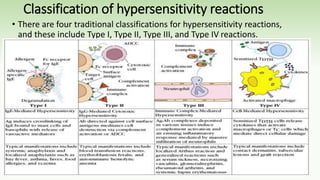
This seminar presentation discusses hypersensitivity reactions, which are exaggerated or inappropriate immune responses to benign antigens. It covers the objectives, mechanisms, classification, complications, and references related to hypersensitivity reactions. There are four main types of hypersensitivity reactions: Type I involves IgE antibodies and mast cell degranulation, Type II involves antibody-mediated cell cytotoxicity, Type III involves immune complex formation and deposition, and Type IV involves T-cell mediated reactions. The presentation provides examples and details of each type of hypersensitivity reaction and their clinical implications.