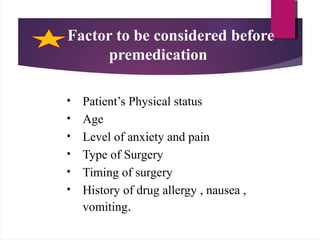
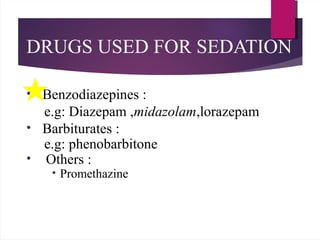
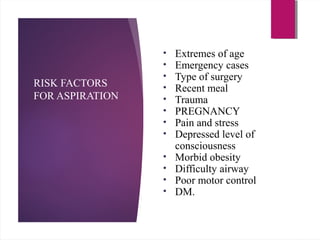
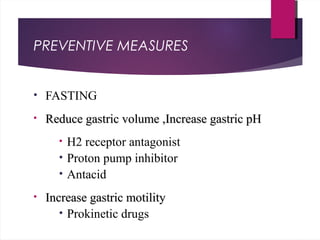
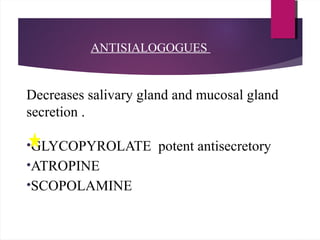
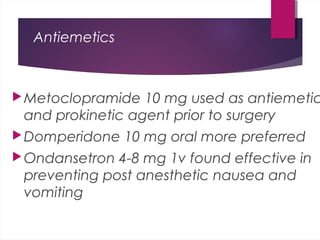
This document discusses premedication before anesthesia. It defines premedication as the administration of drugs before anesthesia induction. The goals of premedication are to provide anxiolysis, analgesia, amnesia and facilitate induction and recovery from anesthesia. Common drugs used for premedication include benzodiazepines for anxiolysis and sedation, opioids for analgesia, anticholinergics to reduce saliva production, antihistamines for their anticholinergic effects, and antiemetics to prevent nausea and vomiting. Factors like a patient's medical history, surgery type and timing must be considered when determining appropriate premedication.