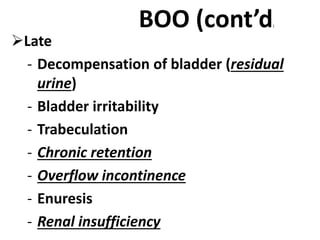
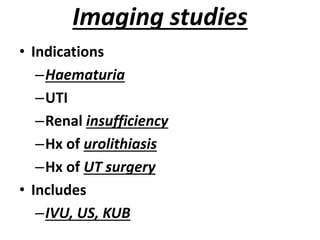
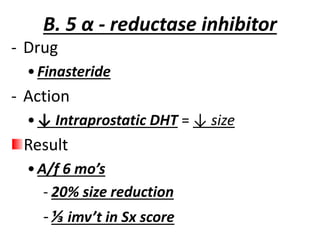
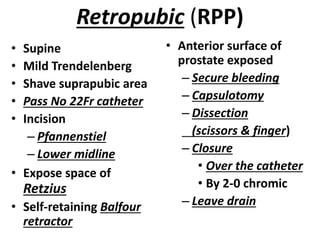
This document summarizes benign prostatic hyperplasia (BPH). It discusses the pathology and pathogenesis of BPH, including that it affects glandular epithelium, stromal cells, and causes increased growth. It also covers the symptomatology, evaluation, and various treatment options for BPH including watchful waiting, medical therapy, and prostatectomies. Surgical treatments discussed are transurethral resection of the prostate (TURP), retropubic prostatectomy (RPP), and transvesical prostatectomy (TVP).






![Patho (cont’d)
• Androgen receptors
- Pst responds to androgen through out life
- ↑ in age
↑ in estrogen
↓
↑ expression of AR in aging prostate
↓
↑ in pst size despite low serum [ ] of
androgen
↓
maintained androgen dependent cell growth](https://image.slidesharecdn.com/chap-231007095657-4c3b55cf/85/Chap-VII-pptx-7-320.jpg)