This document provides guidance on various nursing skills related to ambulation, patient transfers, range of motion exercises, and restraints. Key points include:
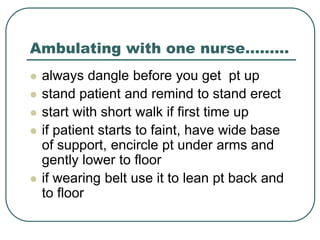
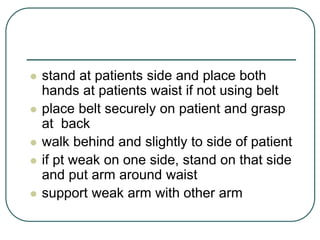
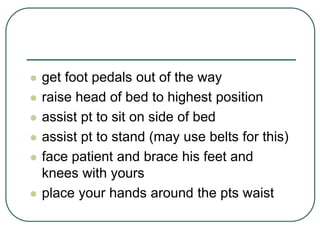
- Assess patient's capabilities and explain the plan before ambulating or transferring a patient
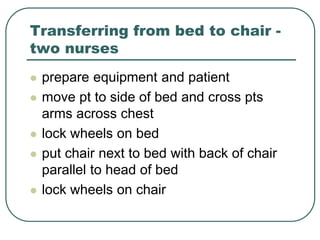
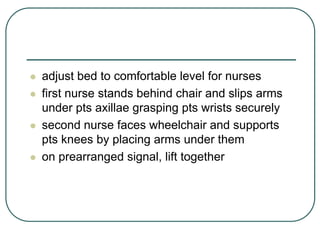
- Use proper body mechanics and any necessary equipment to move patients safely
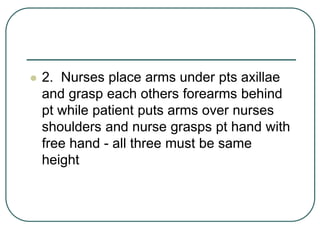
- For ambulation, two nurses can support the patient under the arms or each take an arm
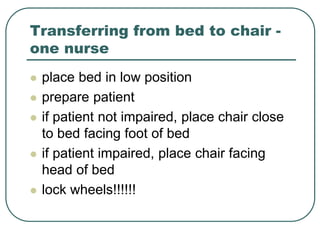
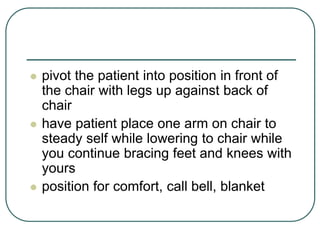
- When transferring from bed to chair, position the chair close to the bed and pivot the patient while bracing their legs
- Use draw sheets and leverage techniques to transfer a patient from bed to stretcher safely
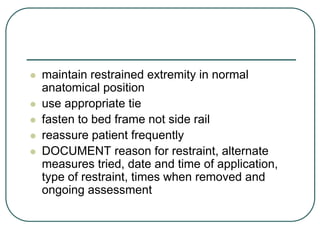
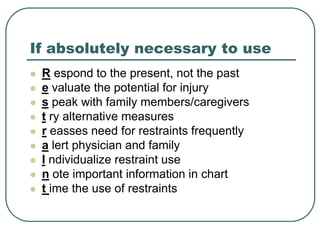
- Obtain a physician's order and use the least restrictive restraints possible, checking the patient regularly