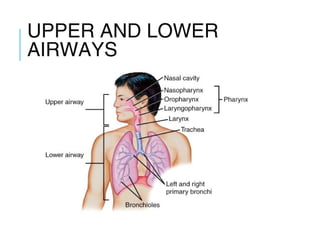
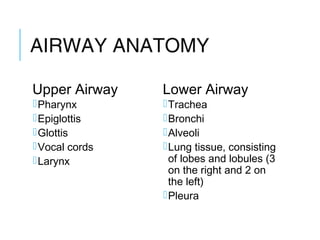
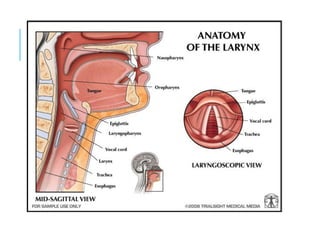
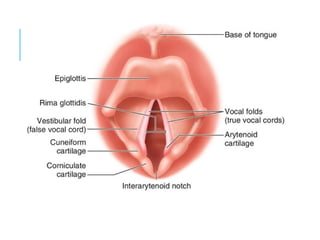
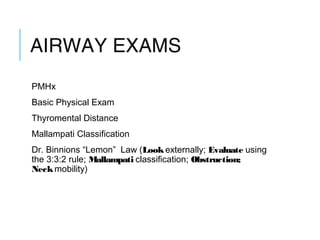
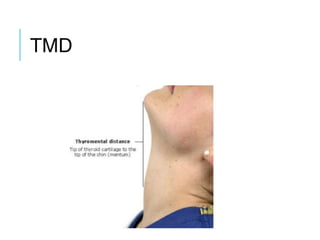
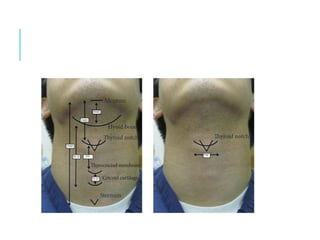
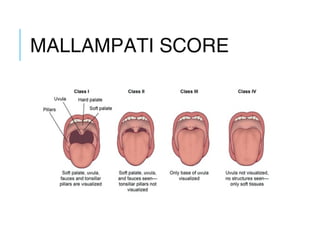
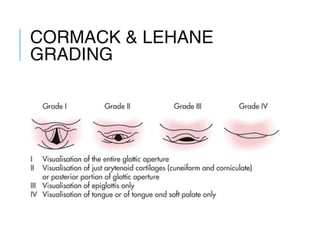
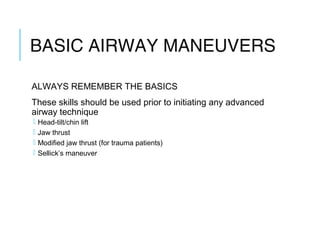
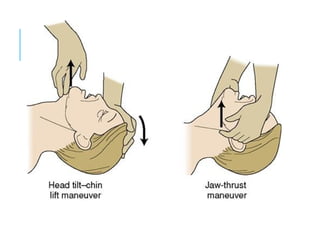
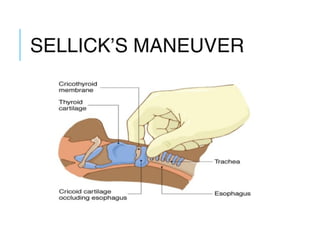
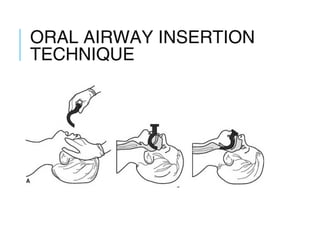
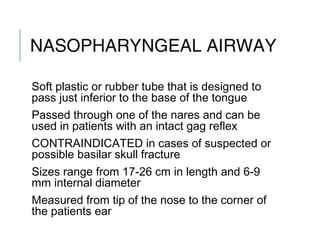
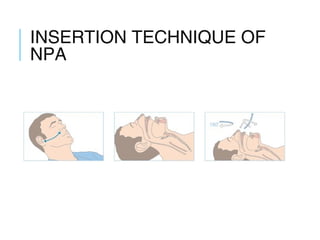
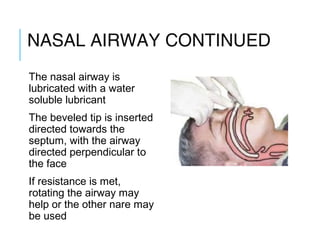
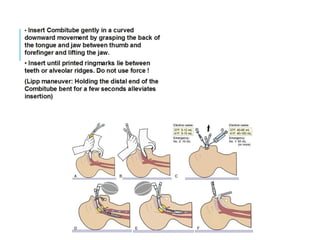
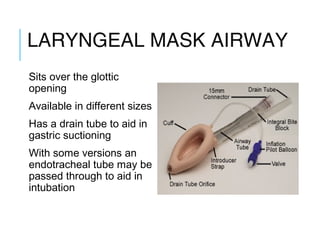
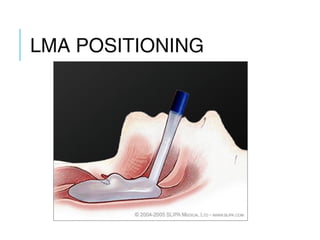
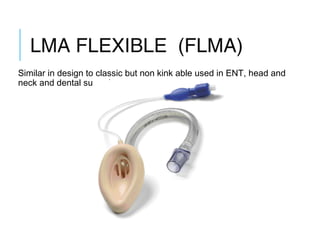
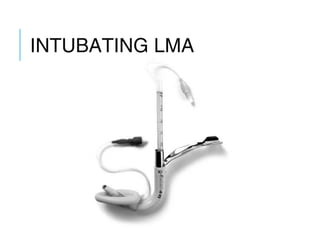
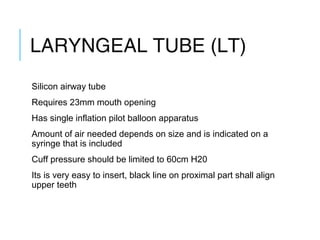
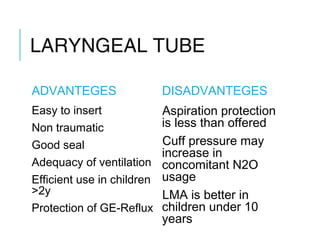
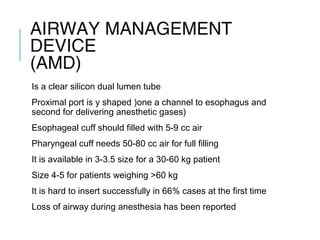
