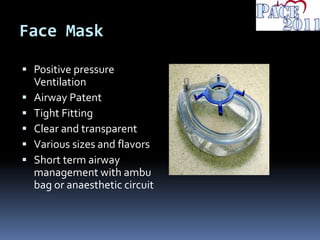
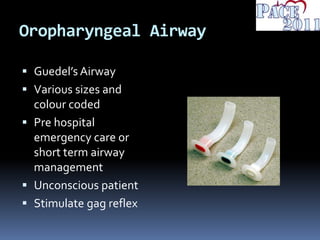
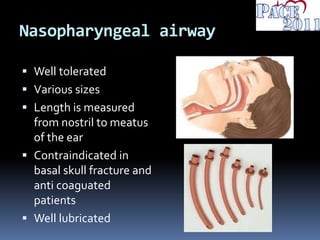
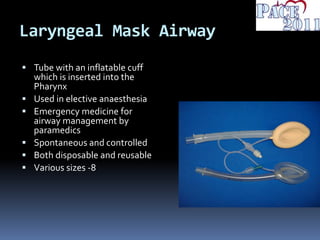
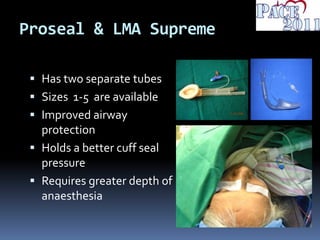
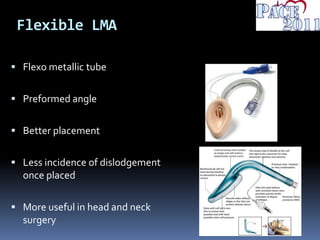
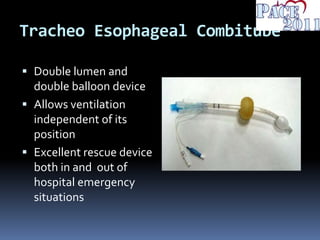
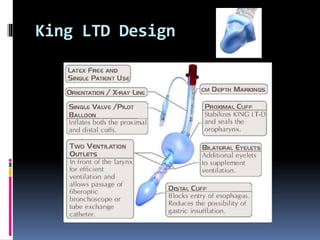
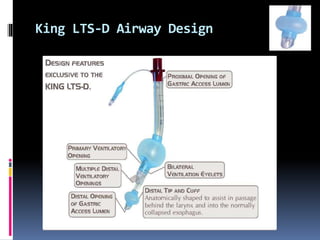
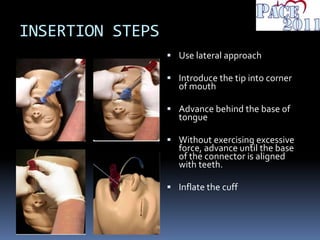
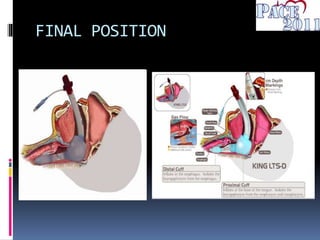
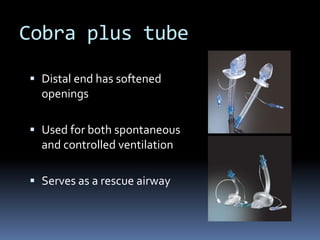
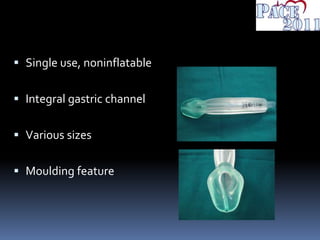
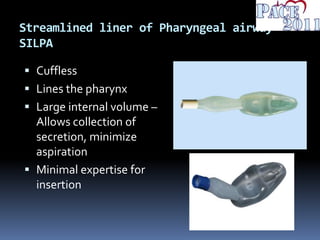
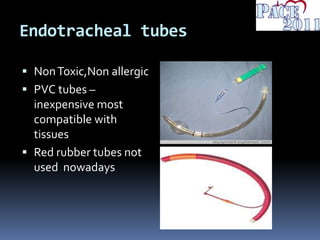
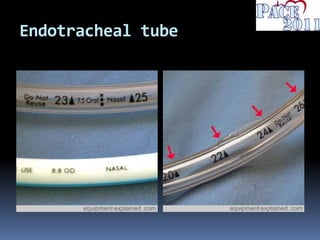
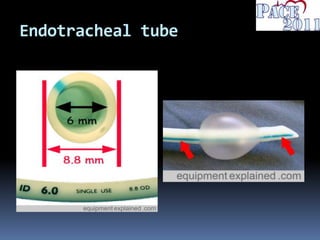
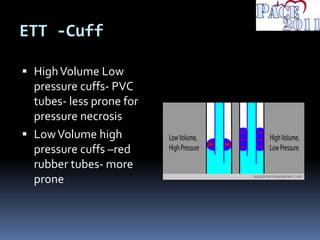
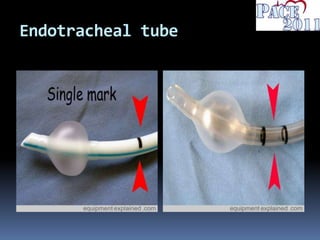
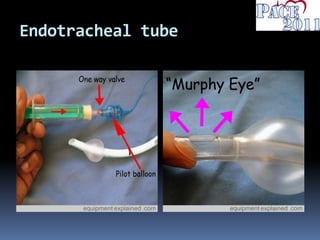
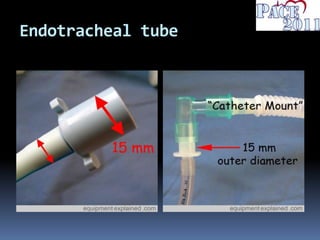
