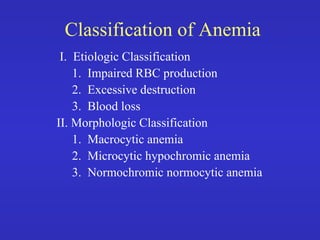
This document provides an overview of anemia, including its classification and causes. It discusses impaired red blood cell production, excessive destruction of RBCs, and blood loss as the main etiologic classifications. The morphologic classifications are macrocytic, microcytic hypochromic, and normochromic normocytic anemia. Causes of impaired RBC production include bone marrow abnormalities and deficiencies in essential factors or stimulation factors. Excessive destruction can be due to intracorpuscular or extracorpuscular defects. Blood loss can be acute or chronic. Specific causes are discussed under each classification.