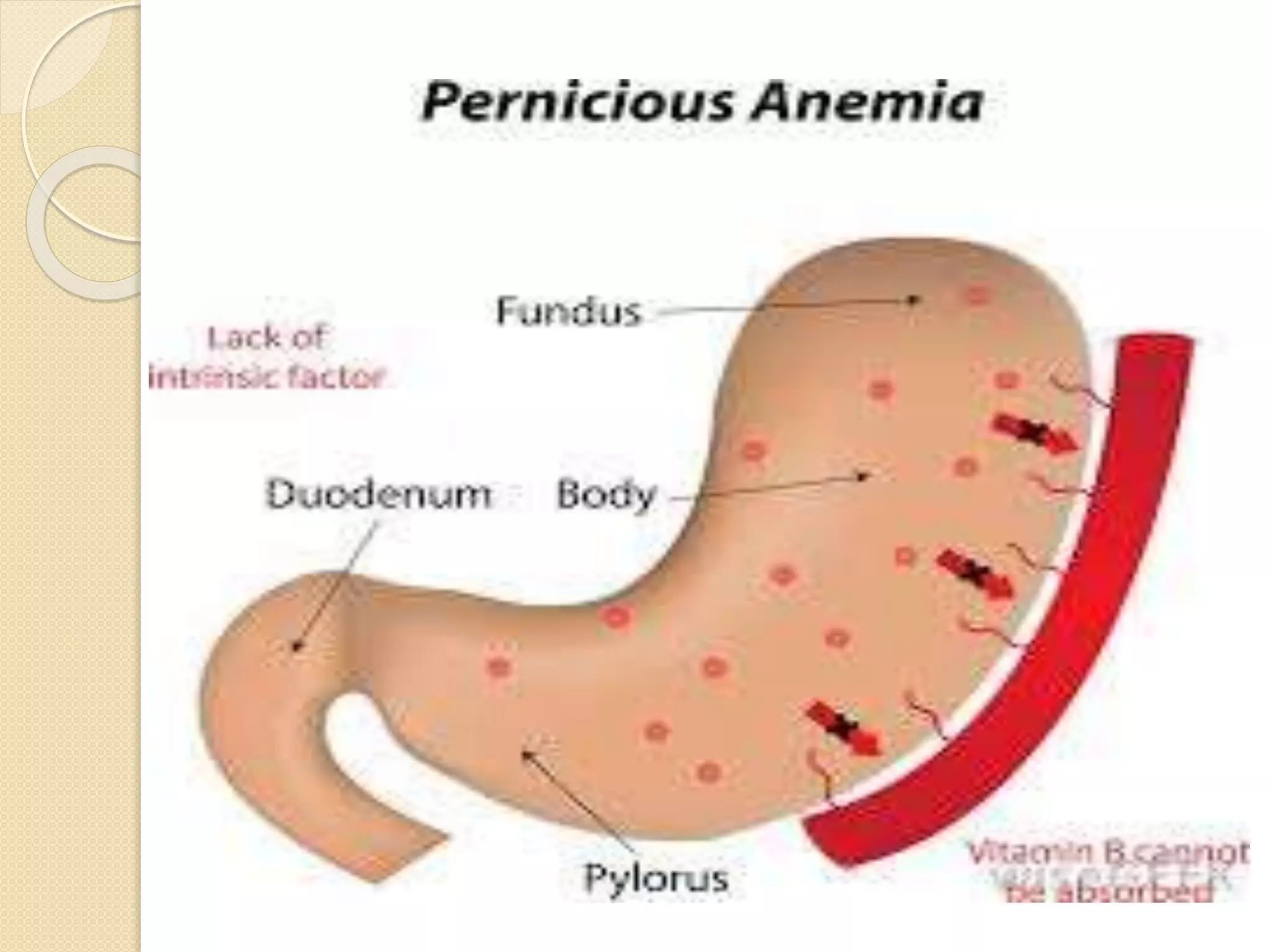
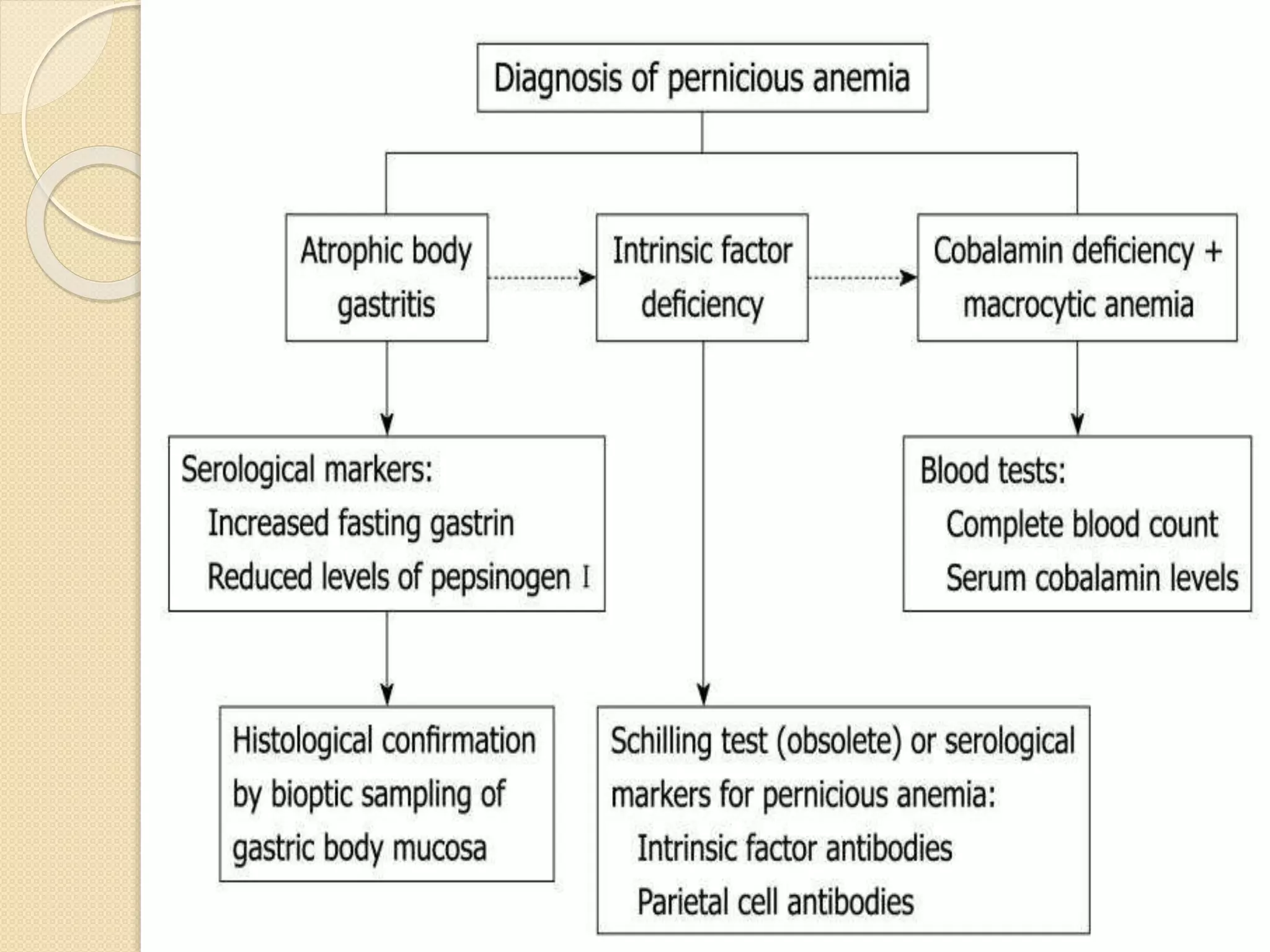
Pernicious anemia is a chronic disorder caused by Vitamin B12 deficiency due to failure of intrinsic factor secretion from gastric atrophy. It results in megaloblastic anemia and neurological manifestations. Diagnosis involves clinical features of macrocytic anemia, neurological symptoms, and low serum B12 levels. Treatment involves lifelong Vitamin B12 supplementation through injections.