1. Amputation involves cutting through bone or joint to remove part or all of a limb. It is usually done as a treatment for a dead, dangerous, or severely problematic limb.
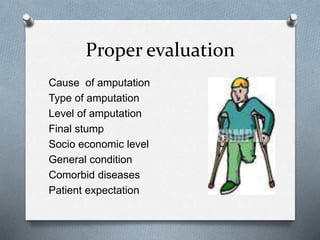
2. Several factors determine the appropriate level of amputation, including the patient's age, underlying condition, and goals for mobility.
3. Proper rehabilitation following amputation, including exercises, stump care, desensitization, and eventually prosthesis training, can help patients regain function and mobility. Complications are minimized with a coordinated post-op care plan.