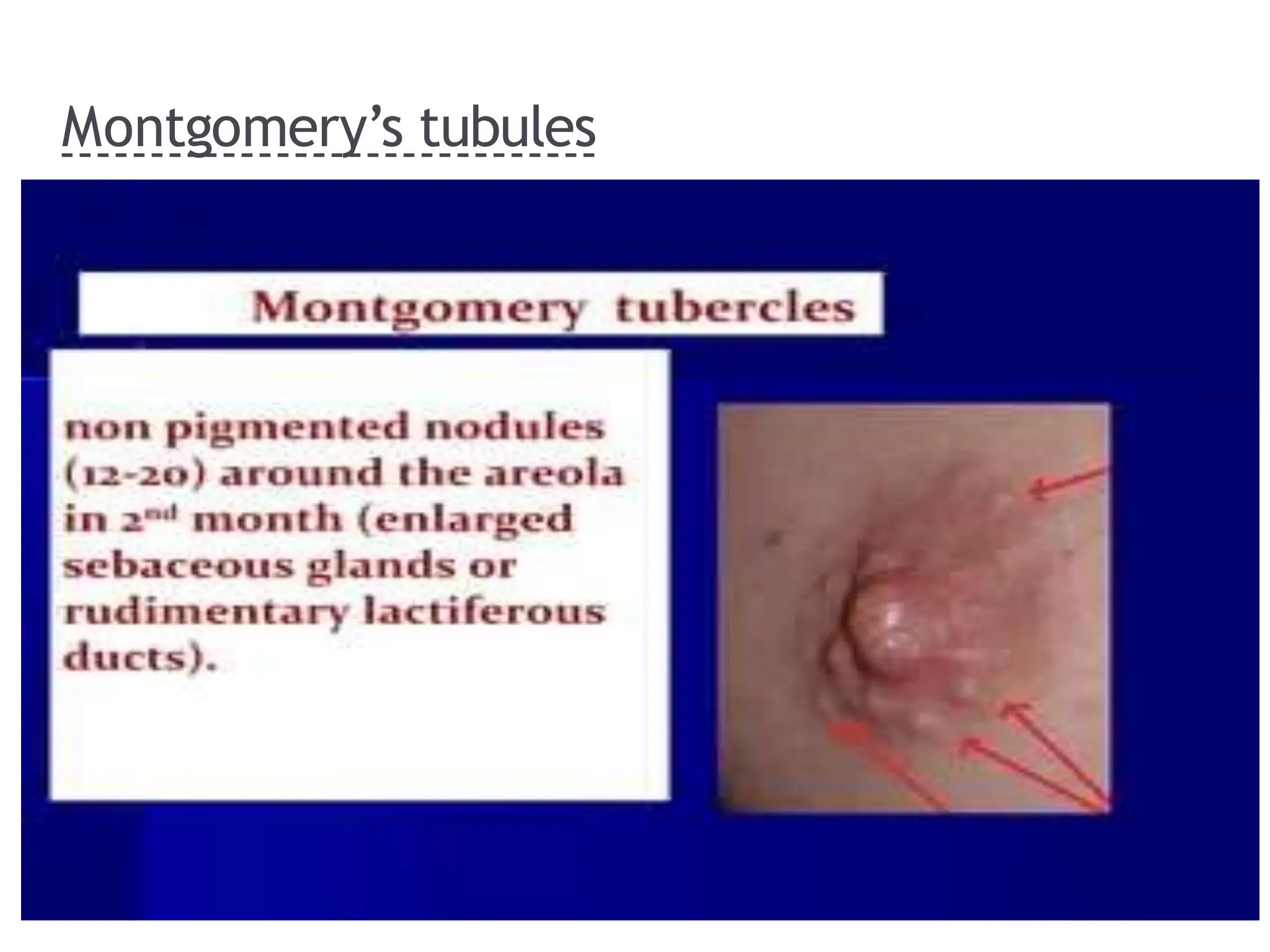
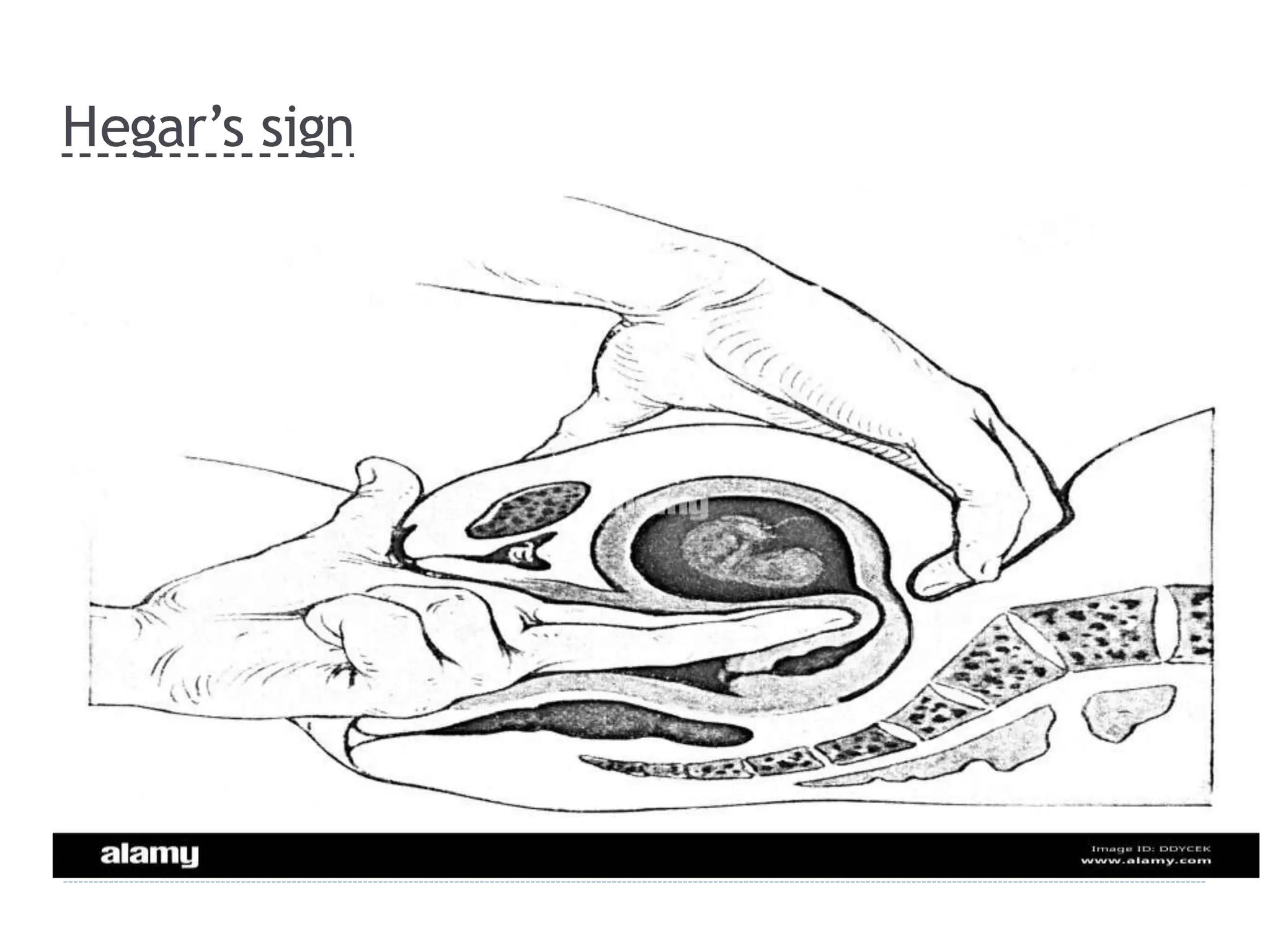
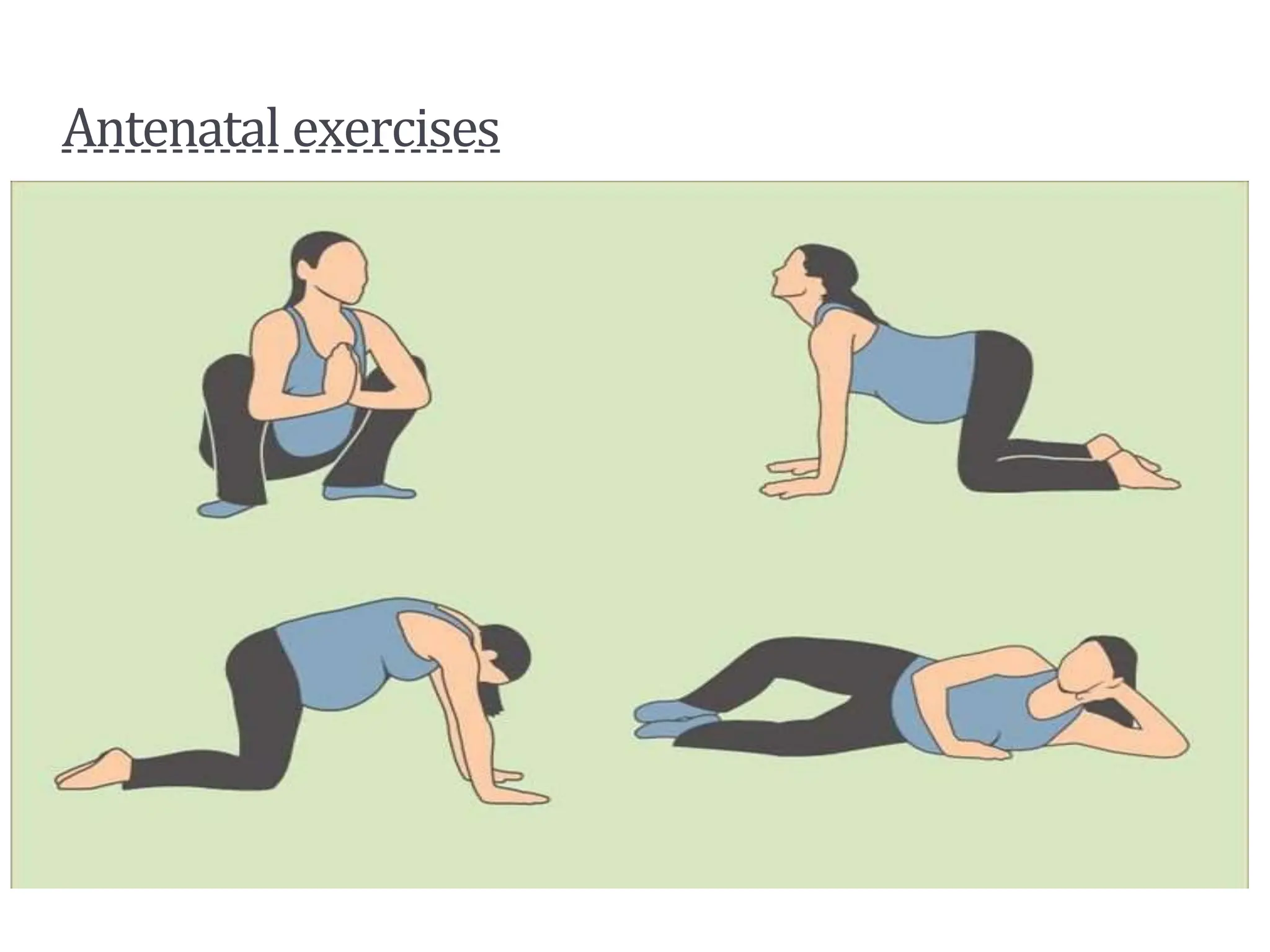
The document outlines the objectives and care practices for antenatal sessions, detailing the definition, aims, and required visits during the three trimesters of pregnancy. It includes information on calculating the expected date of delivery, signs of pregnancy, necessary immunizations, nutritional supplements, and the father's role. Additionally, it lists danger signs of pregnancy that require immediate attention.