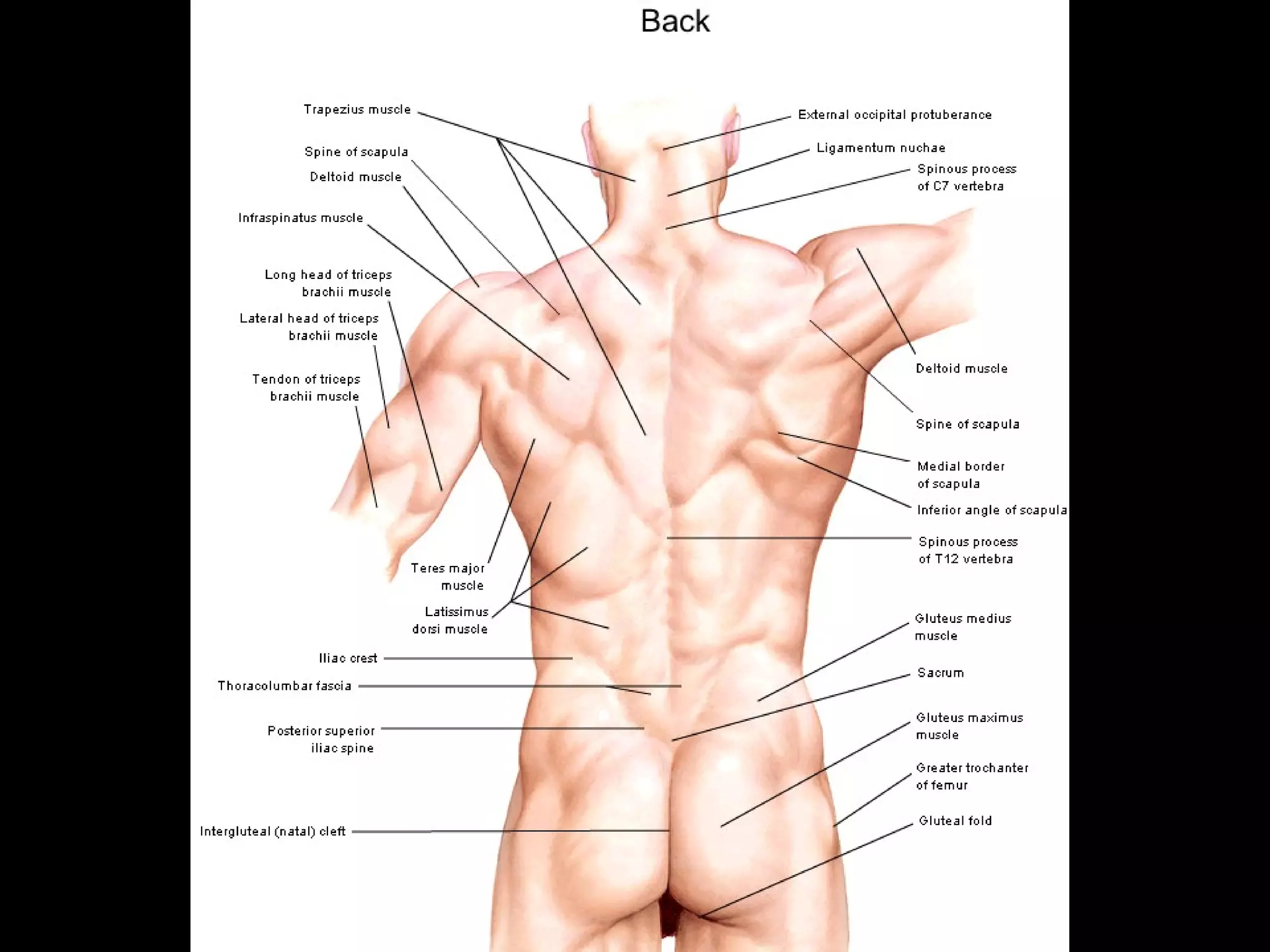
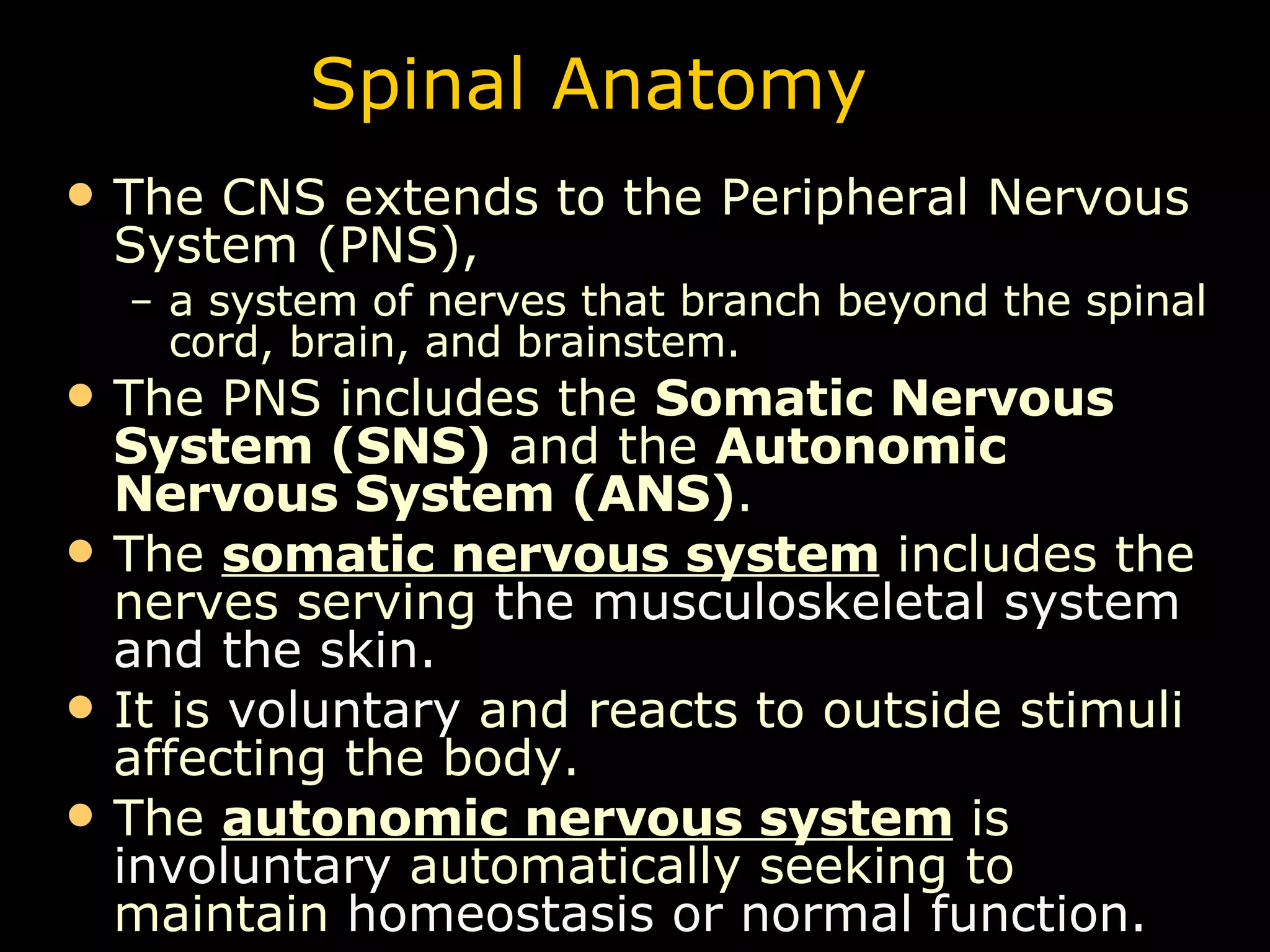
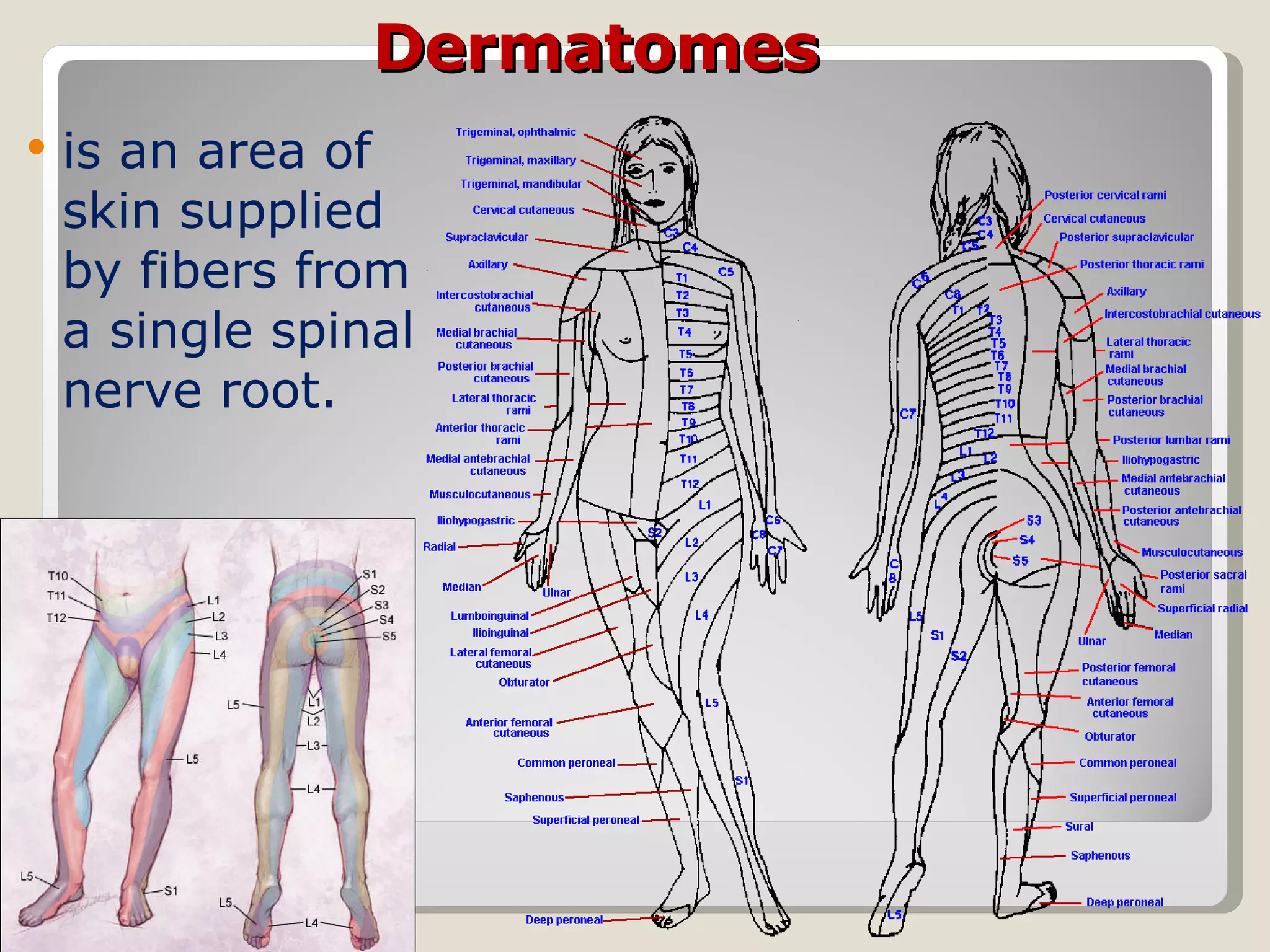
