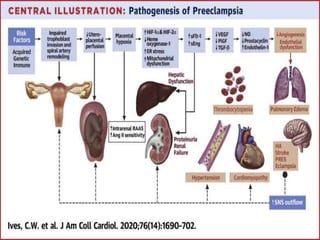
This document provides an overview of preeclampsia and eclampsia. It begins with an introduction and outlines risk factors and classifications. It then describes clinical features such as hypertension and proteinuria. The pathophysiology section explains how abnormal placentation leads to reduced blood flow and imbalance of prostaglandins. Complications are also discussed, including renal failure, pulmonary edema, and intrauterine growth restriction. The document provides information on diagnosis and management of preeclampsia and eclampsia.