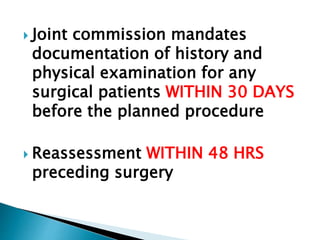
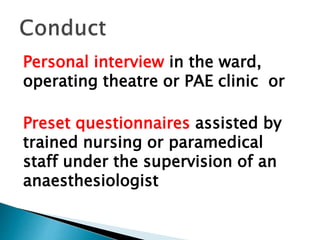
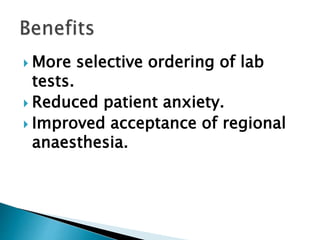
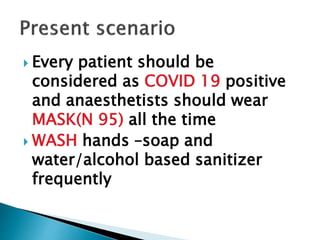
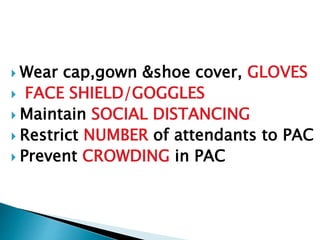
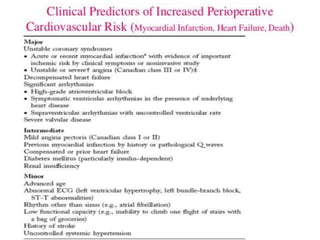
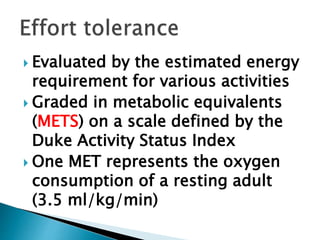
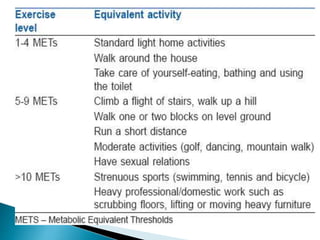
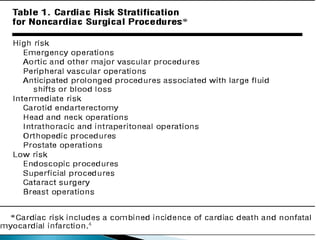
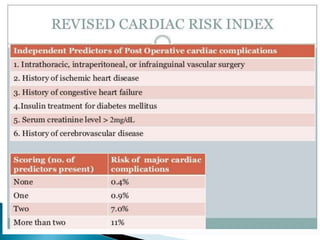
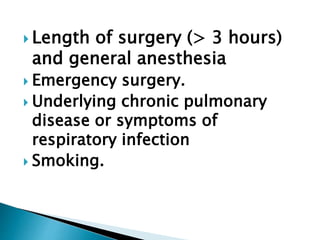
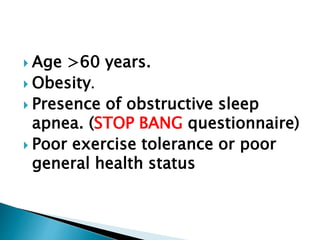
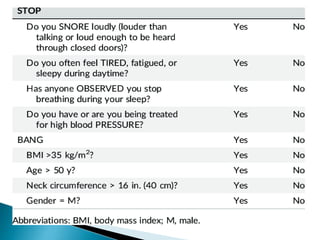
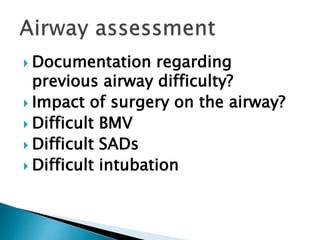
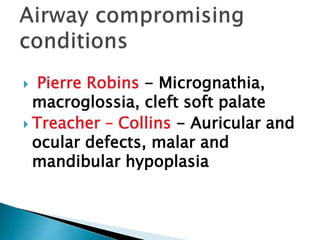
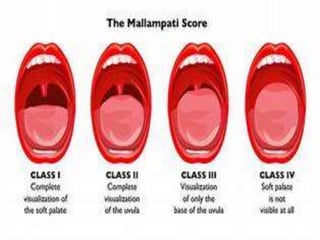
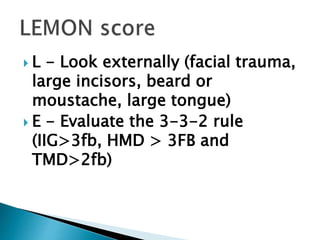
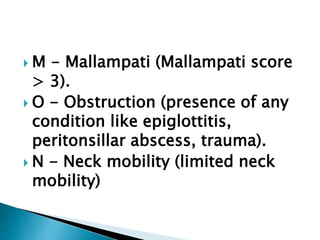
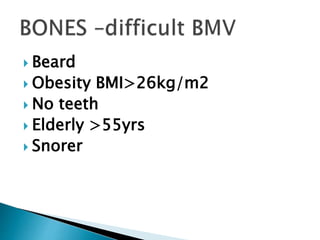
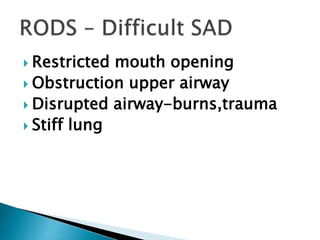
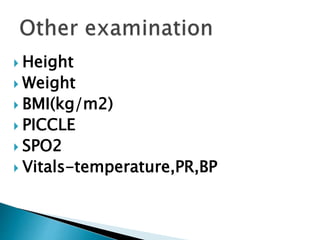
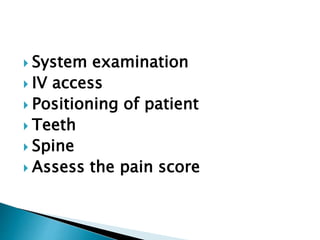
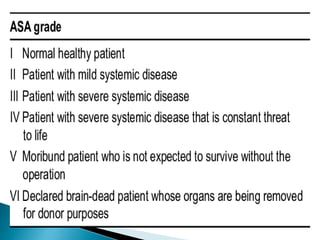
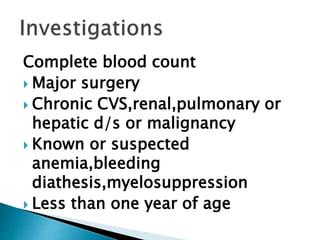
