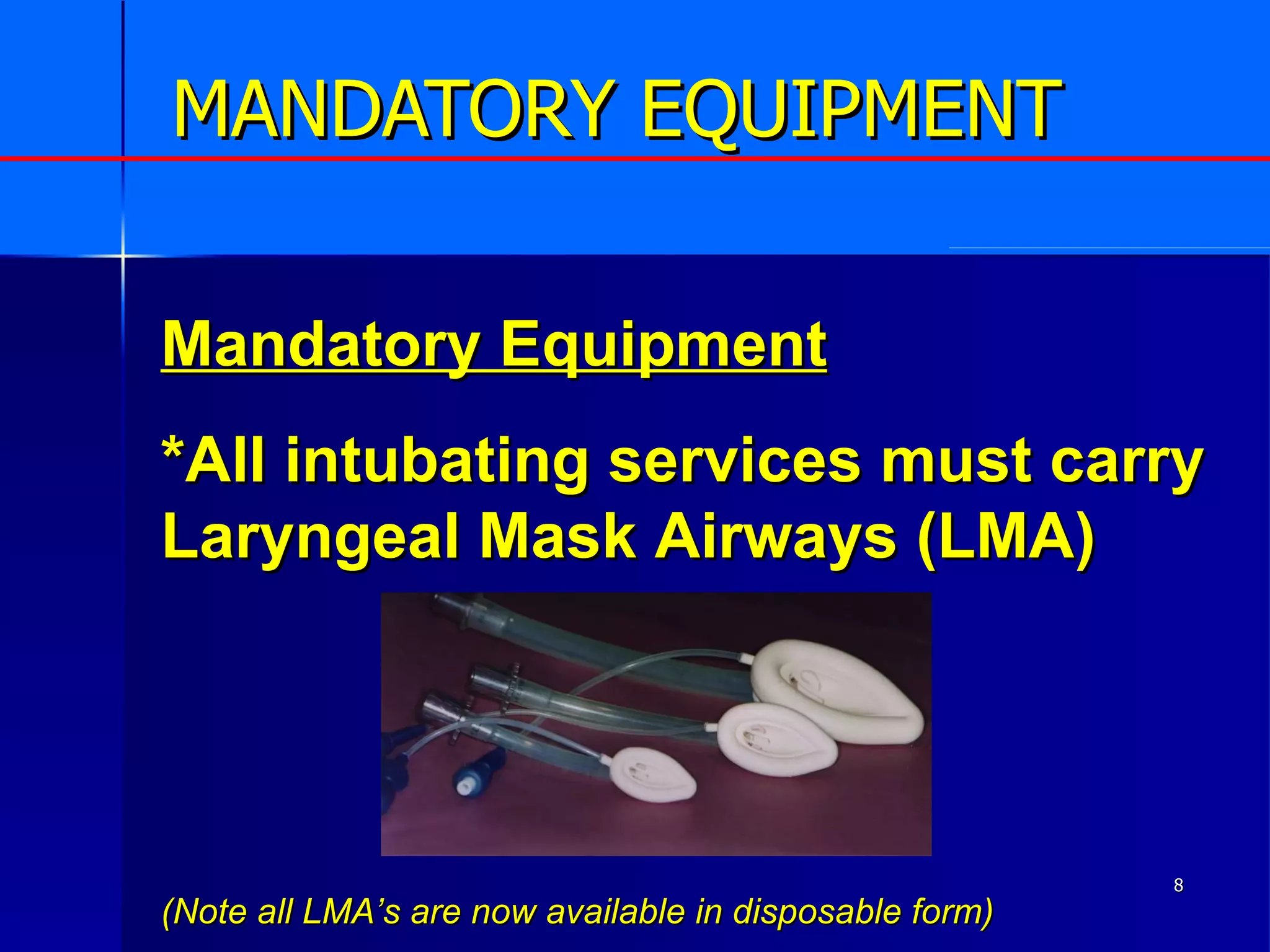
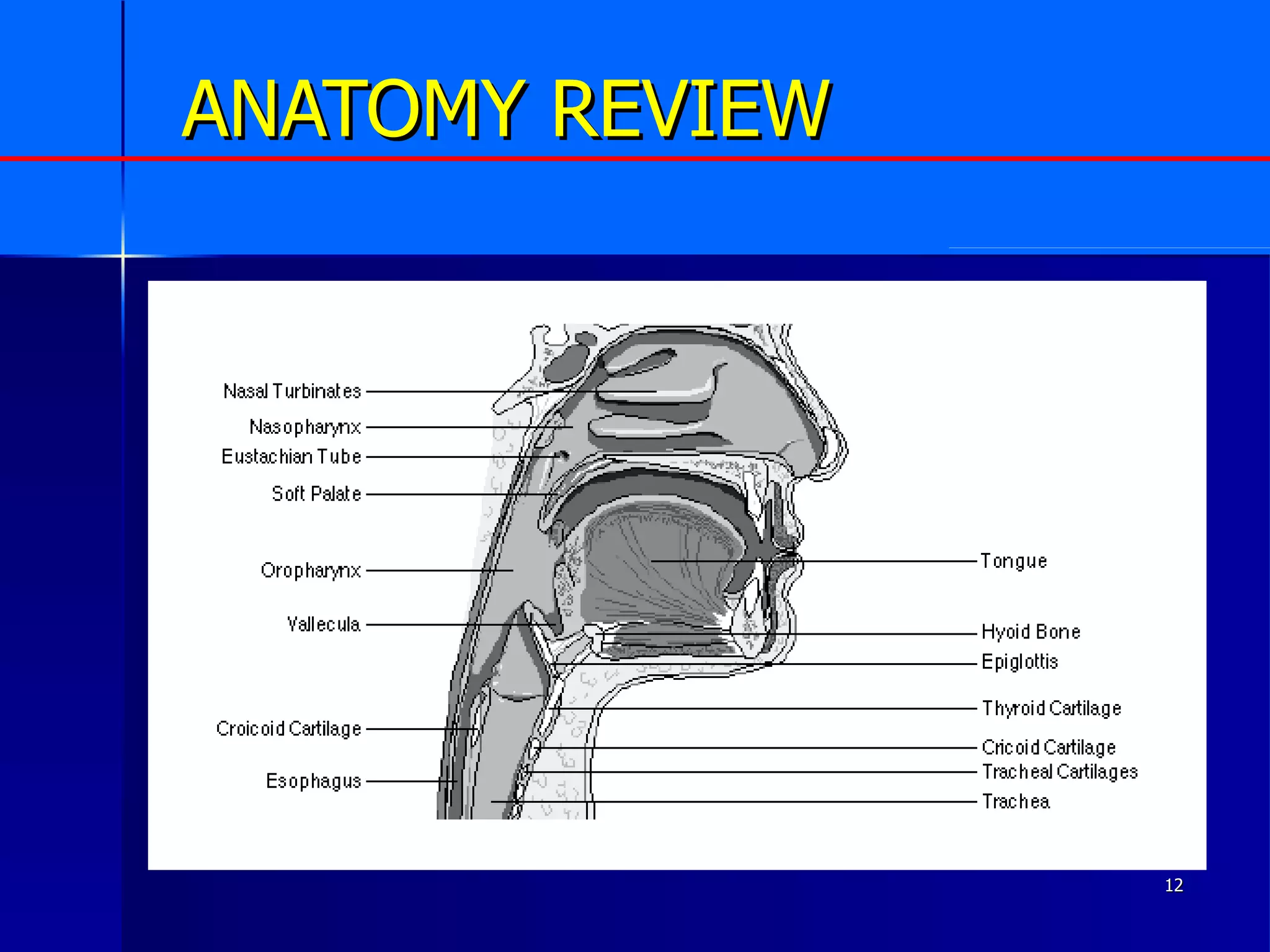
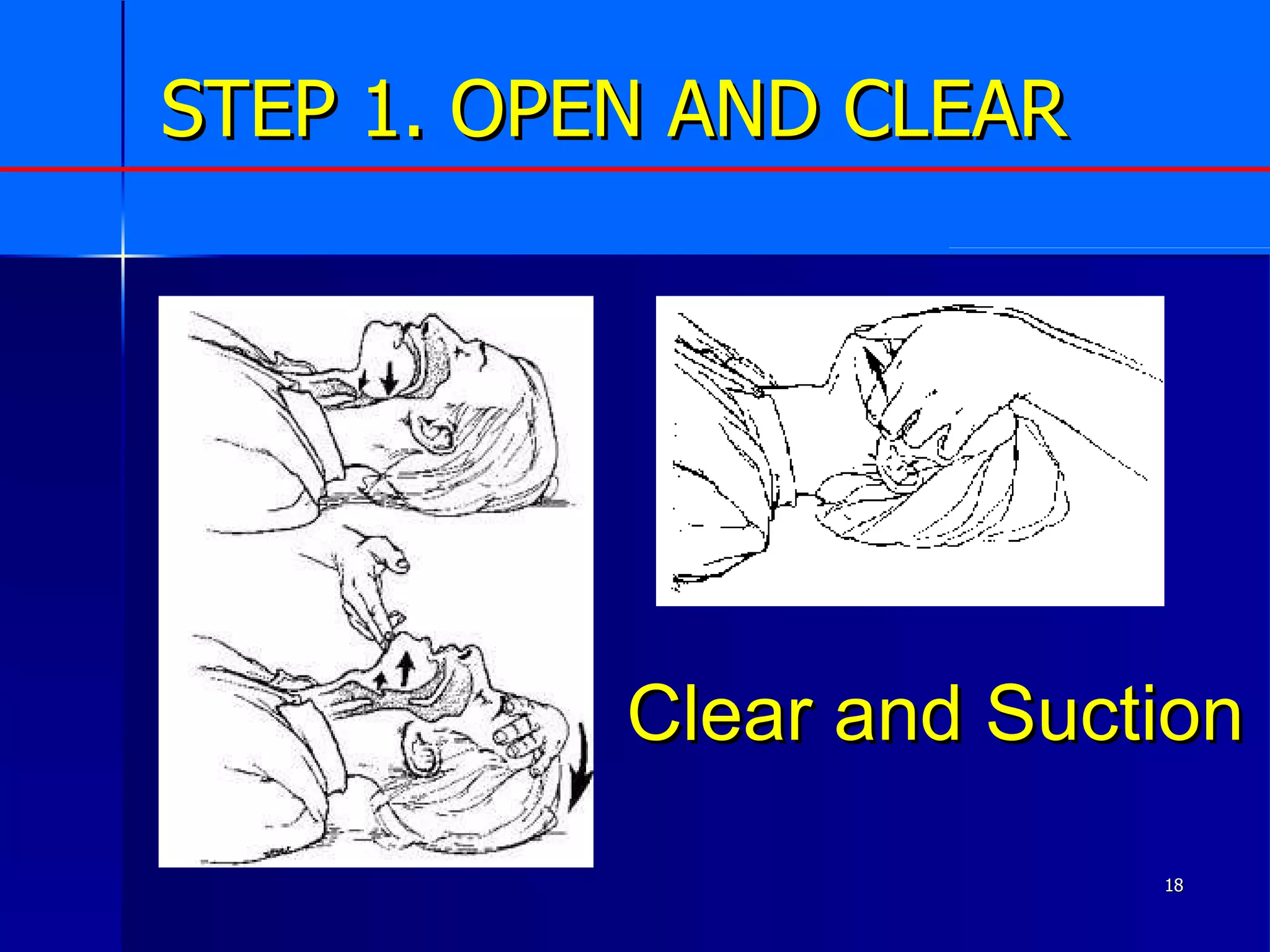
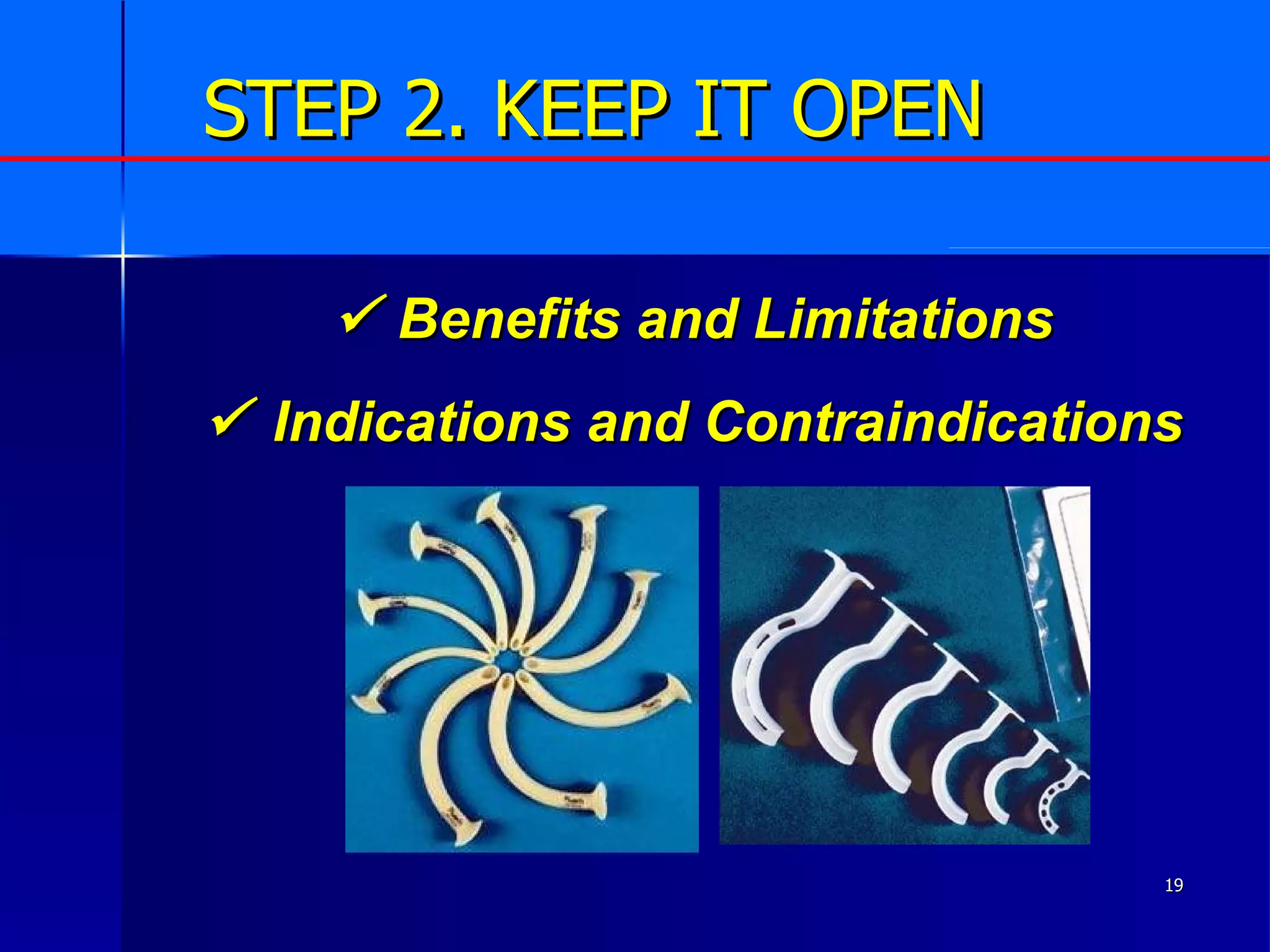
