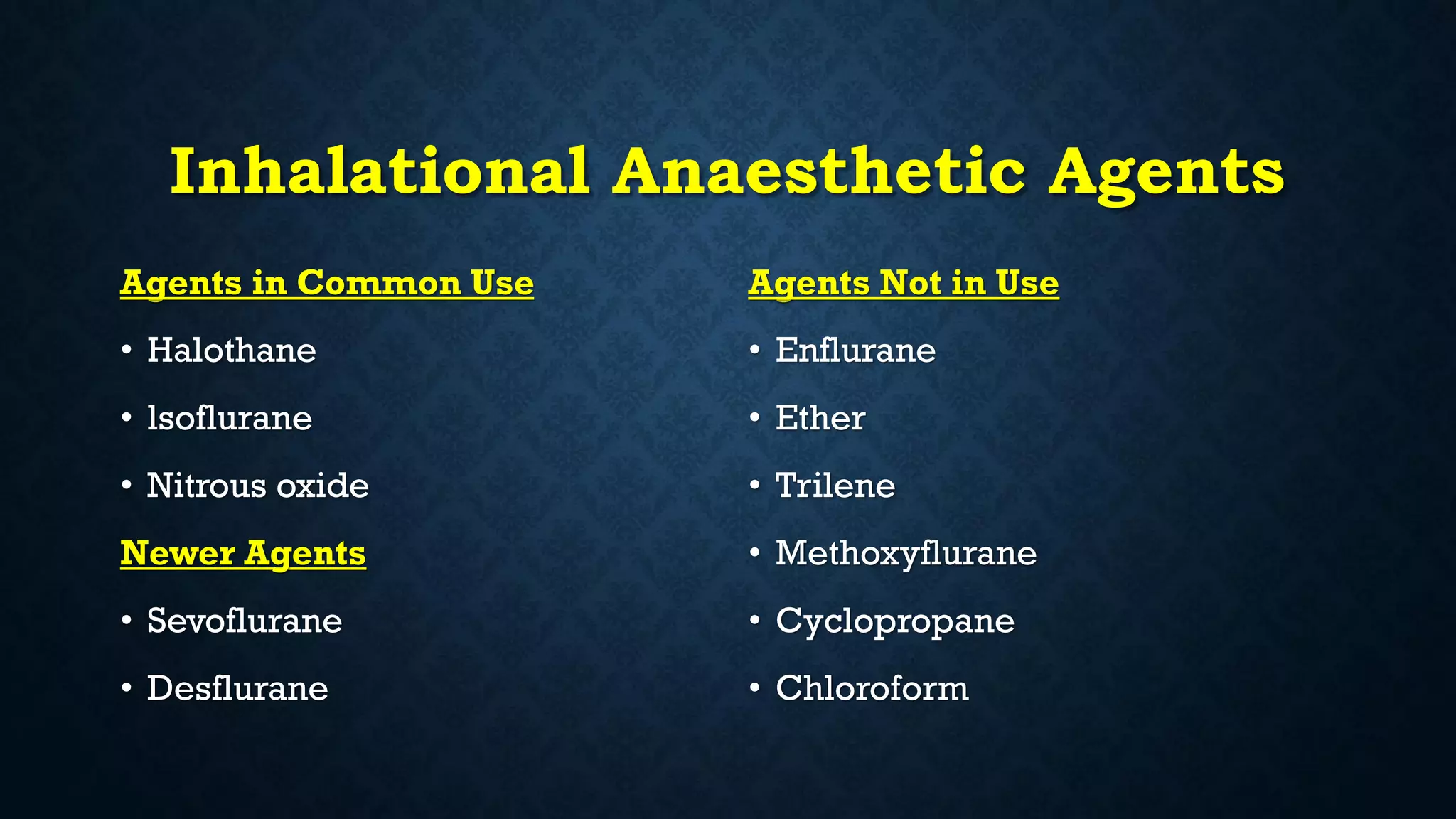
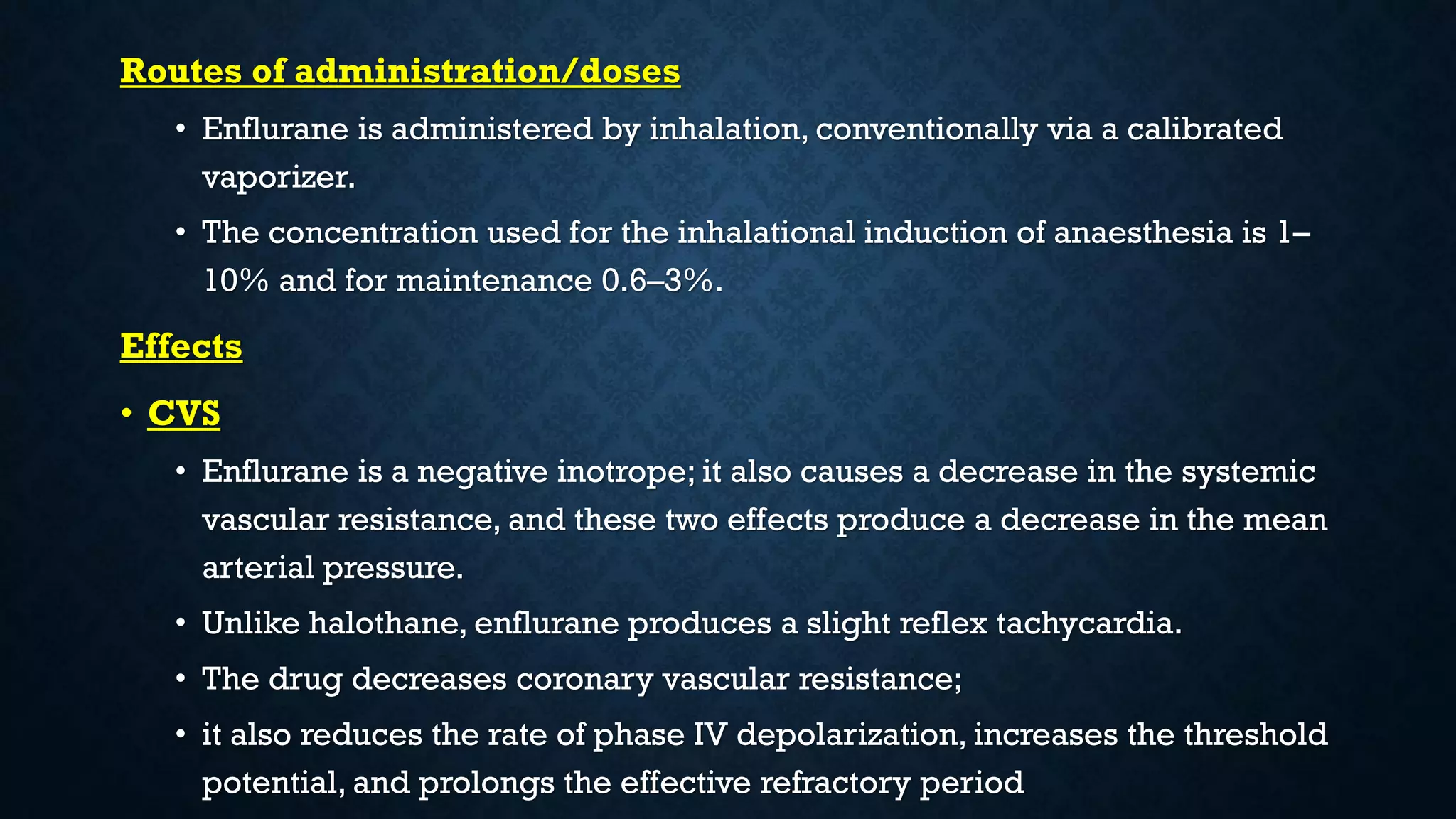
The document discusses various inhalational anesthetic agents used in general anesthesia, including halothane, isoflurane, sevoflurane, desflurane, enflurane, and nitrous oxide, detailing their usage, presentation, main actions, mechanisms of action, routes of administration, effects, contraindications, and potential side effects. Each agent is described with its molecular properties, dosing parameters, and the contexts in which they are preferred or contraindicated, addressing their impacts on the cardiovascular, respiratory, and central nervous systems. Additionally, variations in the minimum alveolar concentration (MAC) and factors affecting their pharmacodynamics are highlighted, emphasizing the importance of careful management in anesthesia practice.