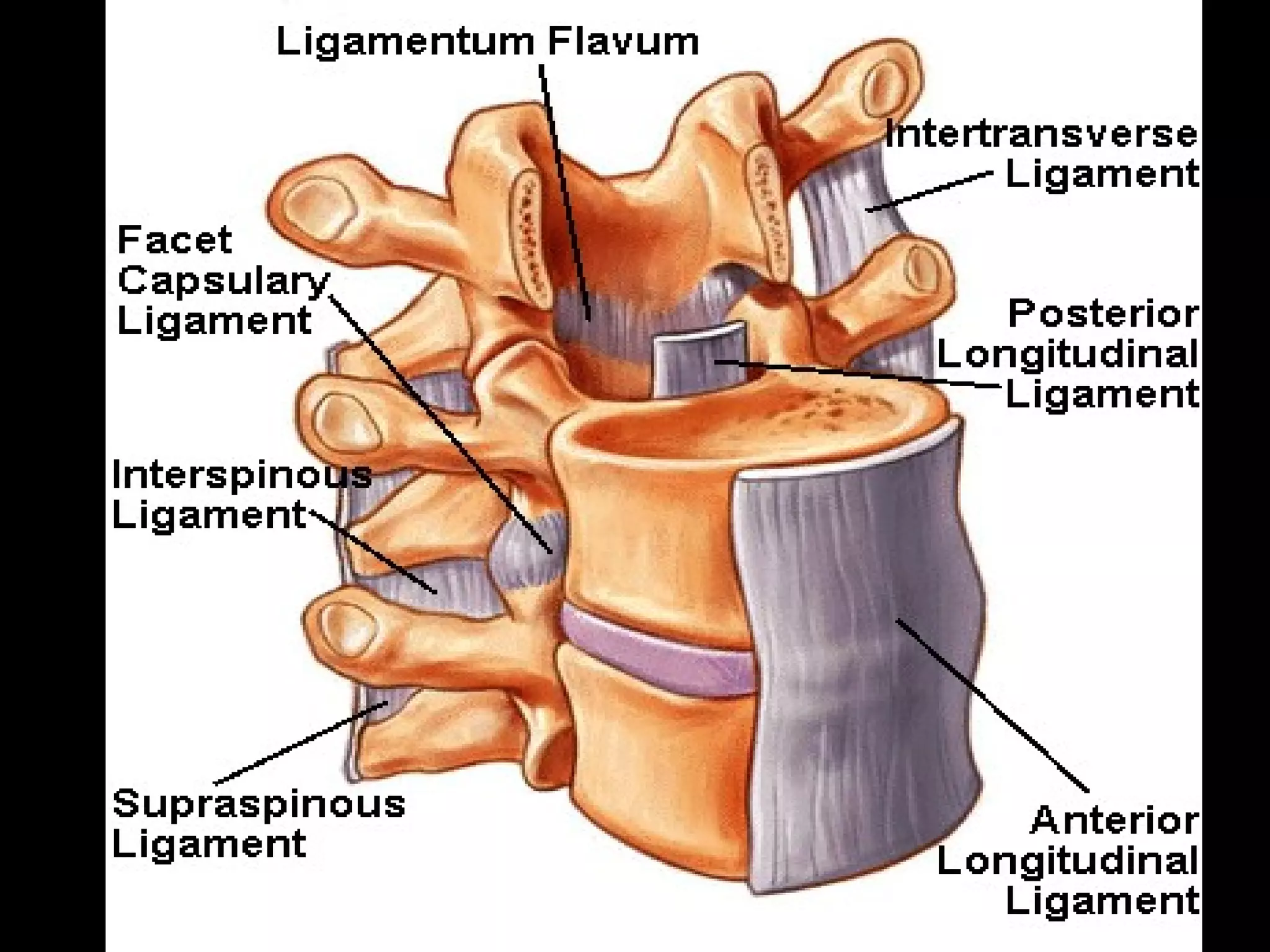
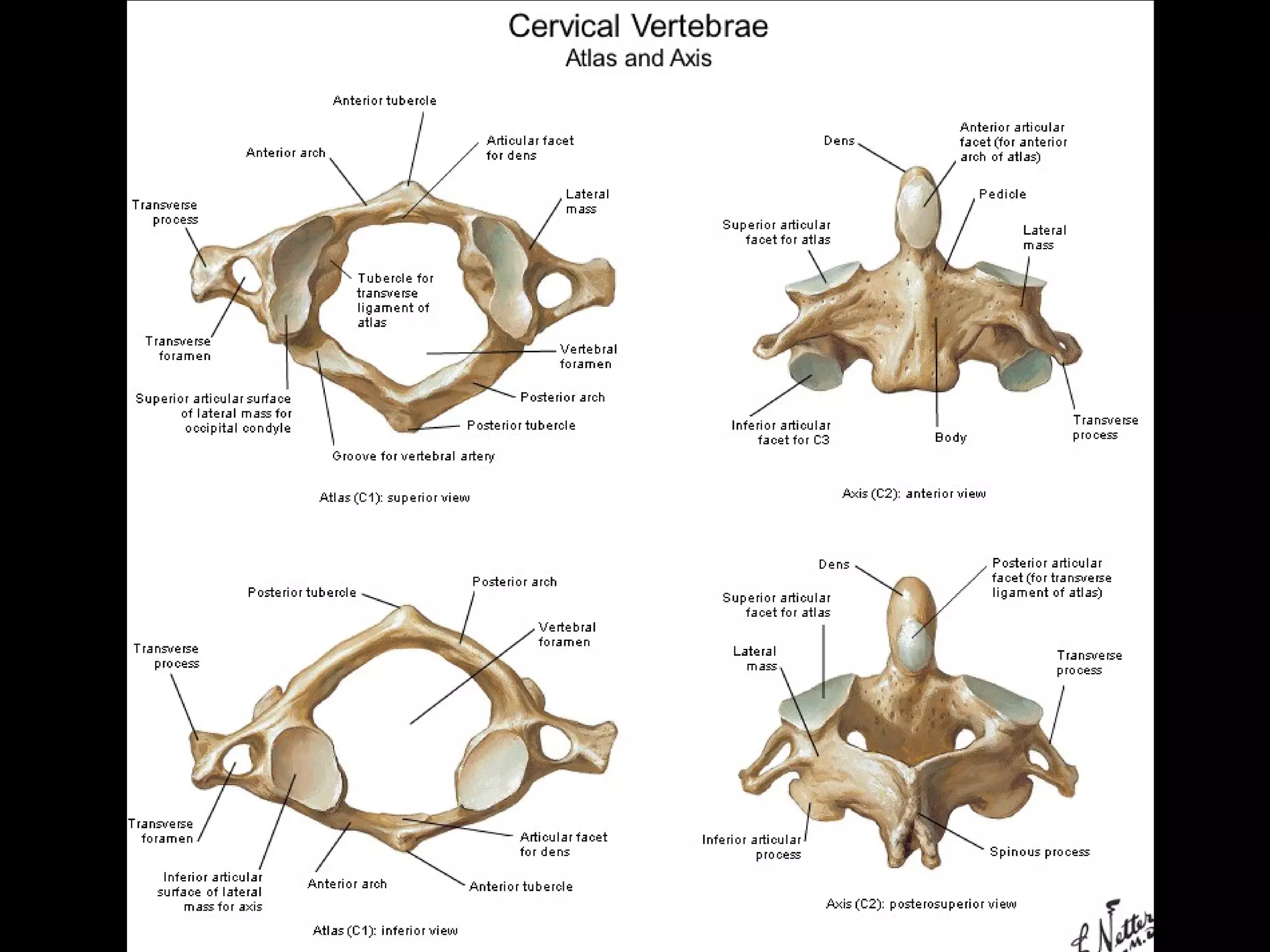
The document summarizes key aspects of spinal anatomy and common spinal injuries. It describes the components of the spine, including vertebrae, discs, ligaments, and nerves. It discusses the cervical, thoracic, and lumbar curves. It also summarizes common spinal injuries like strains, fractures, and spinal cord injuries; symptoms; imaging studies; and treatments.
