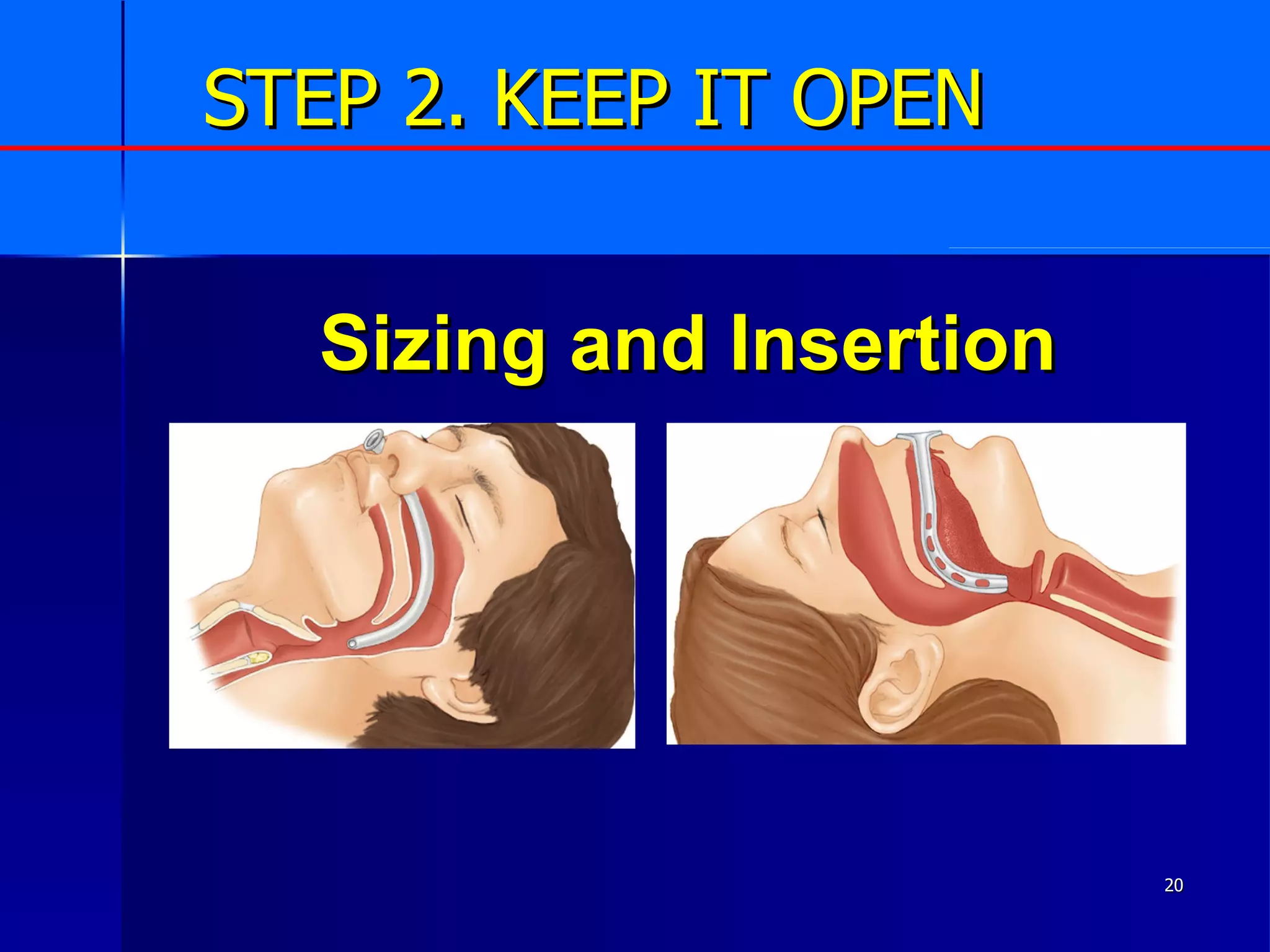
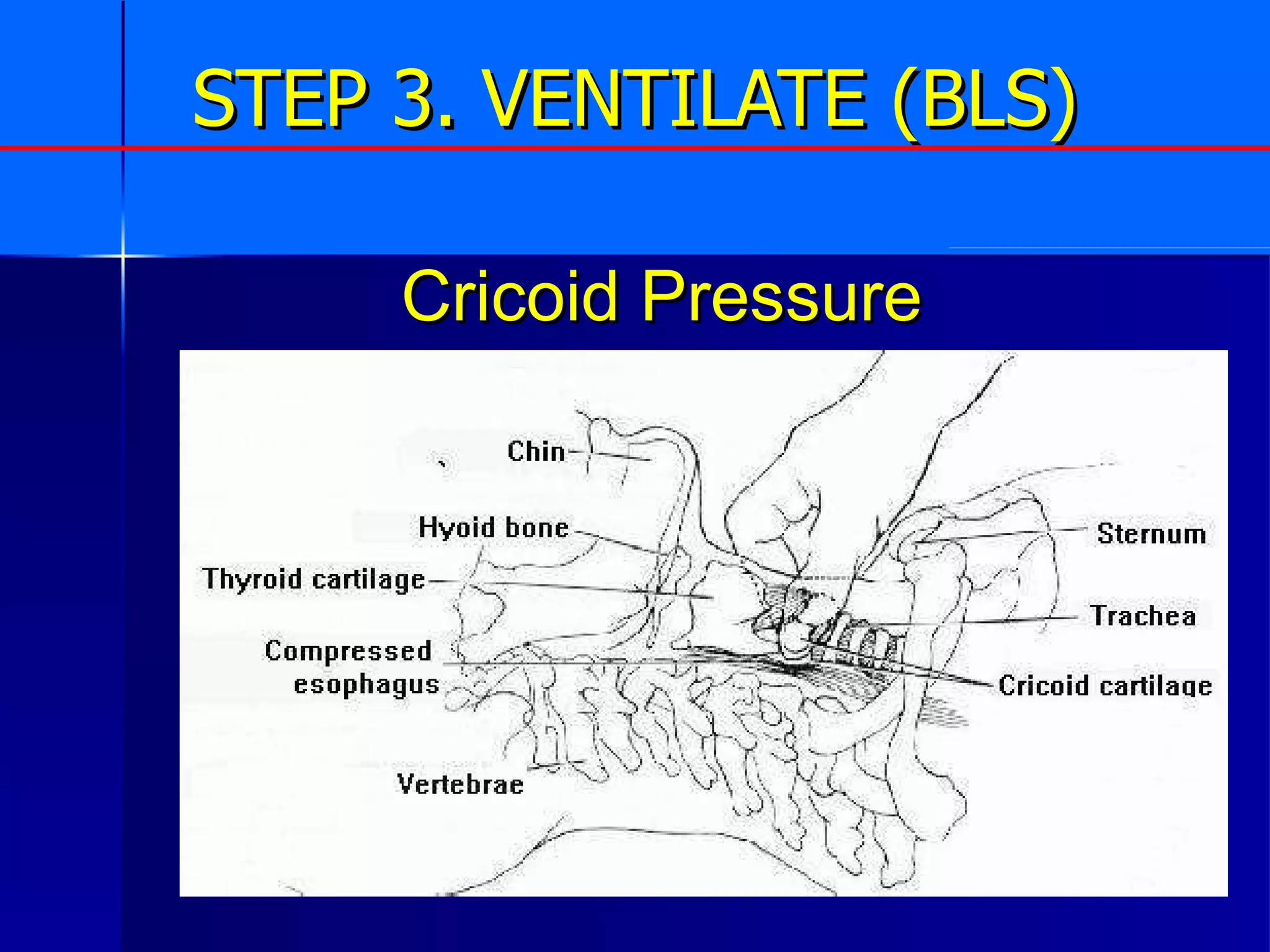
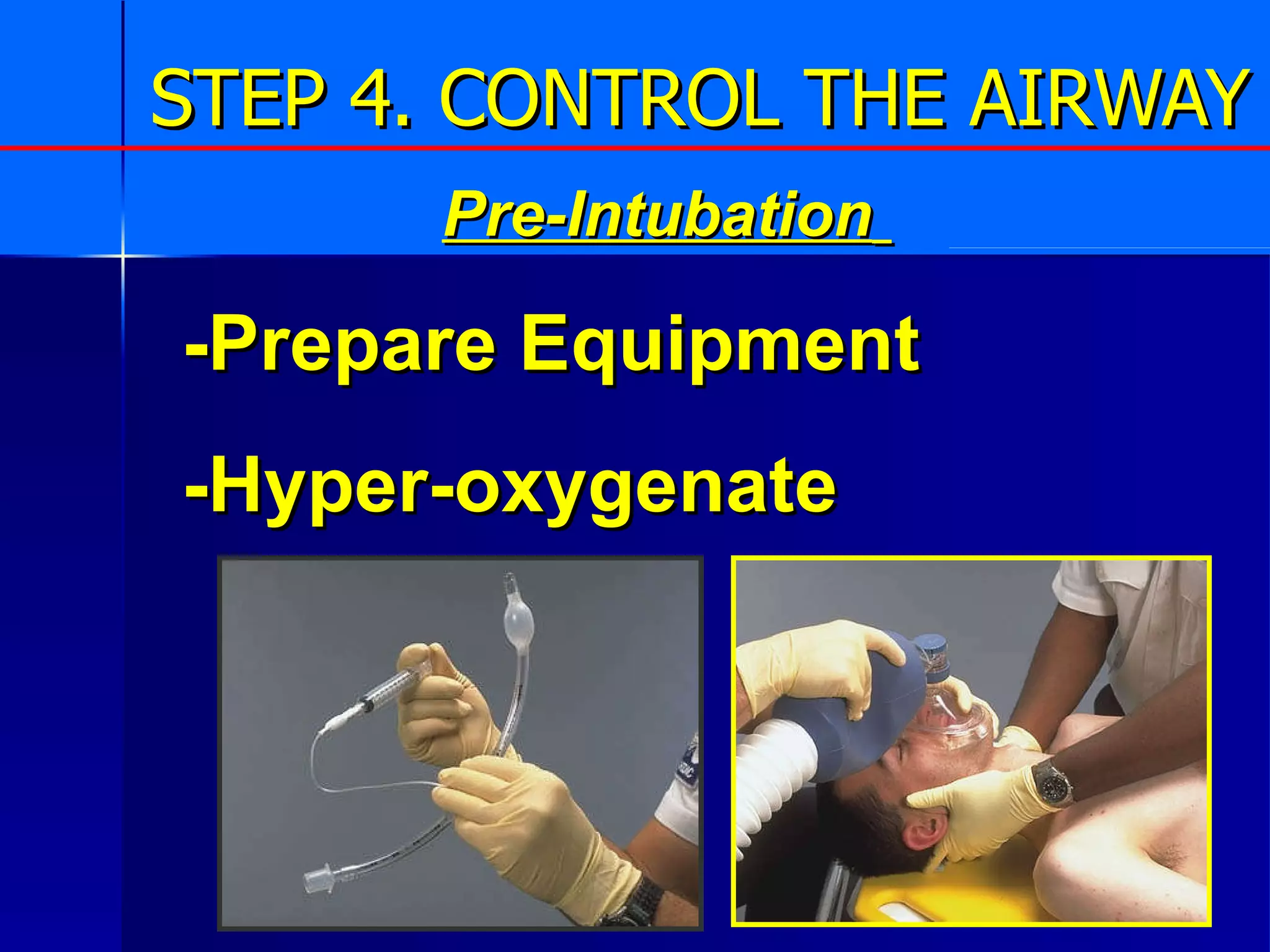
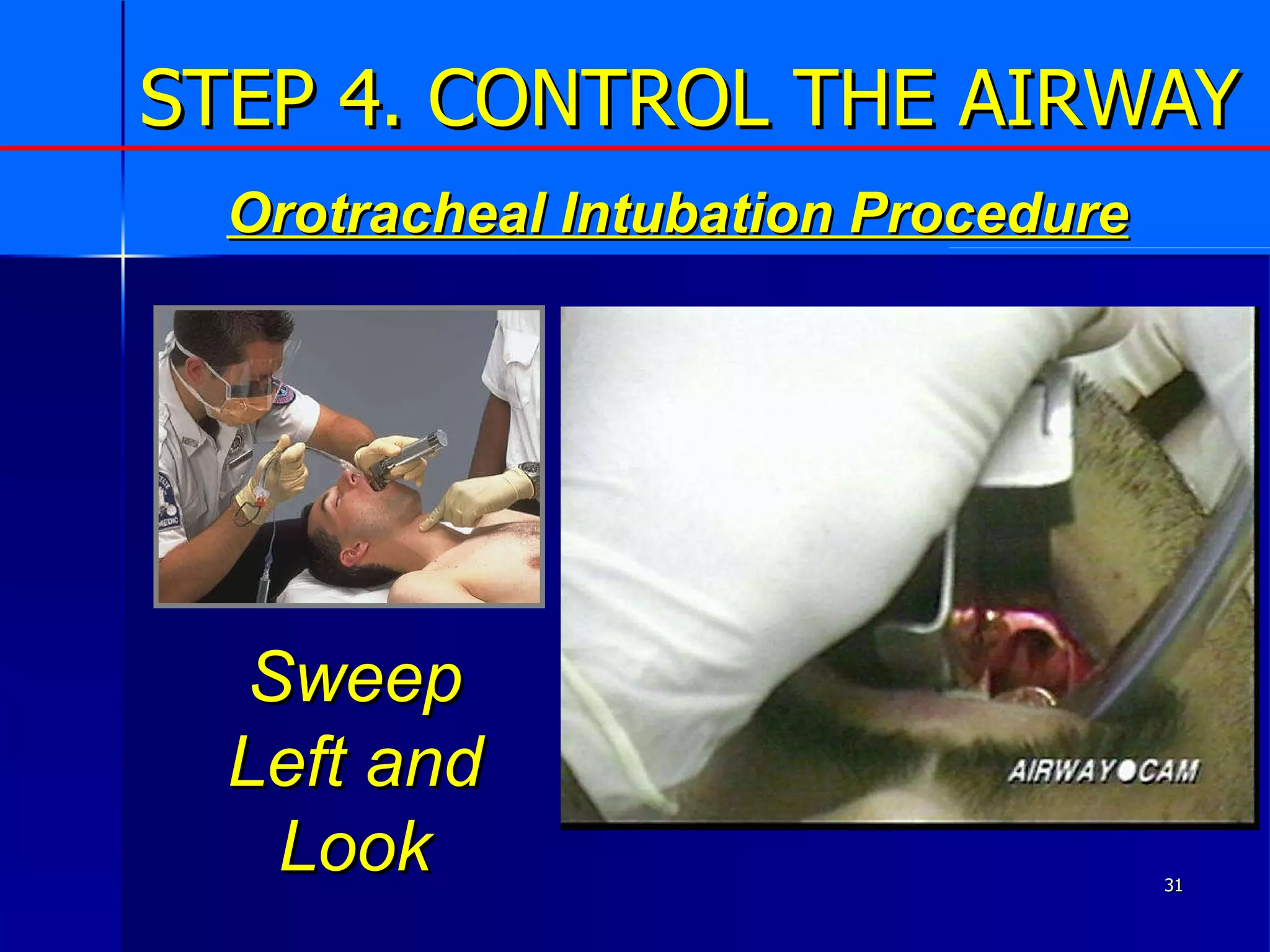