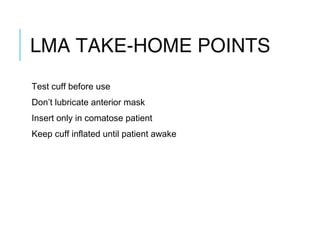
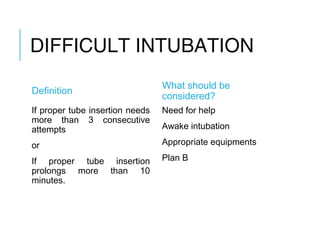
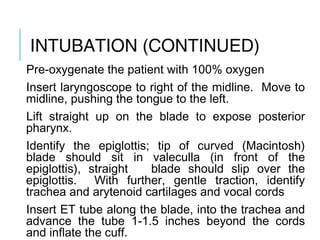
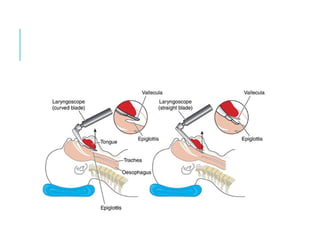
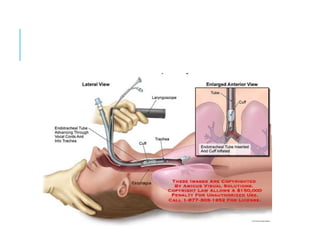
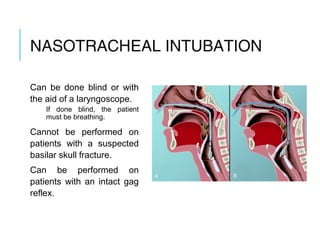
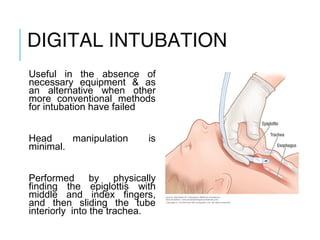
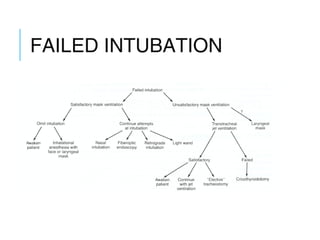
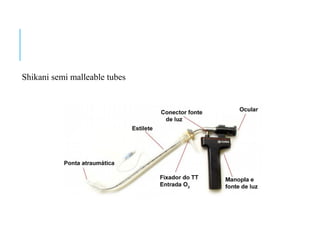
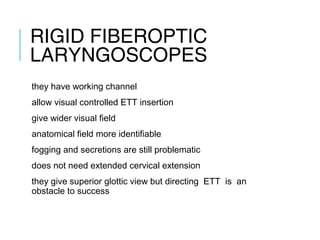
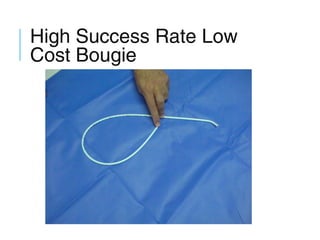
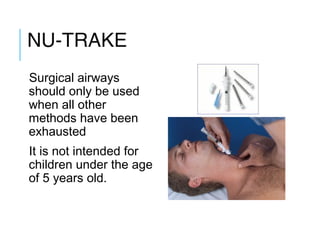
The document provides an extensive overview of airway management techniques, focusing on anatomy, examination, and various airway maneuvers. It covers basic and advanced techniques for airway management in critical and elective situations, detailing tools like oral and nasopharyngeal airways, laryngeal masks, and intubation methods. Additionally, it emphasizes the importance of core airway management skills and considers potential complications and specific guidelines for various patient scenarios.