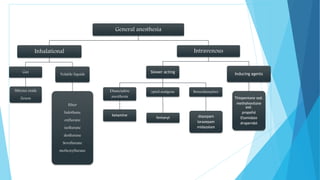
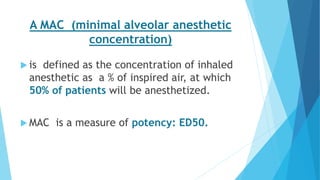
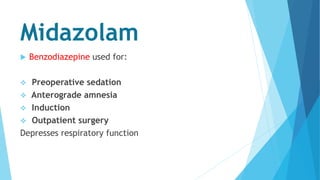
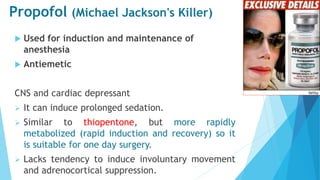
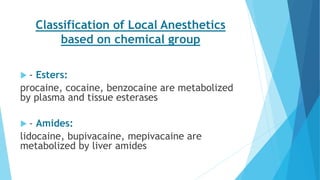
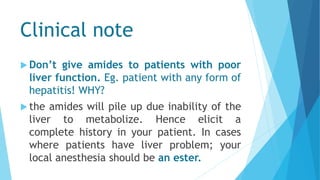
The document provides a history of anesthetics from primitive techniques to modern discoveries. It discusses Crawford Long using ether anesthesia in 1842, followed by chloroform and nitrous oxide. In 1846, William Morton demonstrated ether anesthesia publicly at Massachusetts General Hospital, considered the beginning of modern anesthesia. The document also describes different types of anesthesia including general, regional, and local, and their mechanisms of action and uses. It discusses various anesthetic drugs and their properties.