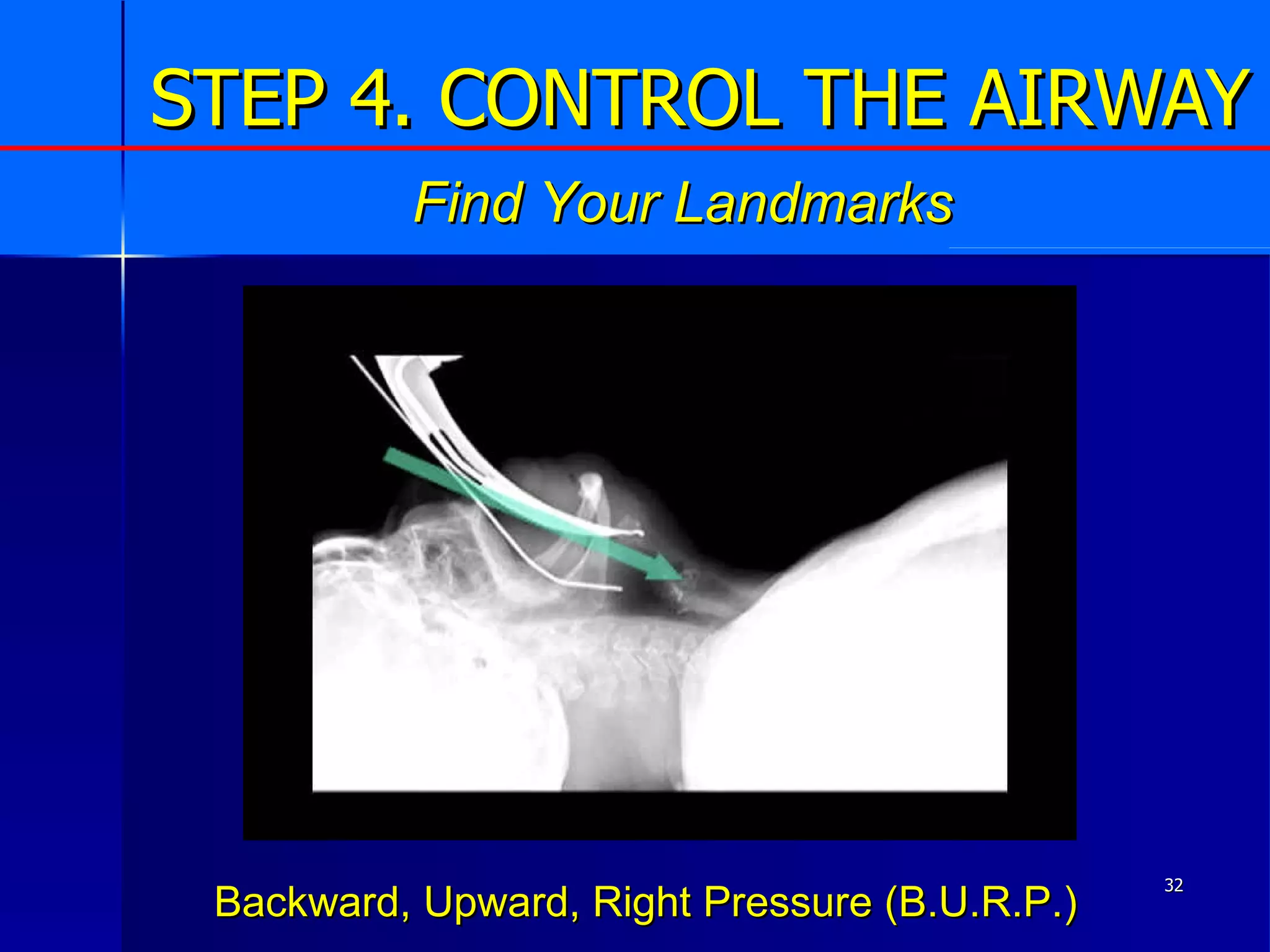
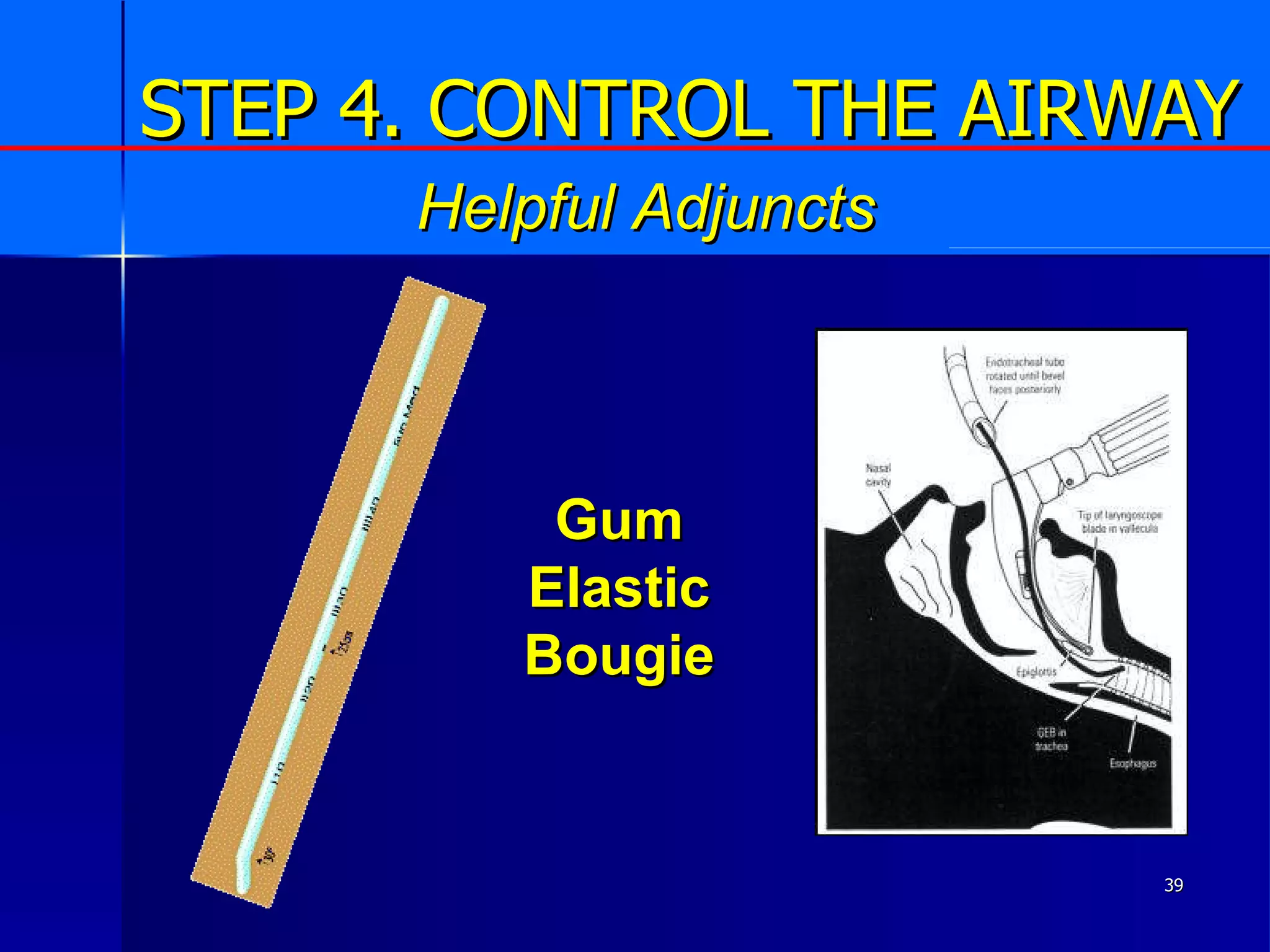
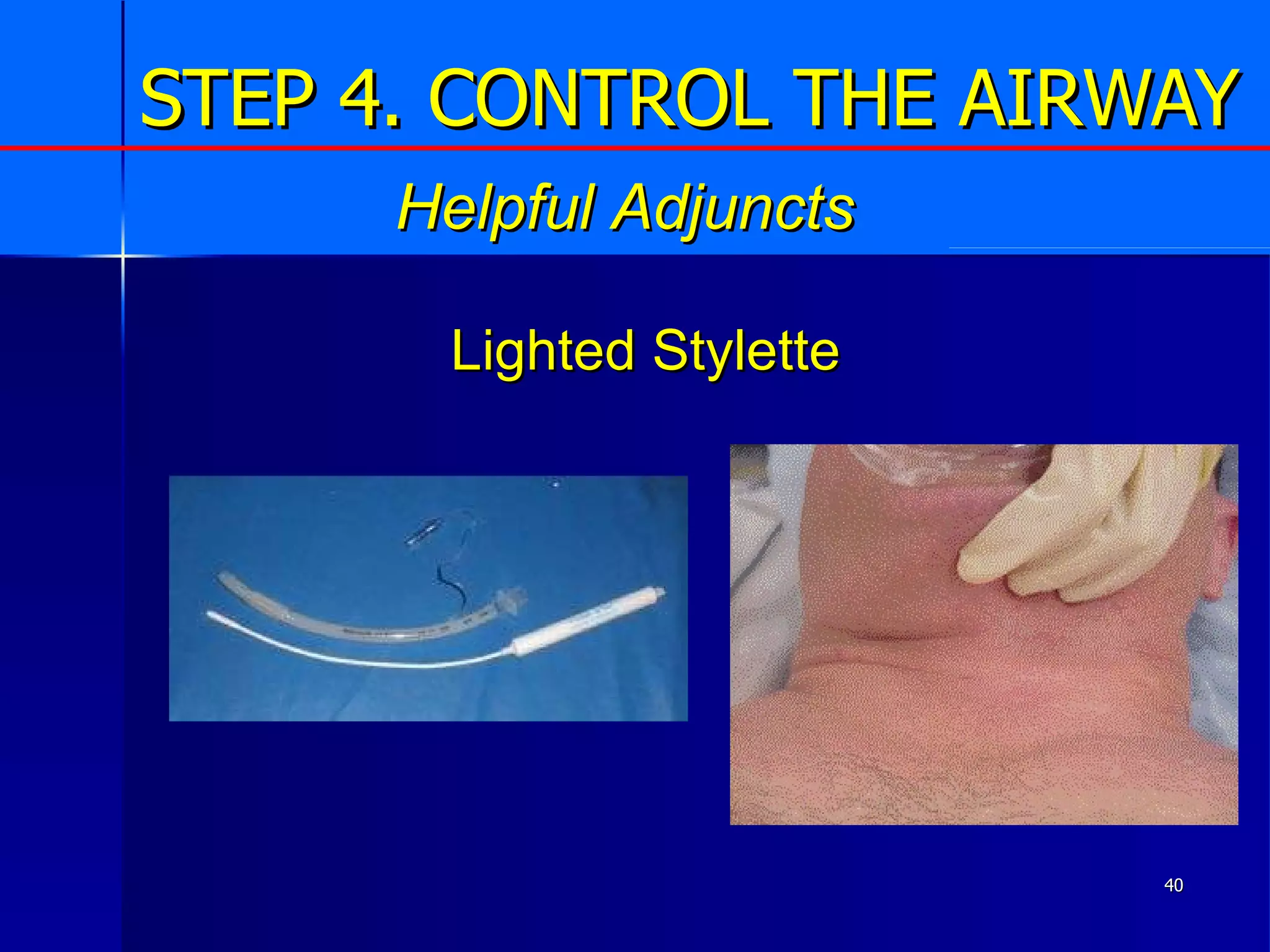
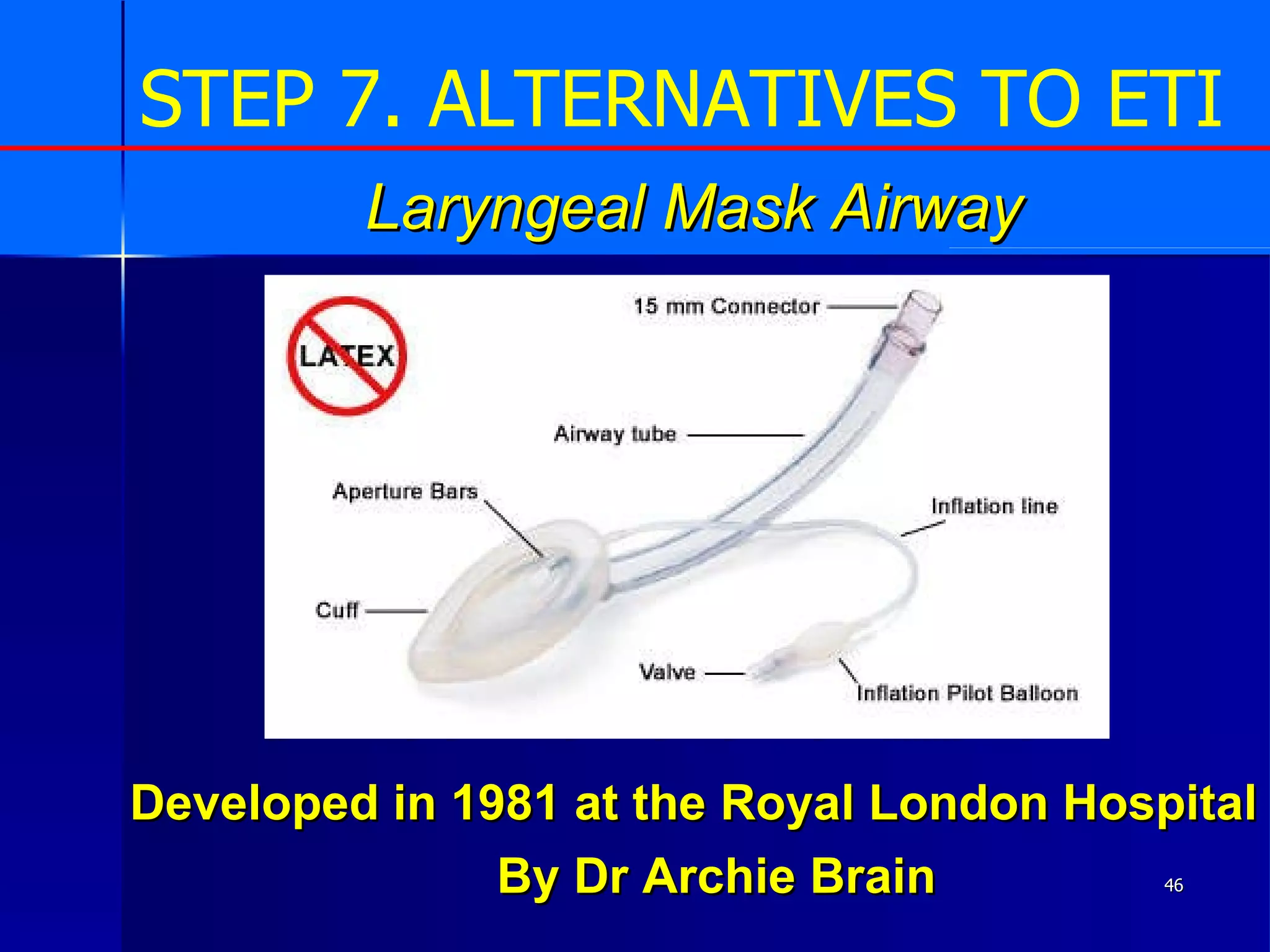