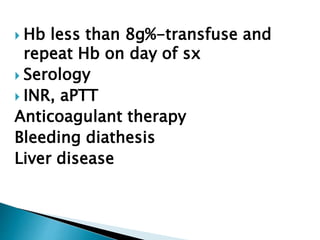
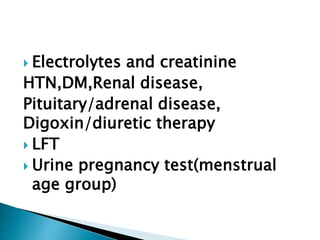
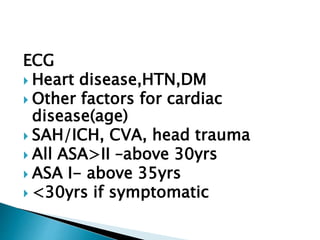
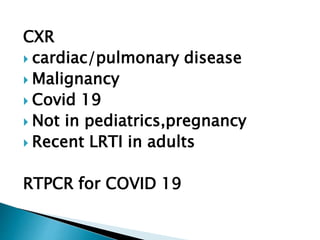
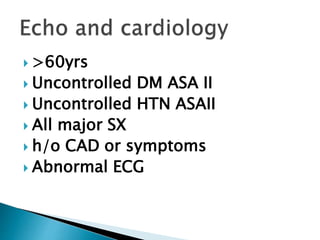
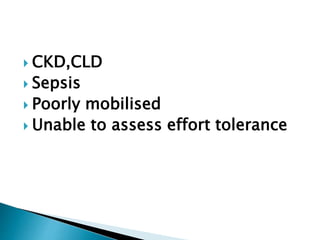
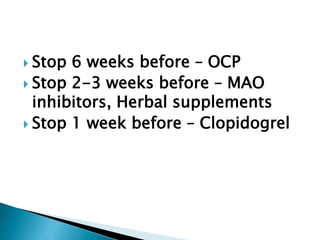
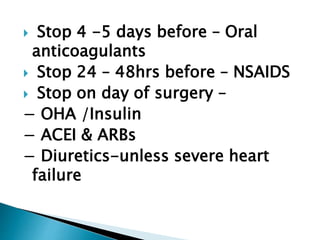
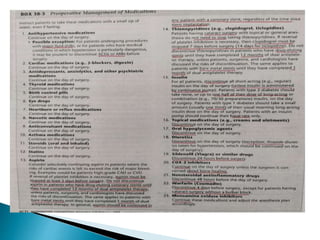
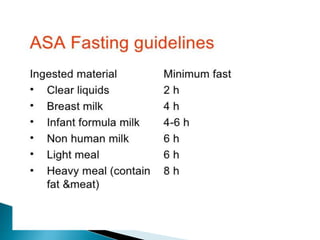
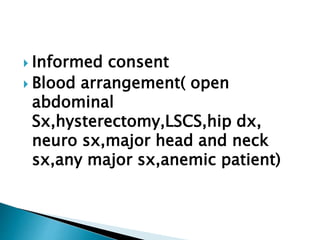
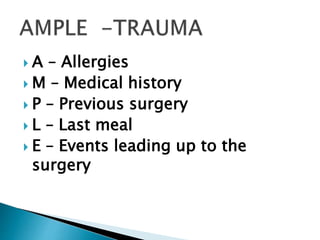
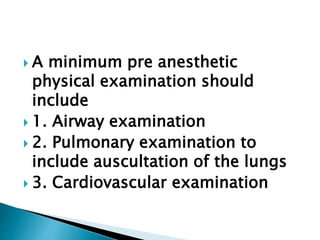
This document discusses guidelines for pre-anesthesia evaluation (PAE). It outlines the components of a PAE, including history taking, physical examination, and relevant investigations. It emphasizes assessing risk factors for perioperative complications, especially related to cardiovascular and pulmonary systems. Modifications to PAE processes during the COVID-19 pandemic are also reviewed, such as taking precautions like masks and distancing.