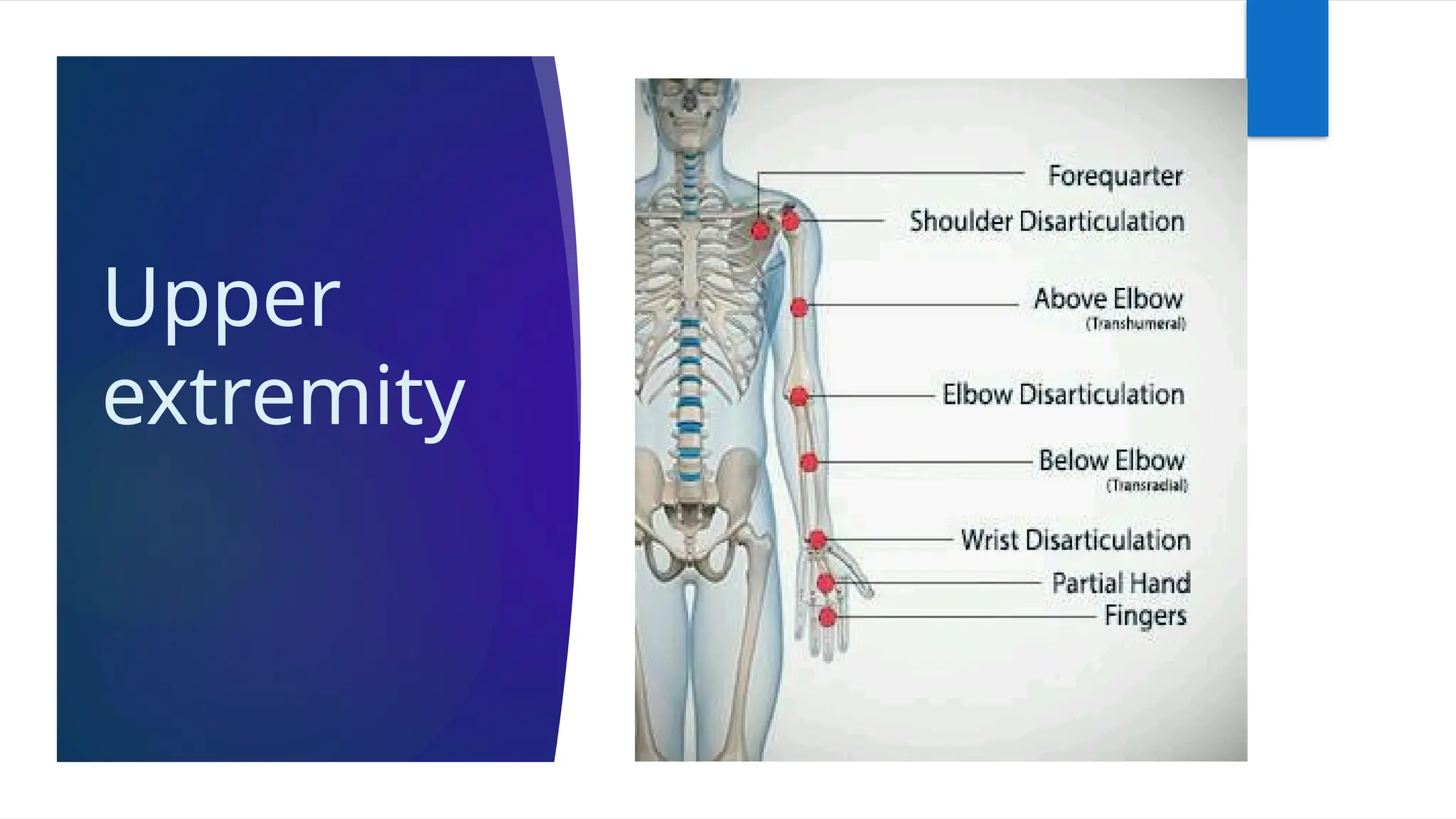
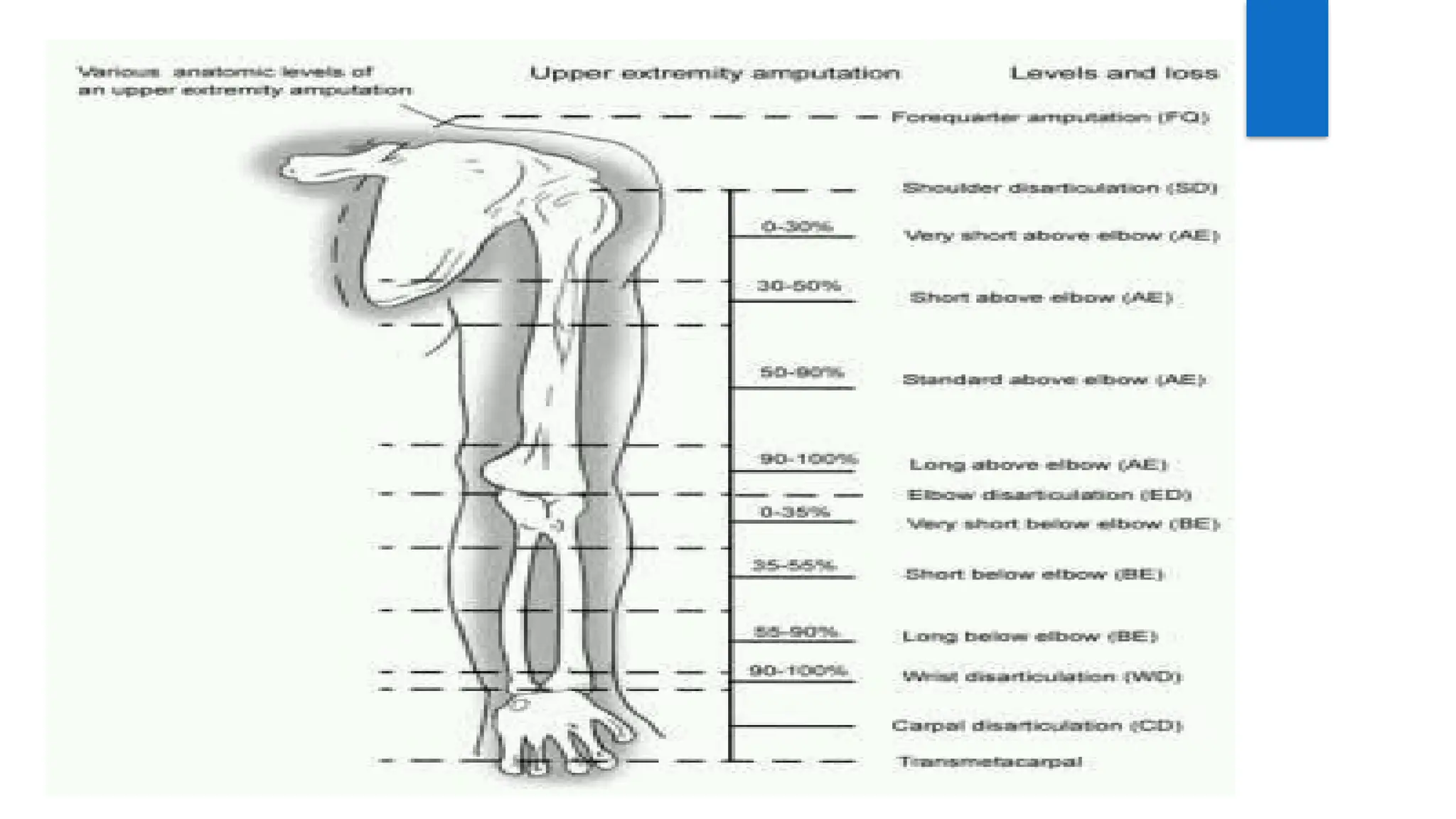
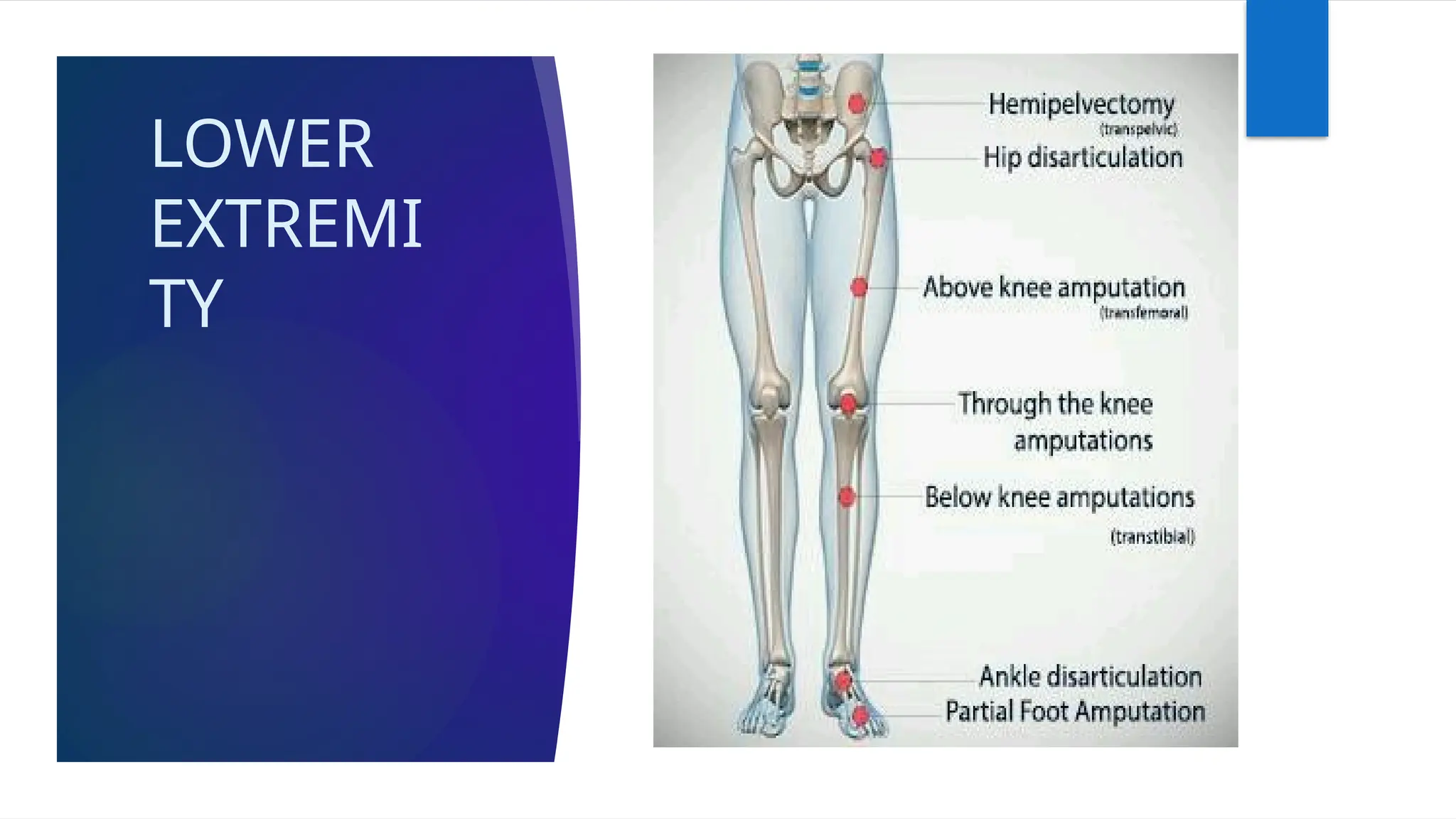
Amputation is the surgical removal of a limb, performed for various life-threatening conditions, injuries, or diseases. It can greatly impact a person's life and necessitates comprehensive management and rehabilitation, including physiotherapy, to ensure optimal recovery and adaptation to prosthesis. The choice of amputation level and procedure depends on factors such as the cause of amputation, vascular supply, and the potential for functional prosthetic fitting.

![ Peripheral vascular insufficiency –Irreversible loss of vascularity to limb
due to disease like diabetes, Berger disease, atherosclerosis,
embolism, arterial thrombosis, arteriovenous aneurysm or trauma
[lead to gangrene]. Advance in arterial in arterial surgery decreased
incidence of amputation
Congenital absence of limb or malformation –There may be incidence of
rudimentary limb structure proximally with apparently normal
terminal segment. Bilateral rudimentary distal segment amputee
managed with bilateral orthosis designed to accommodate deformity .
But when rudimentary portion of limb interfere with fitting of
prosthesis , amputation become necessary](https://image.slidesharecdn.com/amputation-250121044534-ed8642c0/75/AMPUTATION-AND-ROLE-OF-PHYSIOTHERAPY-PPT-9-2048.jpg)