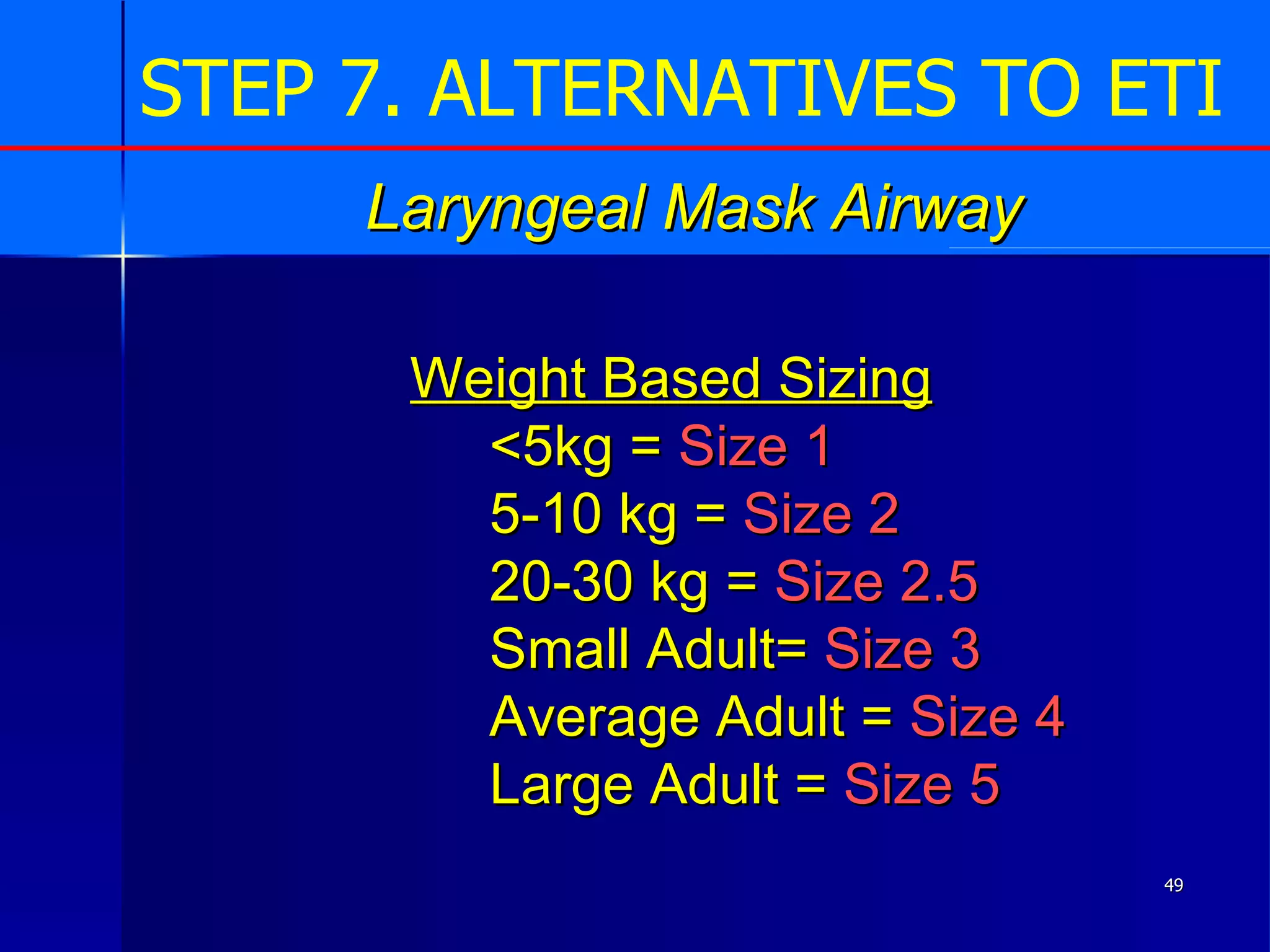
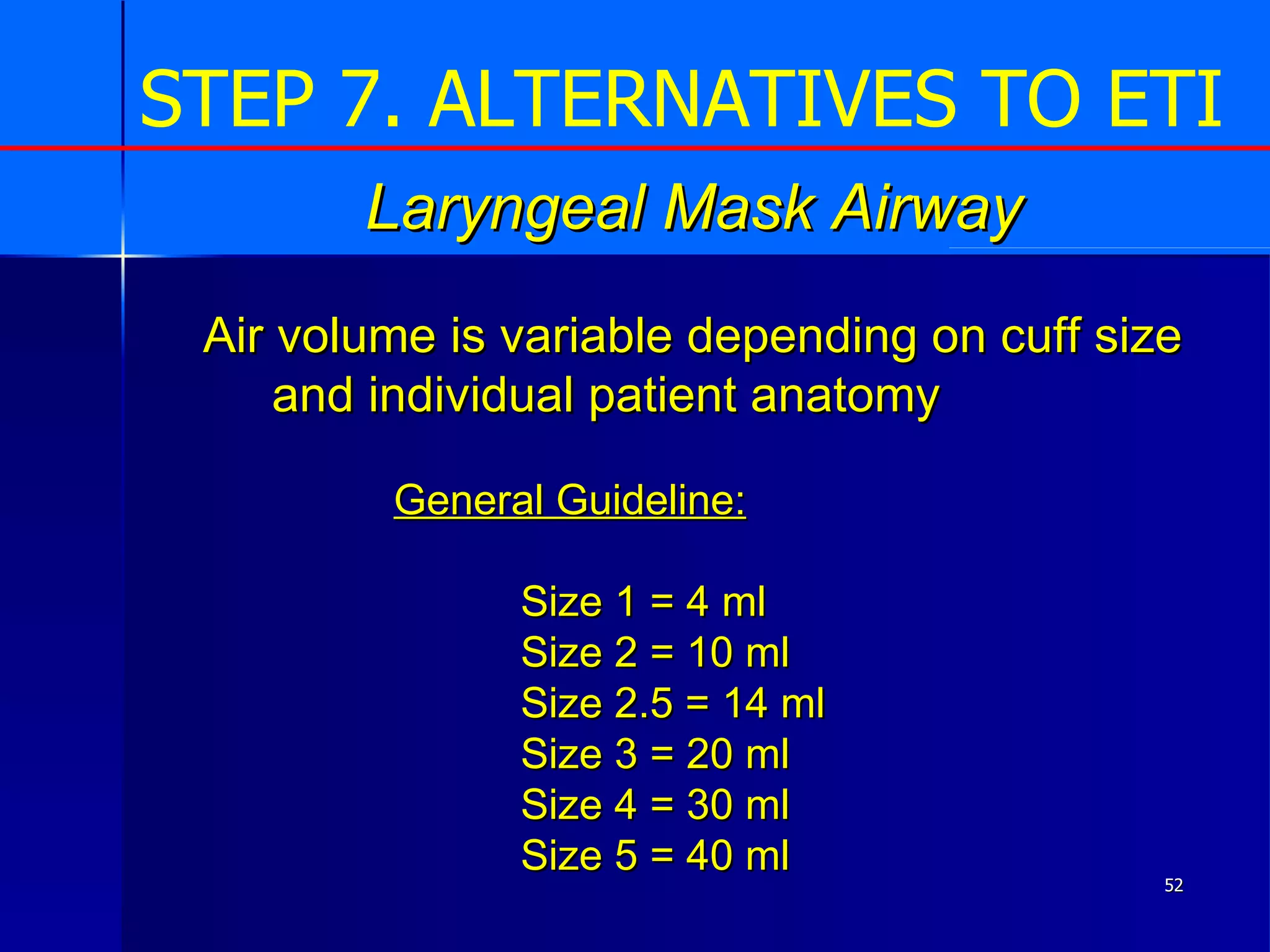
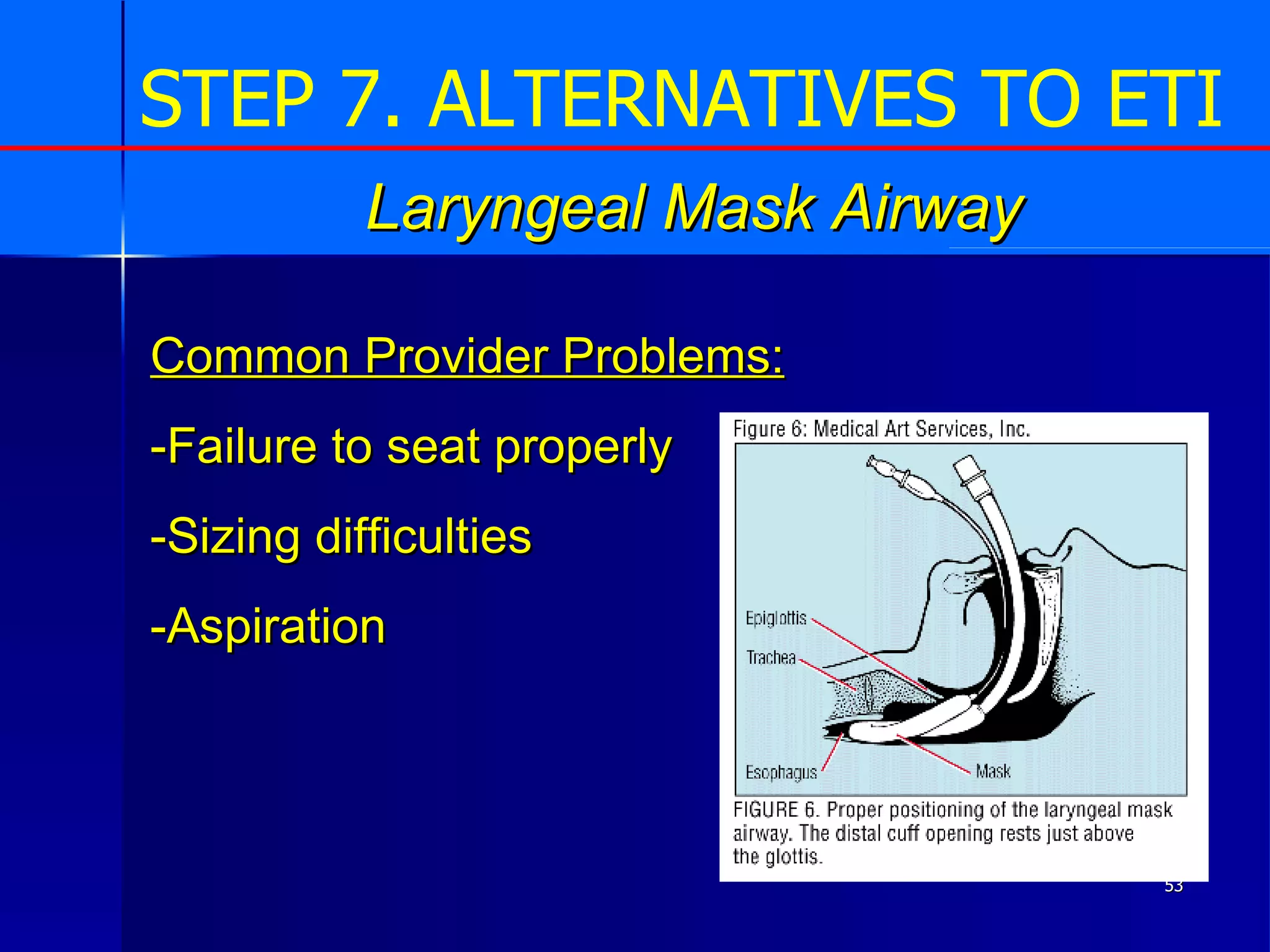
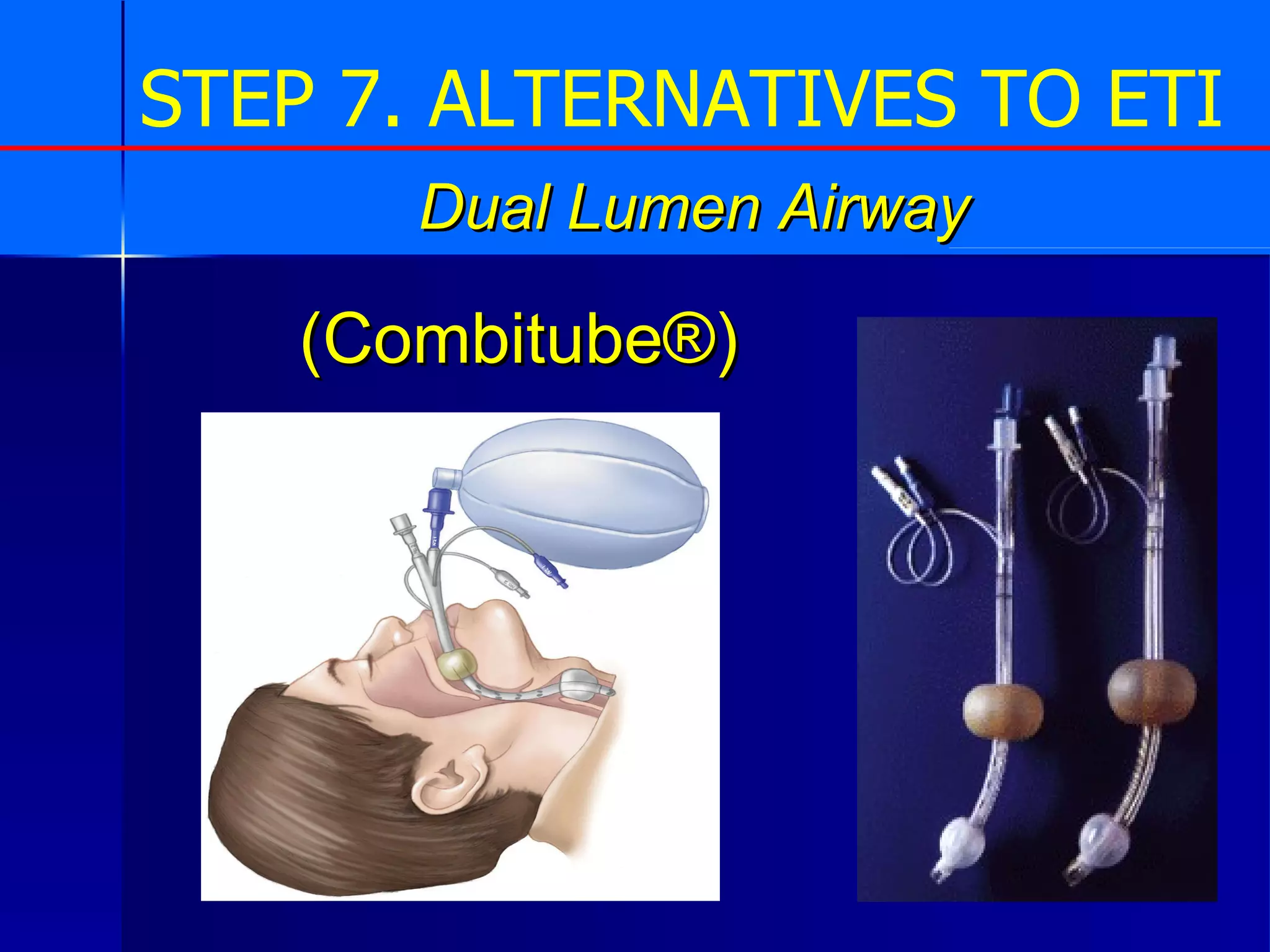