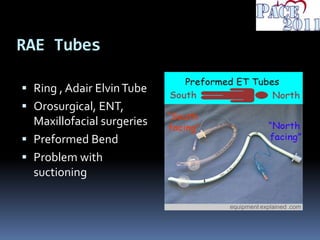
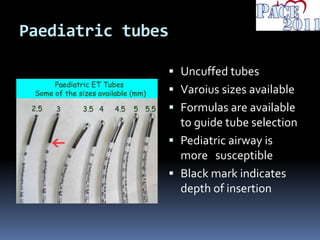
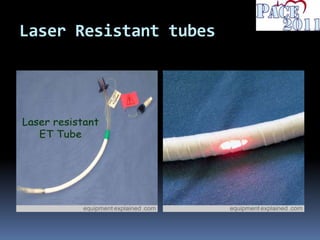
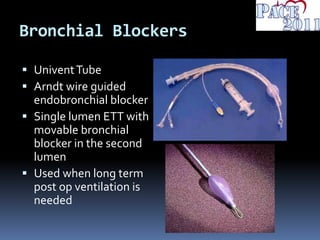
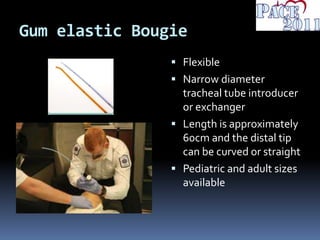
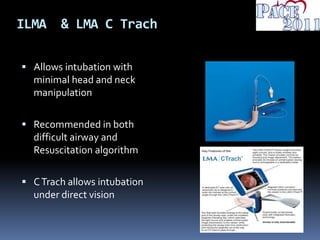
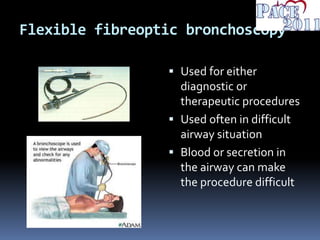
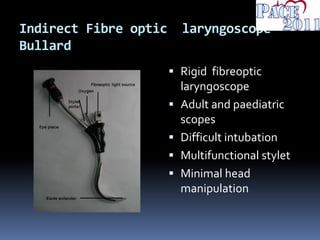
This document discusses various airway devices and their specifications. It describes simple airway devices like face masks, oropharyngeal airways and nasopharyngeal airways. It then discusses supraglottic airways like laryngeal mask airways and their evolution over time. Finally, it covers intraglottic devices like endotracheal tubes and various aids for intubation. Overall, the document provides an overview of the classification and features of many common airway devices used in anesthesia and emergency medicine.