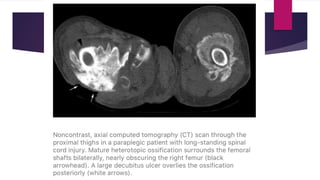
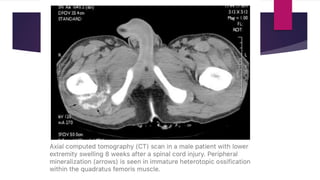
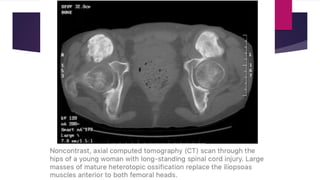
Myositis ossificans, now known as heterotopic ossification (HO), refers to the formation of bone within muscle or soft tissue. There are several classifications of HO, including heterotopic ossification per se, traumatic HO, neurogenic HO, and fibrodysplasia ossificans progressiva. Traumatic HO most commonly develops after musculoskeletal injuries and surgery and can lead to joint stiffness and loss of function. Neurogenic HO occurs after spinal cord or brain injuries. Fibrodysplasia ossificans progressiva is a rare genetic condition characterized by progressive HO.