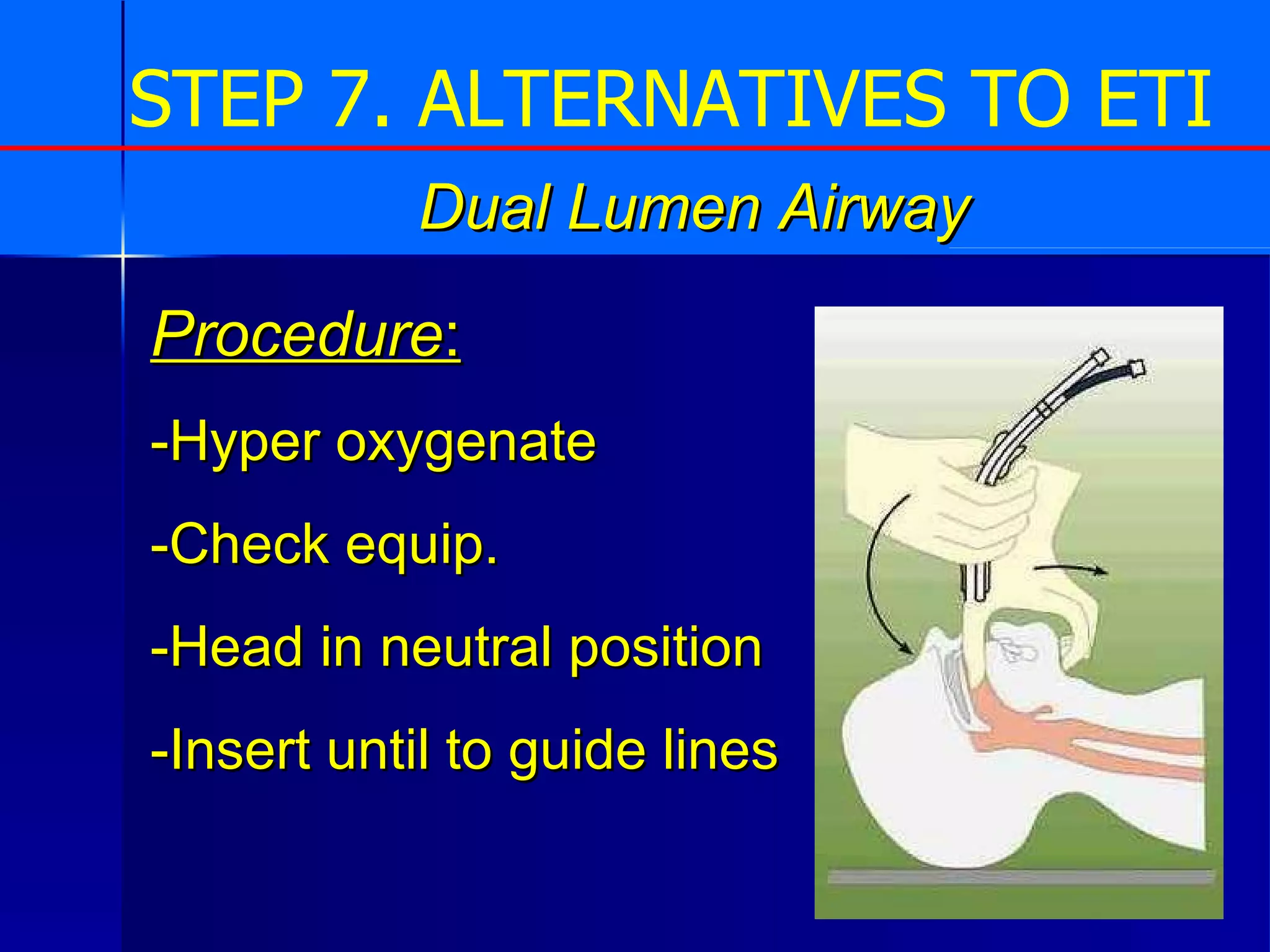
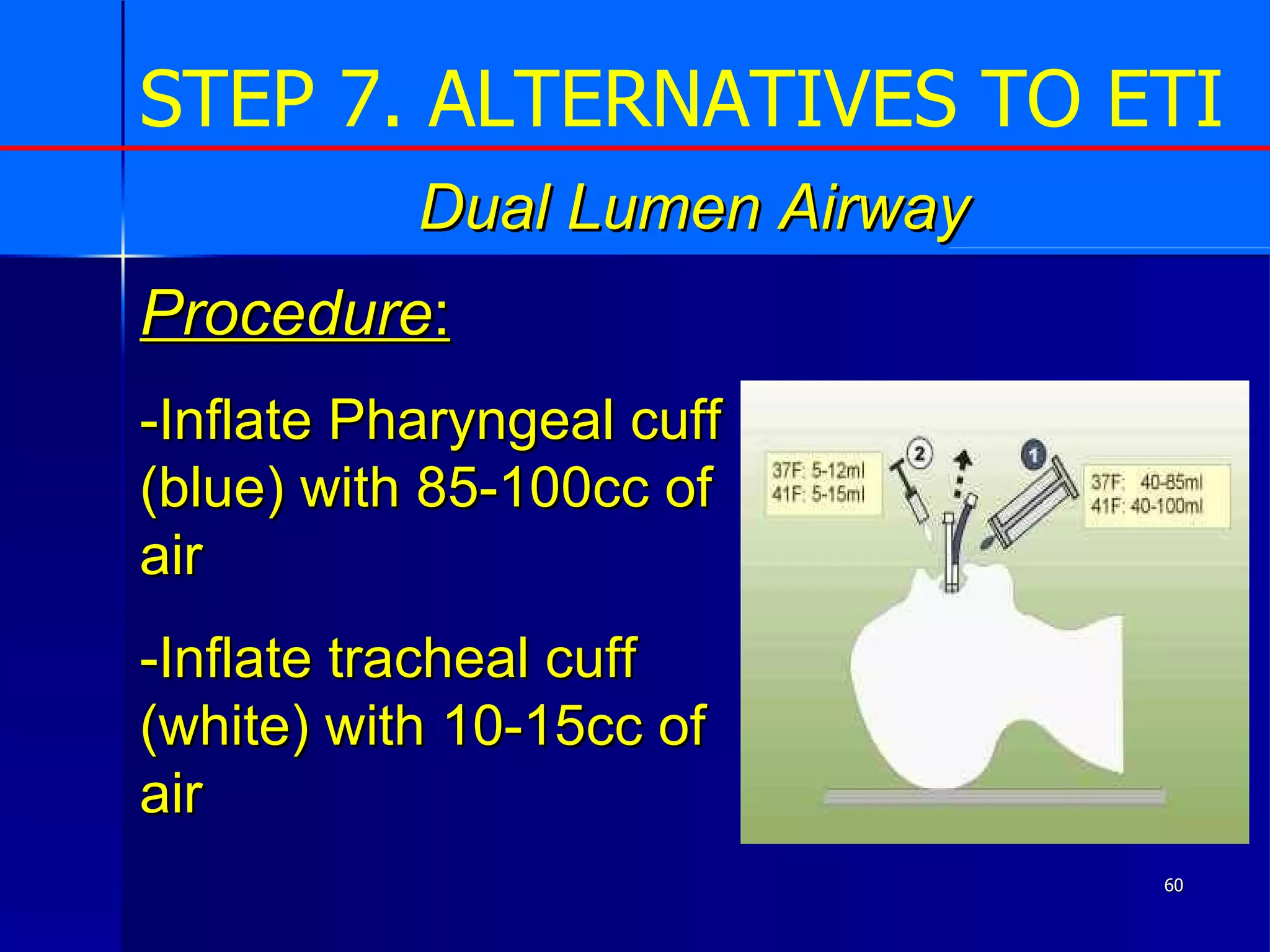
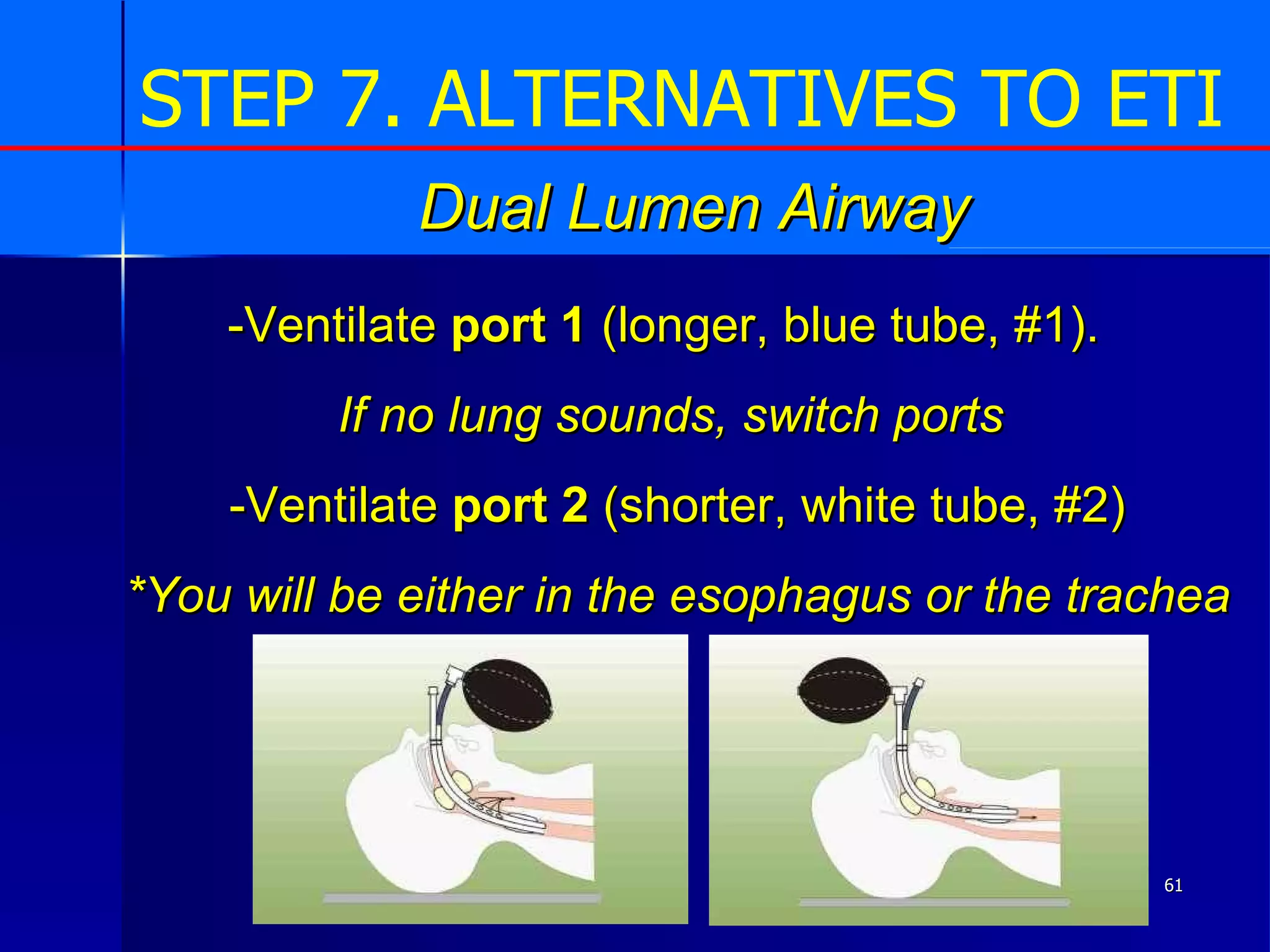
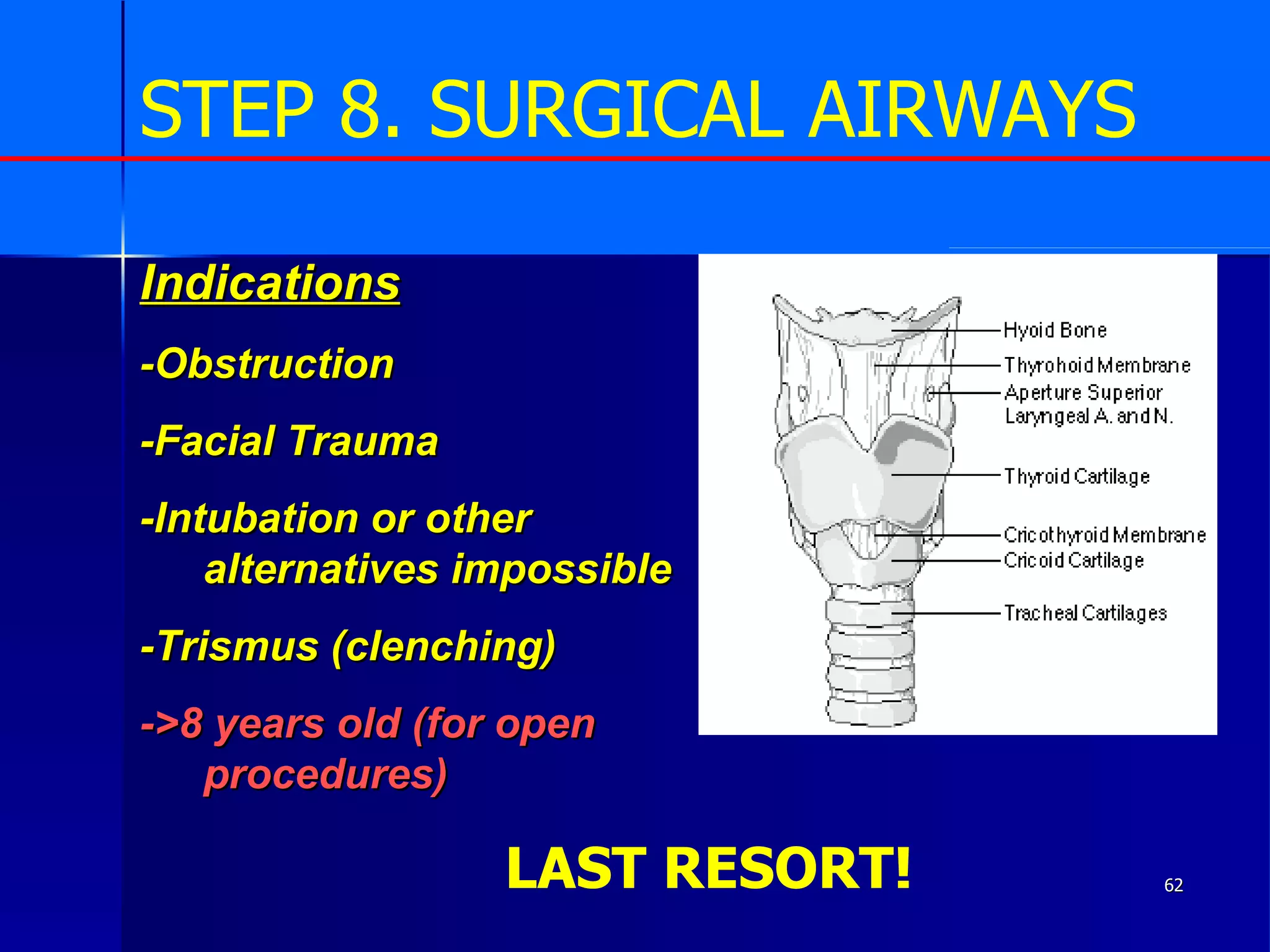