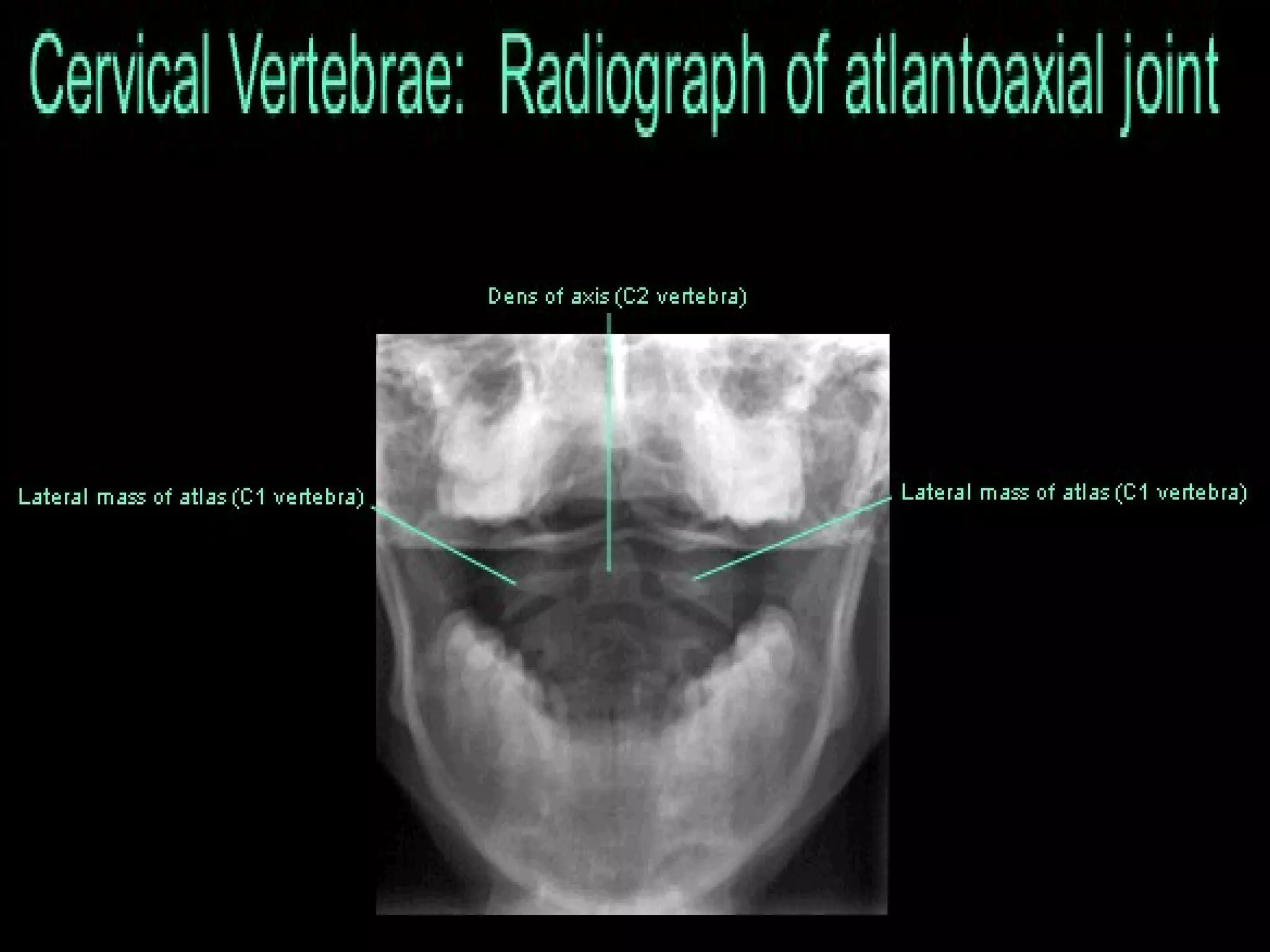
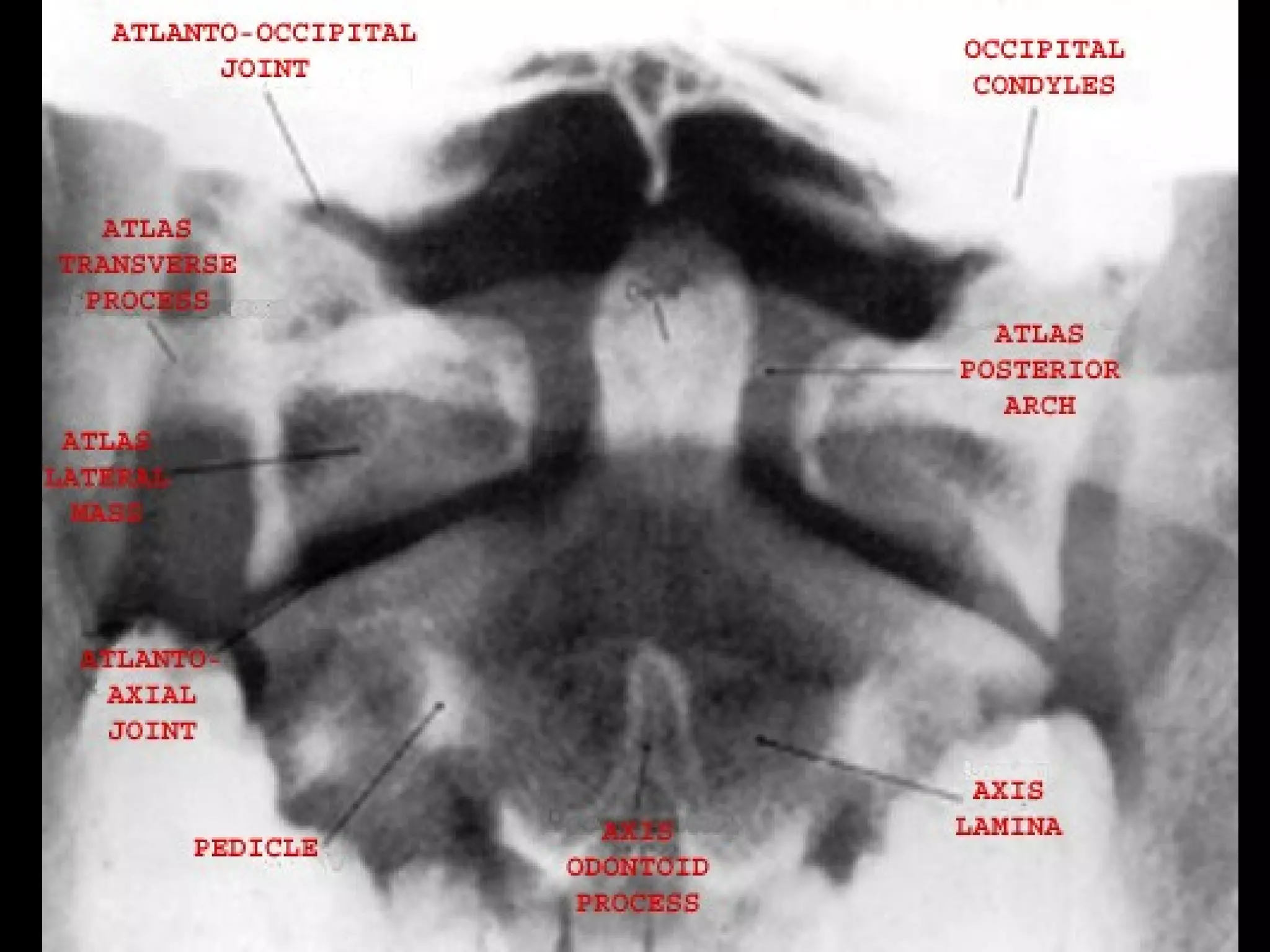
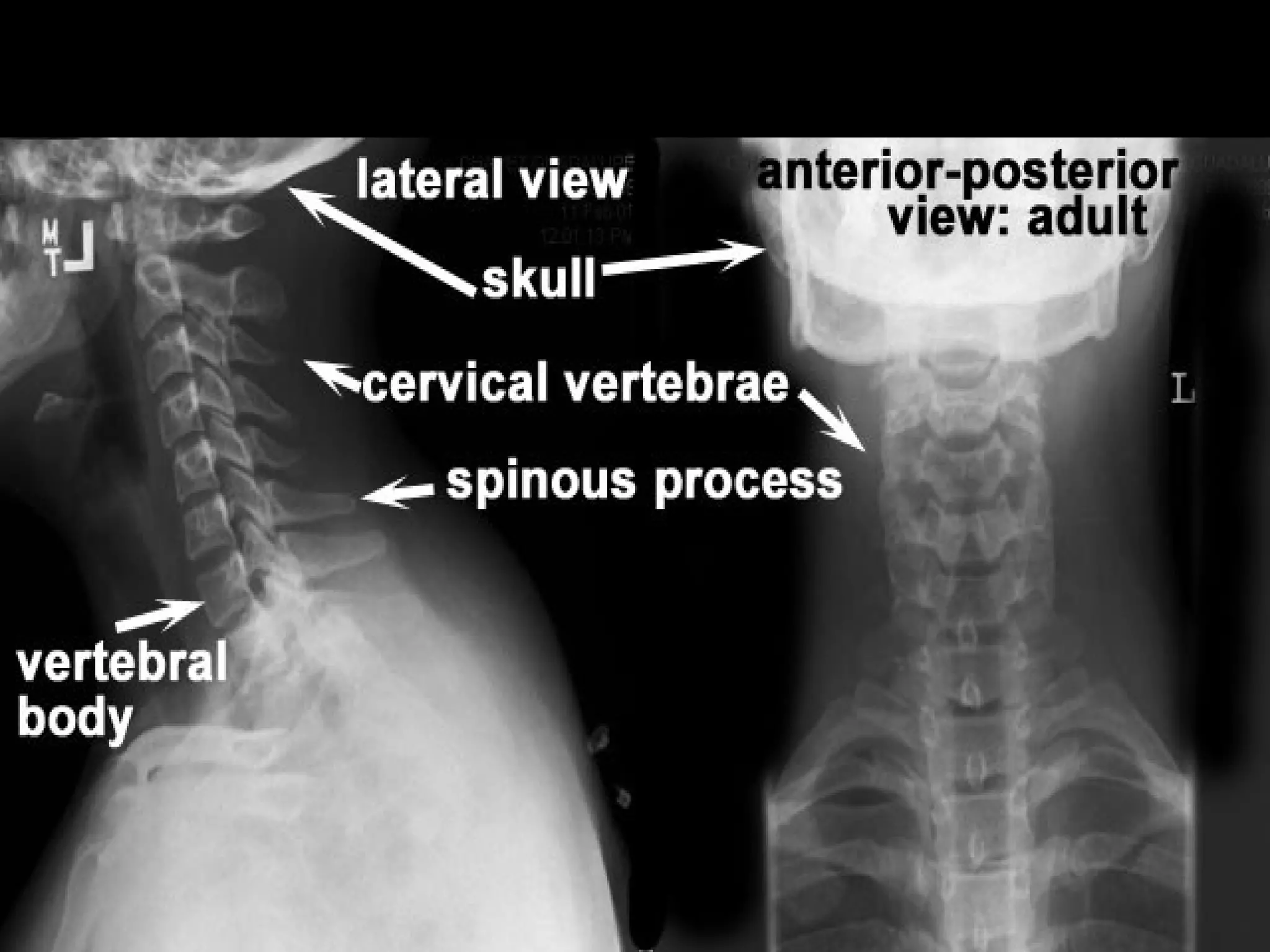
![Spinal Anatomy Injury or mild trauma to the cervical spine can cause a serious or life-threatening medical emergency [e.g. spinal cord injury (SCI) or fracture]. Pain, numbness, weakness, and tingling are symptoms that may develop when one or more spinal nerves are injured, irritated, or stretched. The cervical nerves control many bodily functions and sensory activities.](https://image.slidesharecdn.com/anatomy-lect-5-trunk-spine-1224901892157255-8/75/Anatomy-Lect-5-Trunk-Spine-30-2048.jpg)





























































































































![Chance Fracture With flexion-distraction mechanisms such as those observed in passengers restrained with lap seatbelts , a progression of injury from the posterior column of the thoracolumbar spine is observed anteriorly. The diagnosis is best made on good quality radiographs obtained in 2 planes (anteroposterior [AP] and lateral).](https://image.slidesharecdn.com/anatomy-lect-5-trunk-spine-1224901892157255-8/75/Anatomy-Lect-5-Trunk-Spine-163-2048.jpg)


















