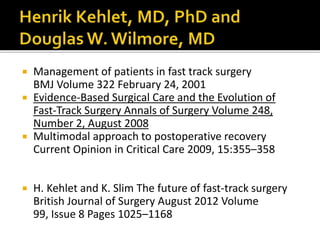
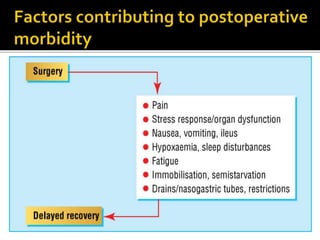
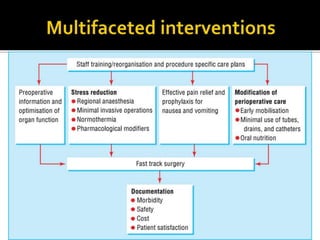
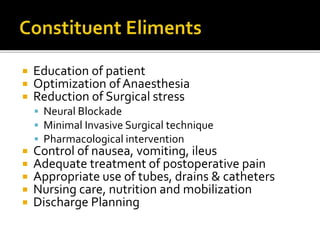
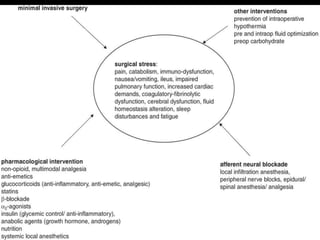
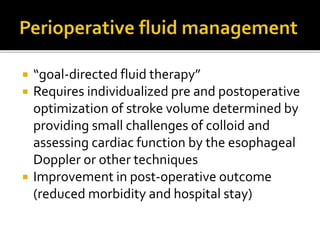
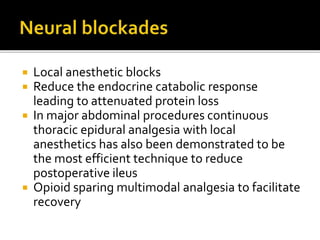
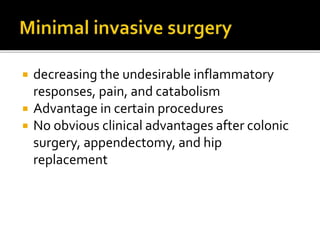
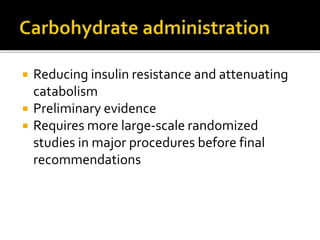
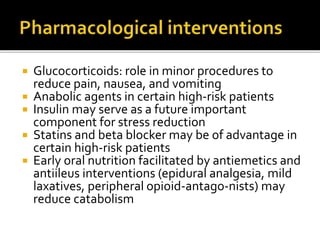
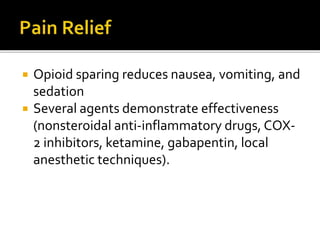
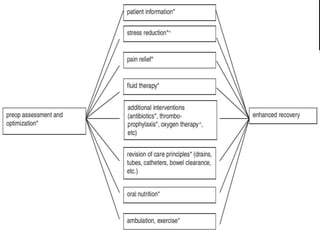
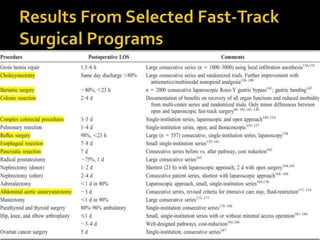
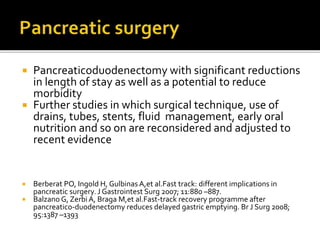
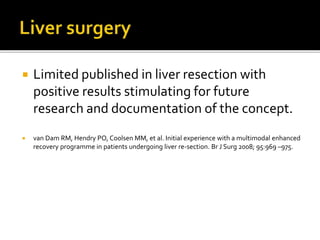
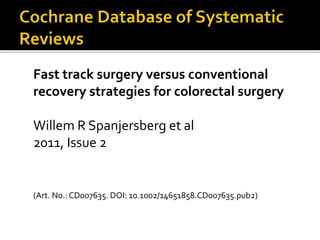
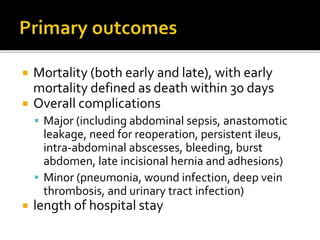
The document discusses the evolution and implementation of fast-track surgery, emphasizing a multimodal approach involving interdisciplinary care to improve recovery outcomes by reducing surgical stress and enhancing patient satisfaction. Key strategies include minimizing invasiveness, optimizing pain management, and facilitating early nutrition and mobilization, which collectively lead to decreased length of hospital stay and postoperative complications. However, there are calls for more extensive research to establish protocols and confirm the effectiveness of specific interventions in various surgical contexts.
![ Fast track surgery combines various
techniques used in the care of patients
undergoing elective operations
epidural or regional anesthesia
minimally invasive techniques
optimal pain control
aggressive postoperative rehabilitation
[early enteral (oral) nutrition and ambulation]](https://image.slidesharecdn.com/fasttrack-200617125543/85/Fast-track-6-320.jpg)