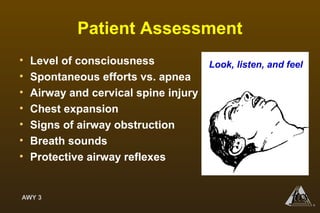
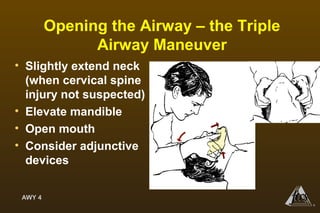
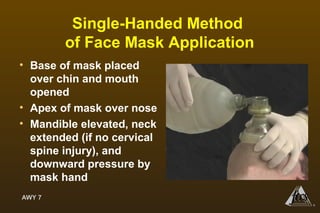
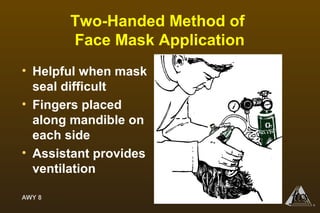
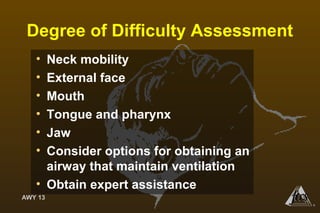
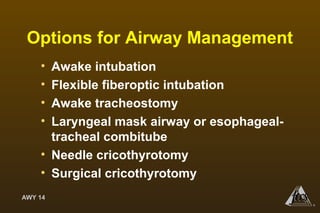
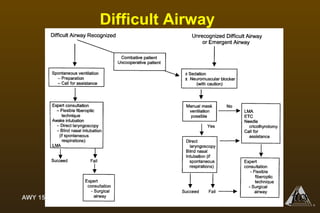
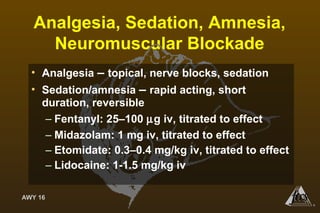
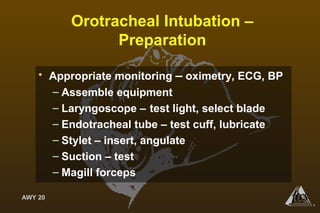
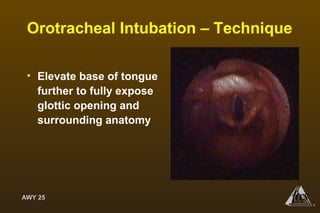
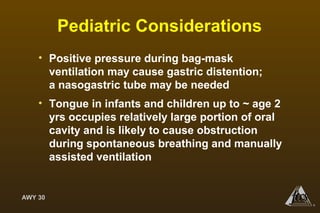
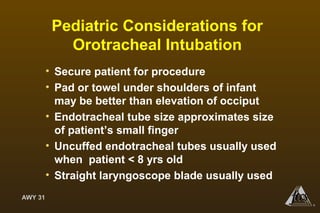
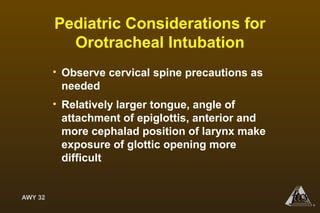
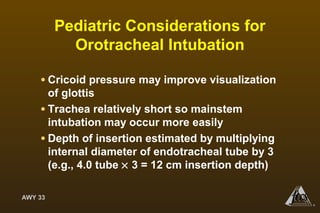
This document provides guidance on airway management techniques. It begins by outlining objectives of airway assessment and various techniques for establishing an airway such as manual ventilation with a face mask, use of airway adjuncts, and endotracheal intubation. Specific steps for patient assessment, opening the airway, reassessment, manual ventilation, and addressing inadequate mask seals are described. Considerations for pediatric patients are also reviewed.