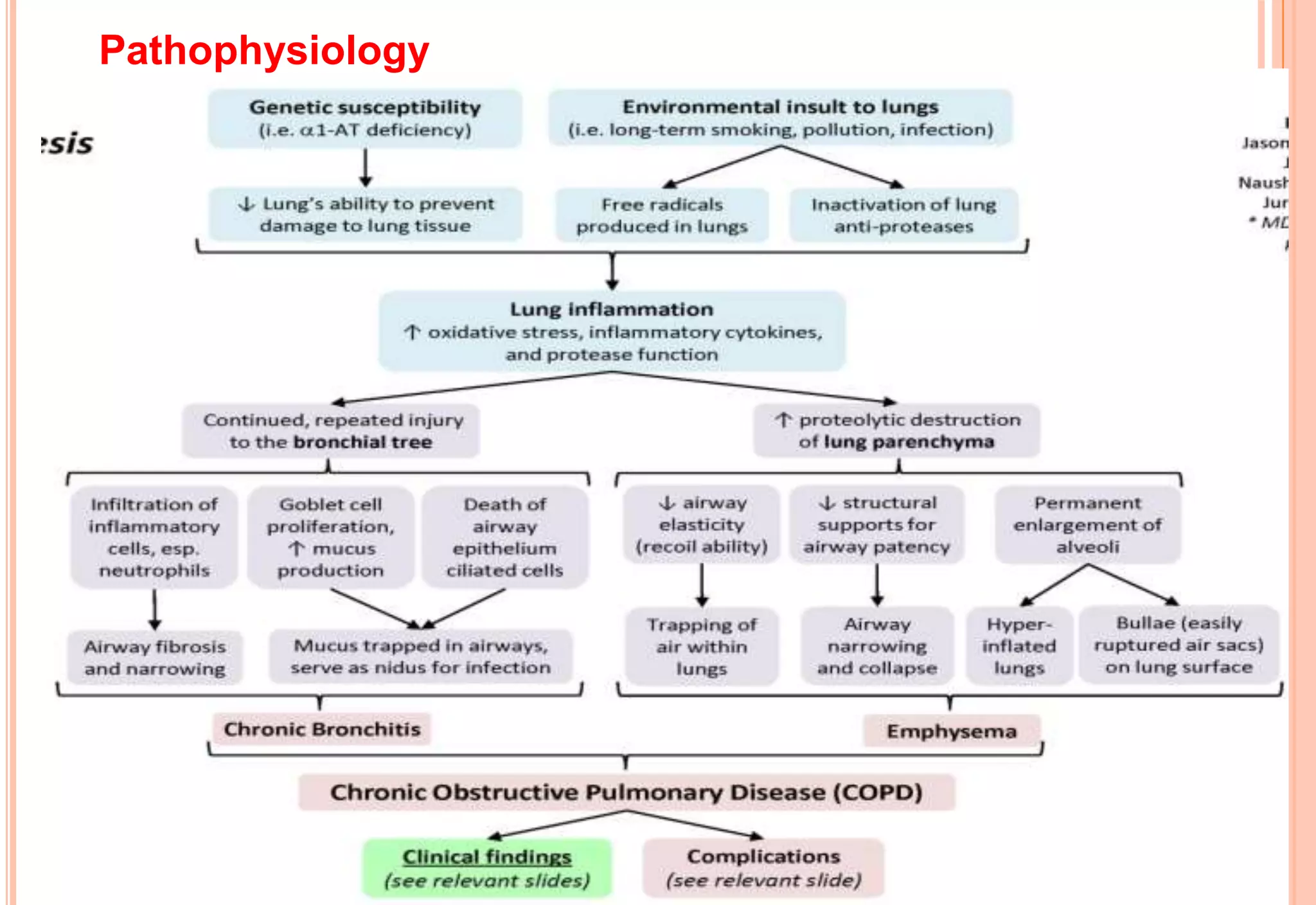
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by chronic obstruction of lung airflow. The two main conditions that make up COPD are chronic bronchitis and emphysema. COPD is the fifth leading cause of death in the United States. Smoking is the primary risk factor for COPD. Symptoms include cough, sputum production, shortness of breath, and wheezing. Treatment focuses on bronchodilators, corticosteroids, oxygen therapy, pulmonary rehabilitation, and smoking cessation. Nursing management for COPD patients focuses on improving ventilation and gas exchange, managing activity intolerance and anxiety, and effectively clearing airways through techniques like chest physiotherapy.