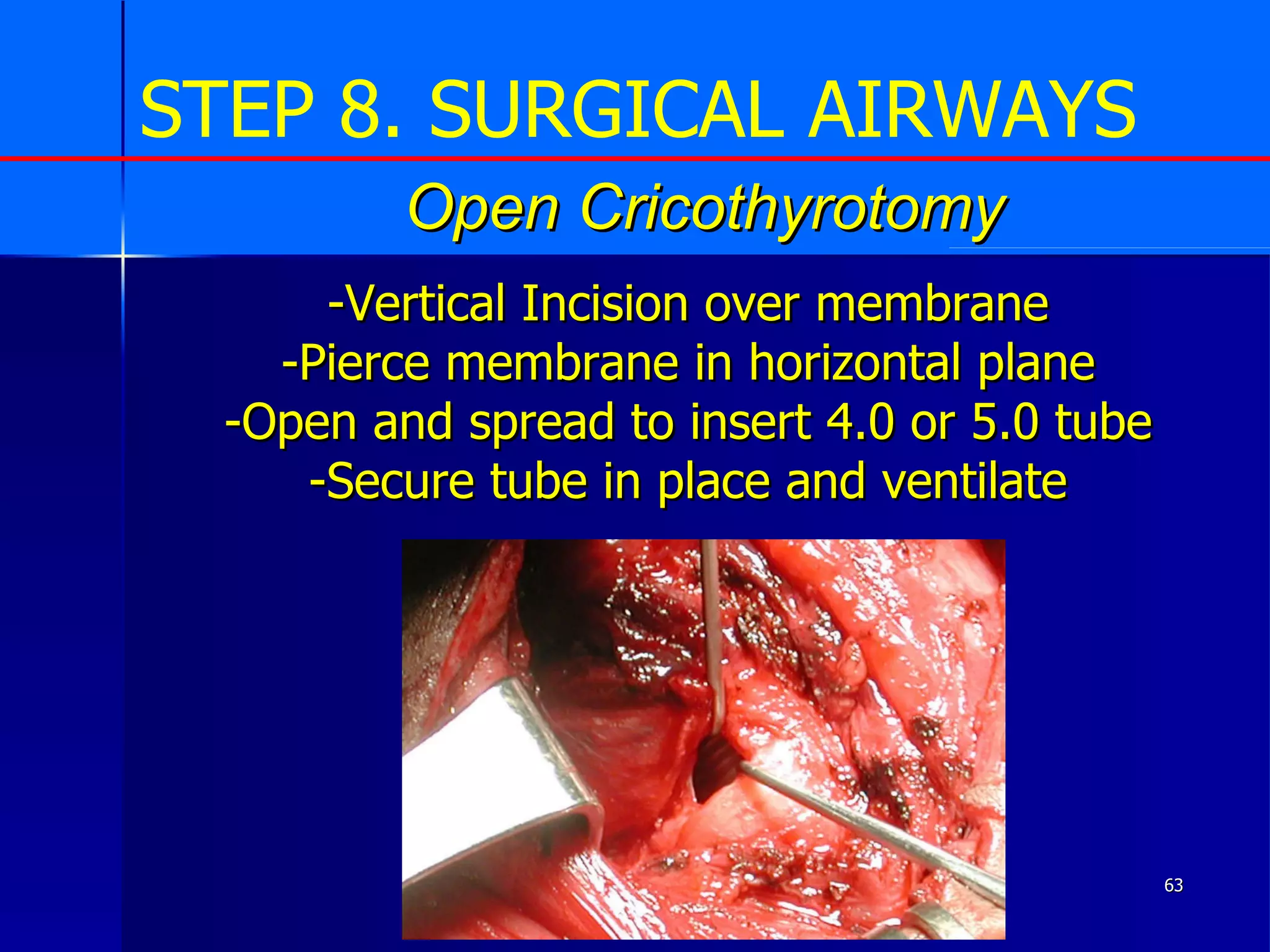
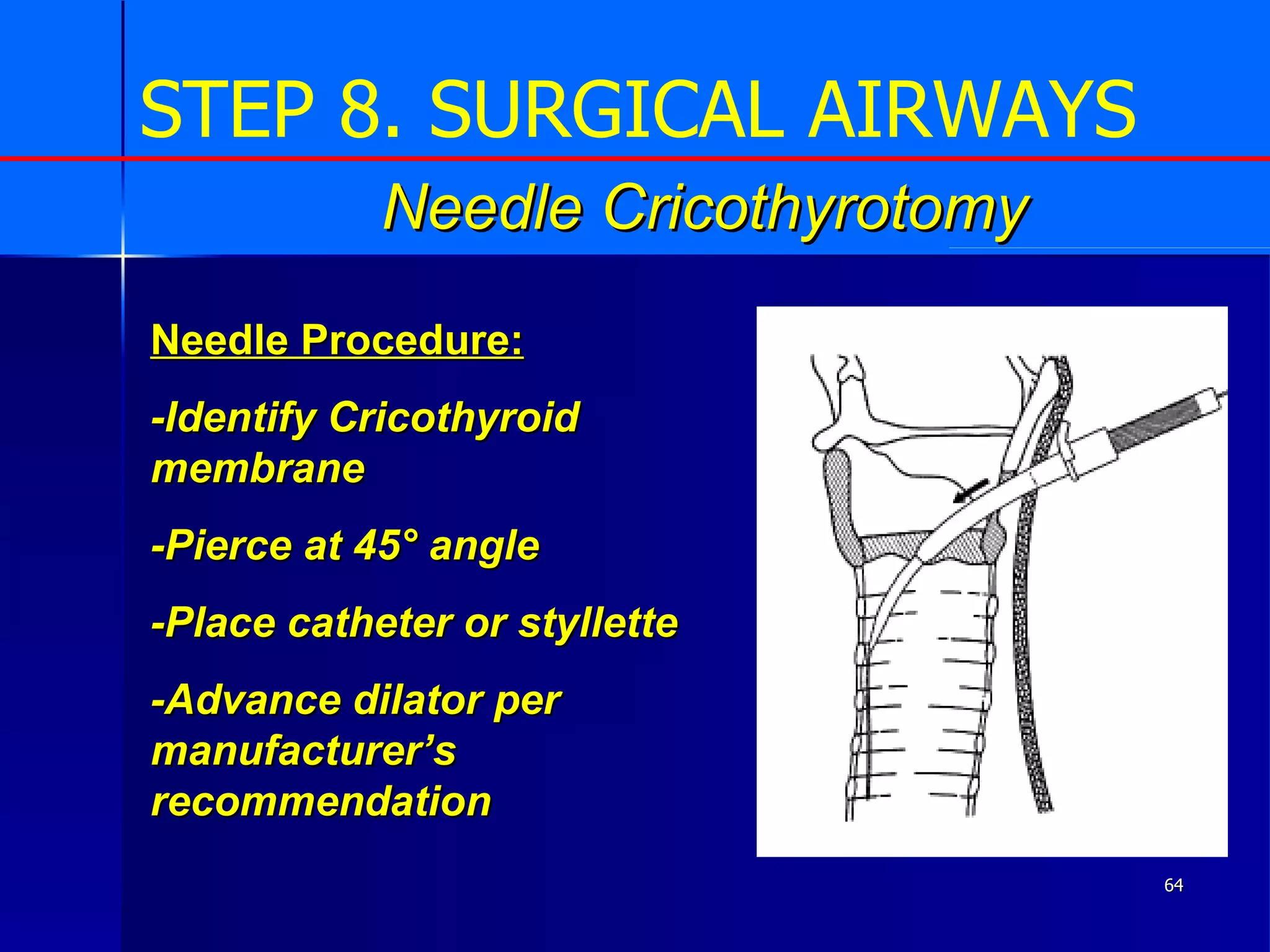
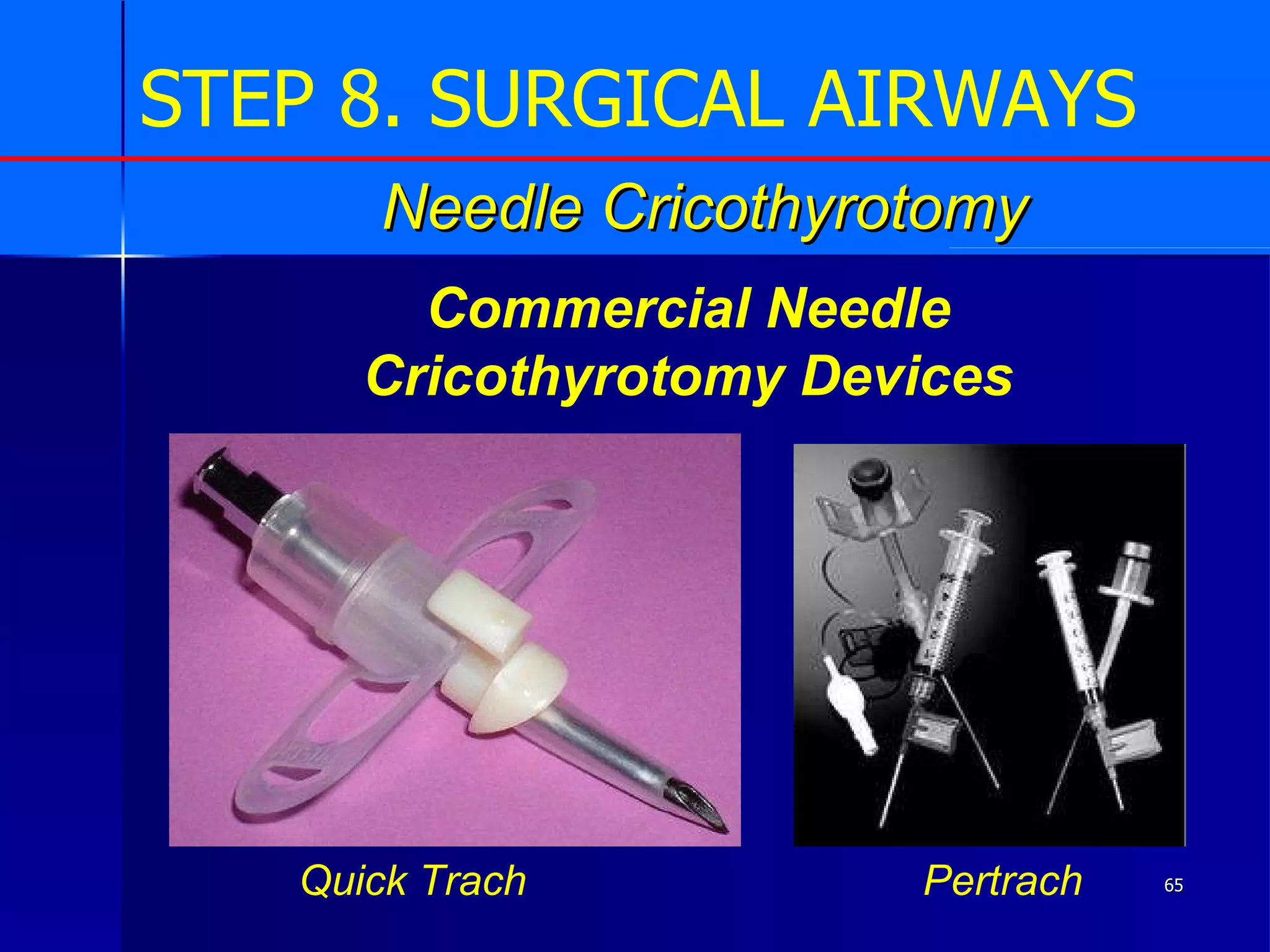
The document outlines Maine's new airway management algorithm which was developed in response to quality assurance concerns. The algorithm provides a step-by-step process for evaluating and managing a patient's airway from basic to advanced life support. It also reviews various airway devices and procedures, outlines mandatory equipment requirements, and provides training objectives for providers.