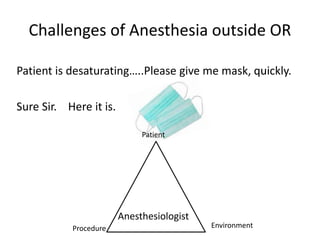
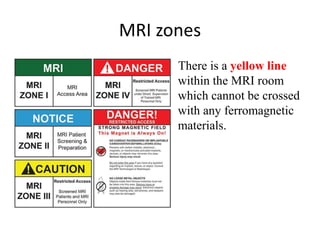
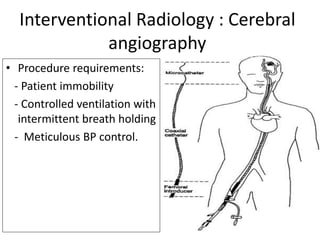
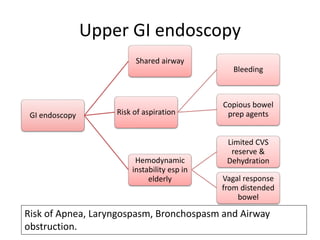
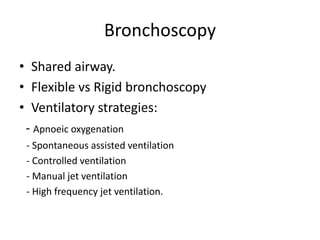
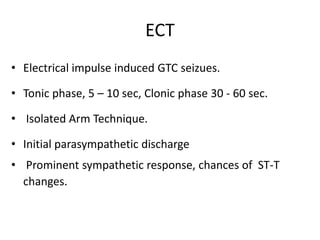
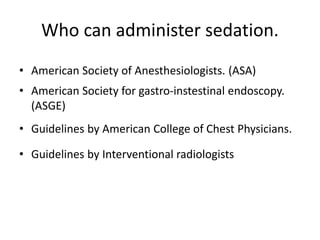
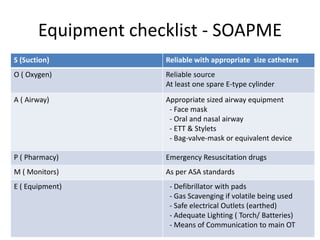
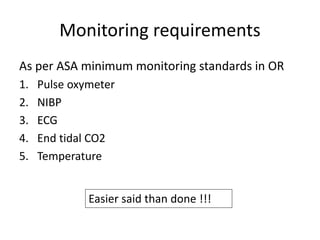
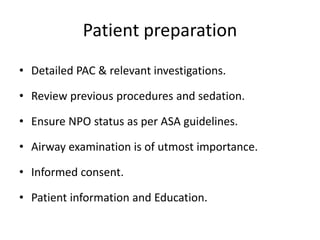
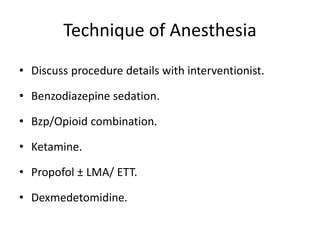
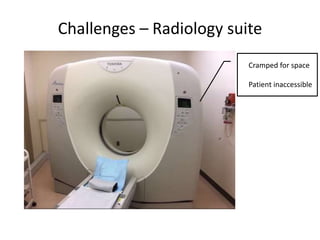
The document discusses anesthesia and sedation practices in offsite locations, emphasizing the importance of safety, effective monitoring, and the unique challenges faced in various environments such as radiology and interventional suites. Key challenges include limited access for anesthesiologists, unfamiliar equipment, and the need for specific preparations for each procedure. It also outlines safety measures and best practices to enhance patient care during these high-risk procedures.