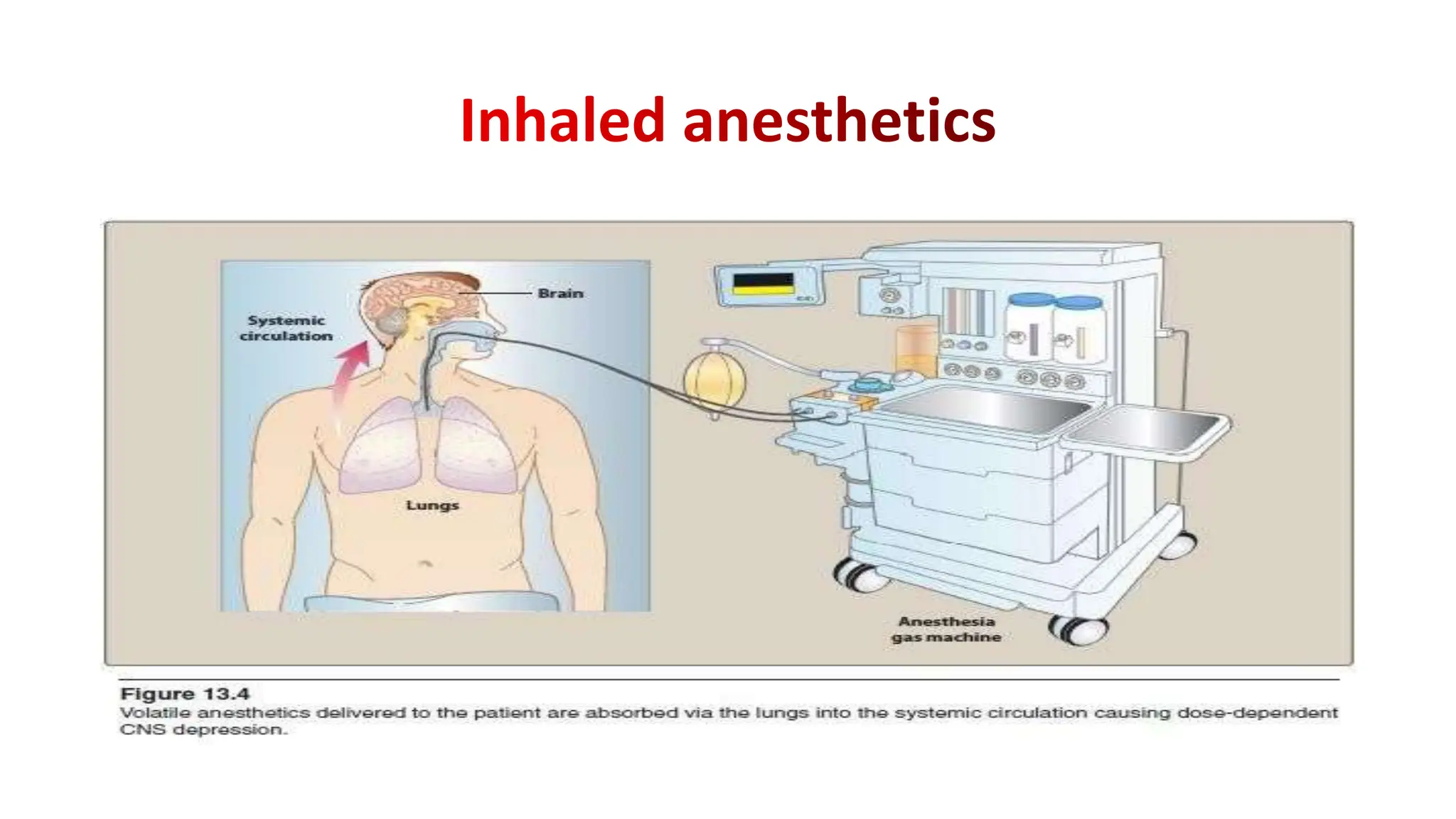
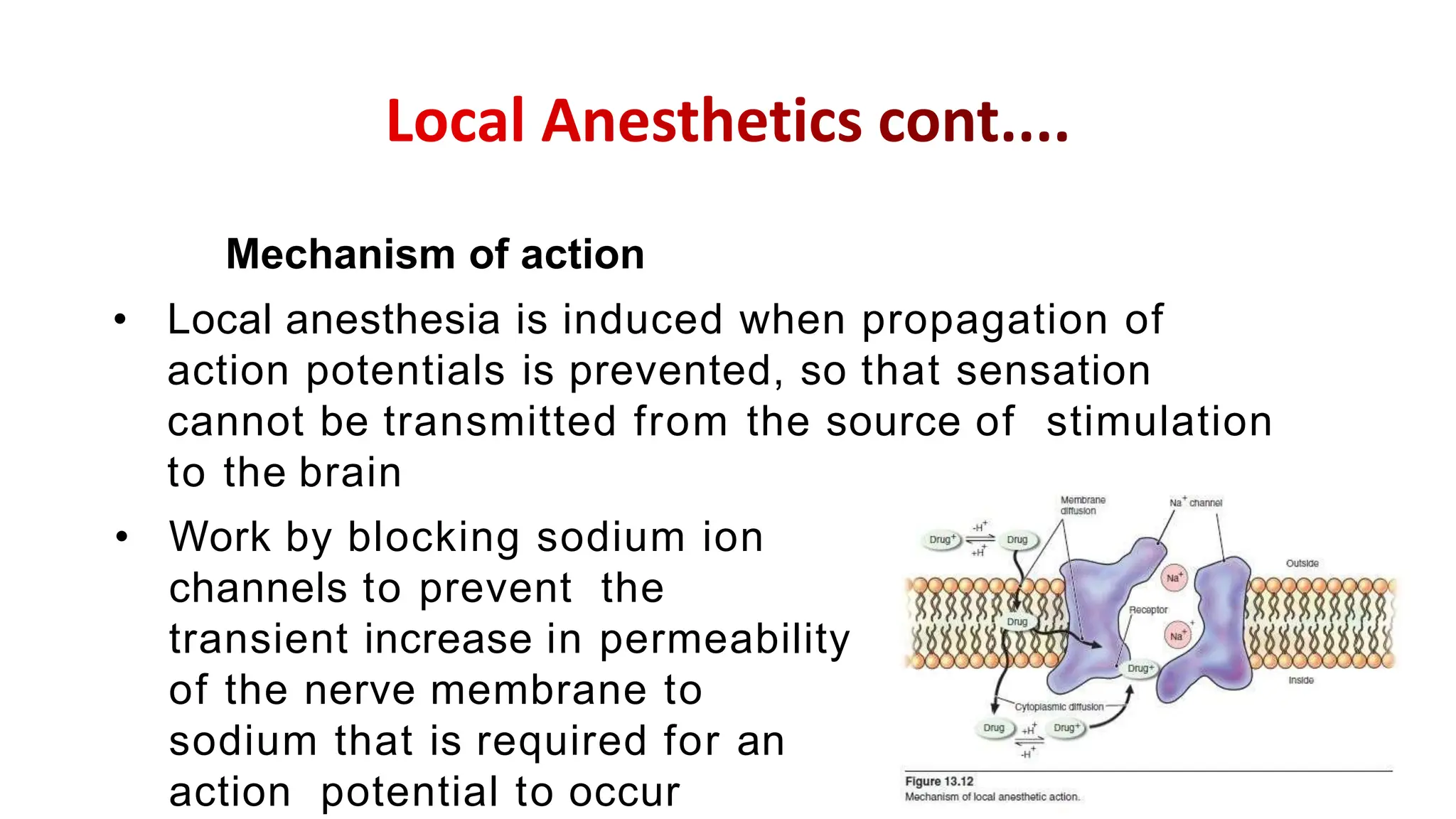
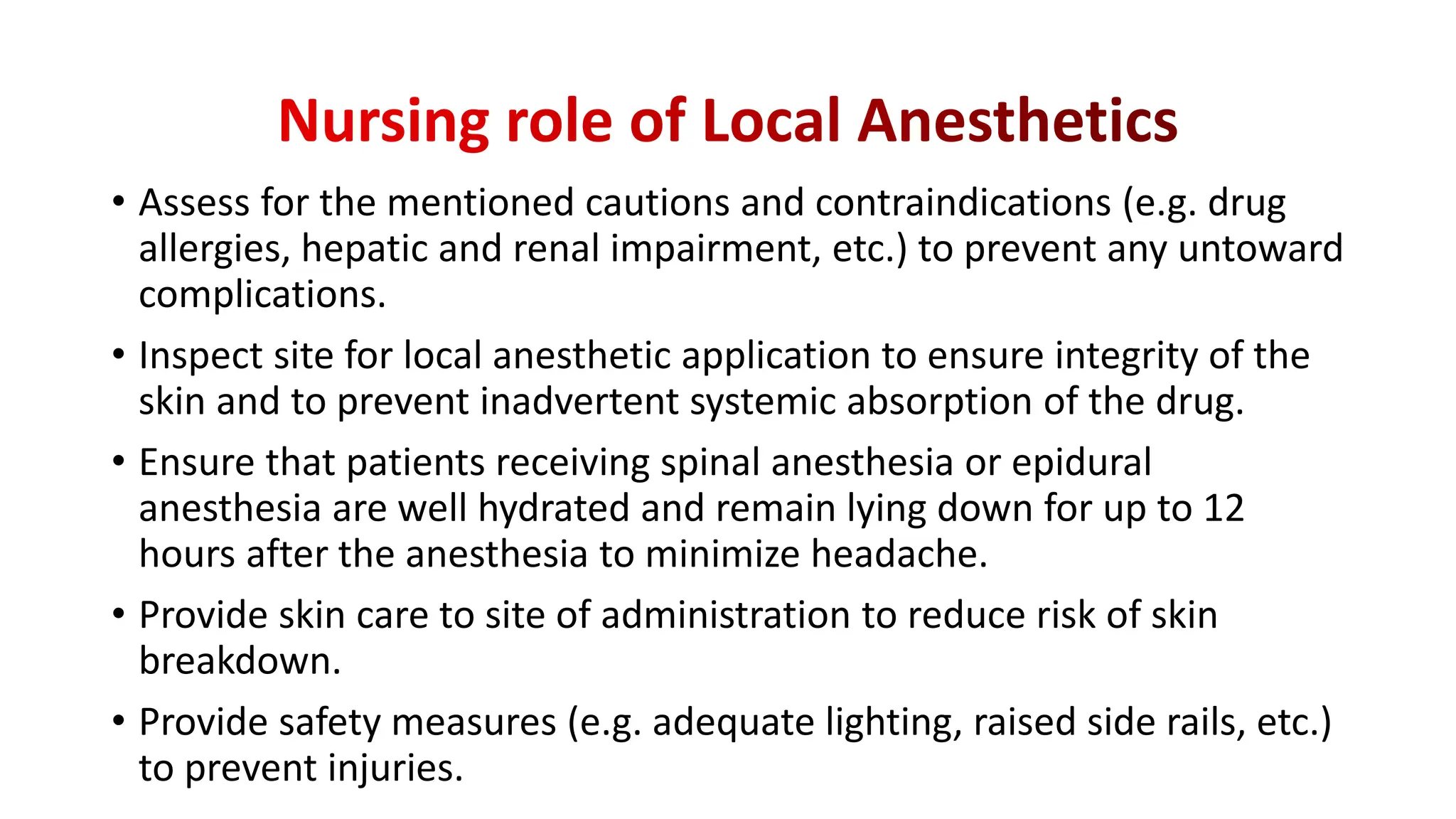
This document provides an overview of anesthetics and anesthesia. It defines anesthesia and differentiates between general and local anesthesia. The four stages of general anesthesia are described. Commonly used general inhalation anesthetics like halothane and intravenous anesthetics like propofol are outlined. Local anesthetics like lidocaine are also discussed. The mechanisms of action, indications, and side effects of various anesthetic agents are reviewed. Factors in choosing anesthetics and the roles of nurses are summarized.


![• Karch, A. M., & Karch. (2011). Focus on nursing pharmacology.
Wolters Kluwer Health/Lippincott Williams & Wilkins. [Link]
• Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill
Education.
• Lehne, R. A., Moore, L. A., Crosby, L. J., & Hamilton, D. B. (2004).
Pharmacology for nursing care.
• Smeltzer, S. C., & Bare, B. G. (1992). Brunner & Suddarth’s textbook of
medical-surgical nursing. Philadelphia: JB Lippincott.](https://image.slidesharecdn.com/anesthetics-240113033722-88391b82/75/Anesthetics-and-its-side-affect-Mechanism-of-action-50-2048.jpg)
