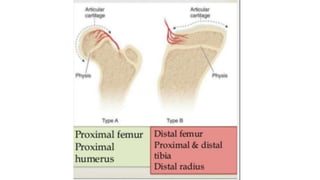
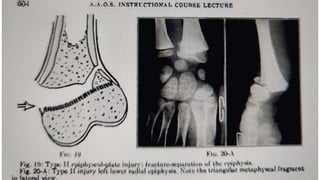
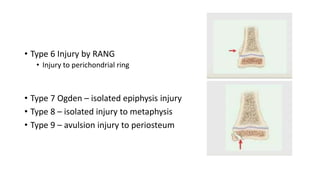
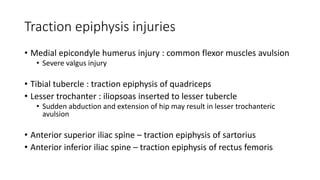
This document discusses epiphyseal injuries in children. It notes that growth disturbance is the most common complication if not properly diagnosed and managed. It describes the two types of epiphysis - pressure and traction - and provides examples. It also details the Salter-Harris classification system for epiphyseal injuries. Key factors in prognosis include the type and location of injury, the child's age, degree of displacement, and whether the blood supply is disrupted. Early closed reduction within 10 days of injury generally leads to the best outcomes.