1. The document discusses principles of fractures, including definitions, causes, types, open fractures, fracture healing, and management. It defines a fracture as a break in bone structure.
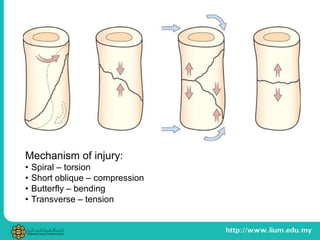
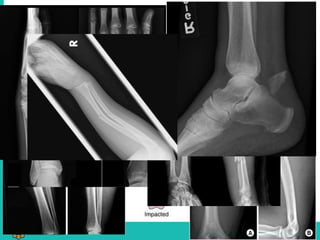
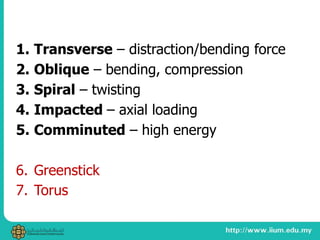
2. Common causes of fractures include direct traumatic force, indirect force, pathological fractures from weakened bone, and stress fractures from repetitive stress. Types include transverse, oblique, spiral, impacted and comminuted.
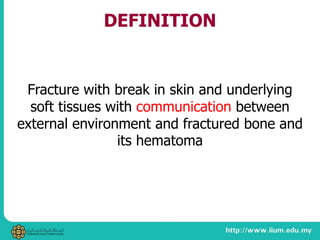
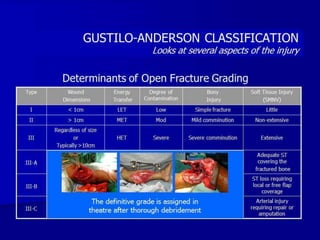
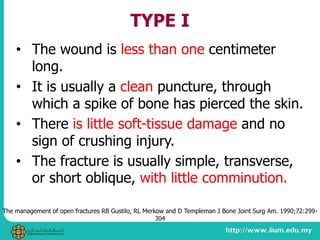
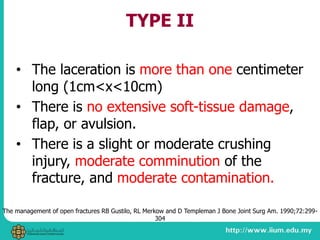
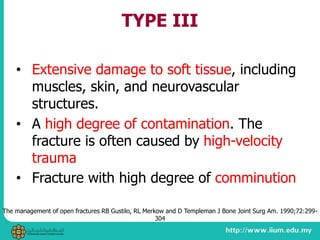
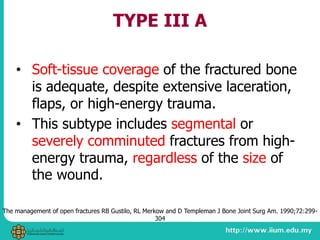
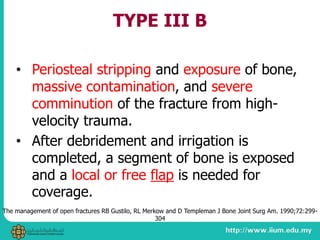
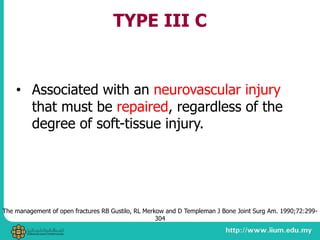
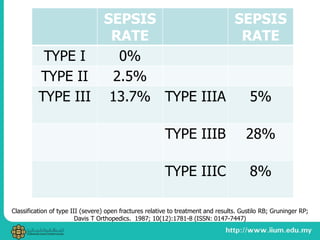
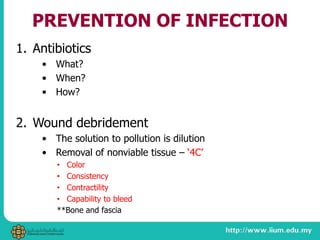
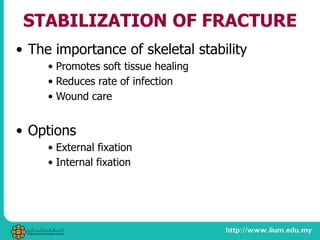
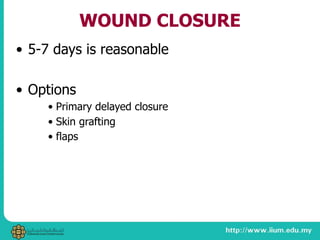
3. Open fractures involve a break in the skin and soft tissues, and are classified using the Gustilo system from Type I to III based on wound size, soft tissue damage, and bone comminution.