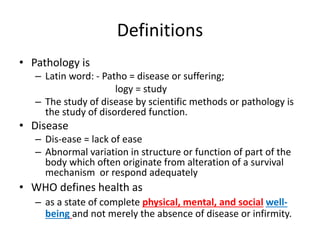
This document provides an introduction to pathology. It defines pathology as the study of disease through scientific methods and examines the mechanisms of disease from etiology to clinical manifestation. The key points are:
1. Pathology studies the etiology, pathogenesis, morphologic changes, and functional derangements that result from disease processes.
2. Diseases are examined through diagnostic techniques including histopathology, cytopathology, and biochemical/immunological testing to identify structural and molecular alterations.
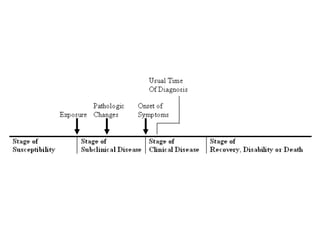
3. The natural course of a disease involves stages from initial exposure through biological onset, clinical onset, potential resolution or death.