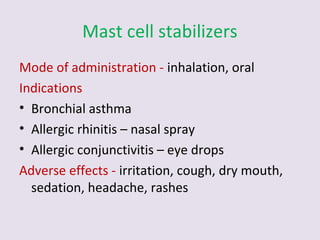
This document provides information on the treatment of bronchial asthma. It discusses the major classes of drugs used including bronchodilators like beta agonists, anticholinergics, and methylxanthines. It also covers corticosteroids, mast cell stabilizers, and leukotriene modulators. For each class the mechanism of action, administration route, indications, and potential adverse effects are outlined. Treatment of an acute asthma attack and contraindicated drugs are also summarized.