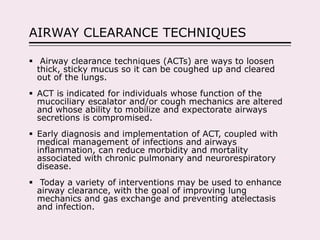
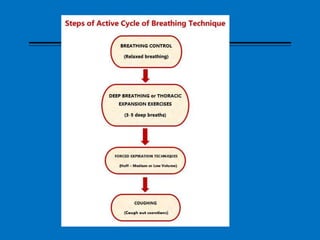
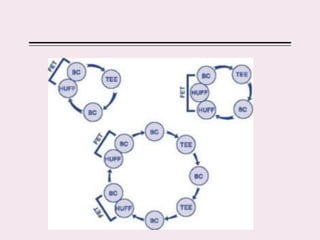
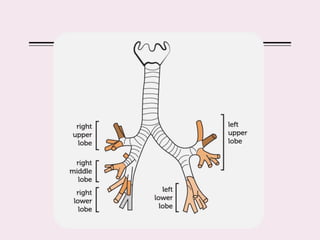
The document discusses various airway clearance techniques (ACTs) used to loosen and remove thick mucus from the lungs. It describes techniques like active cycle of breathing, thoracic expansion exercises, forced expiratory techniques, percussion, and positions. ACTs work by mobilizing secretions using breaths, coughing, and vibrations applied to the chest. Proper technique and regular implementation of ACTs can help clear airways and reduce disease symptoms and risks from conditions like cystic fibrosis or chronic lung disease. Contraindications include things like bronchospasm or inability to follow instructions.
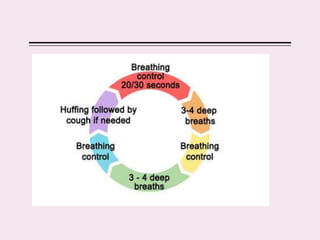
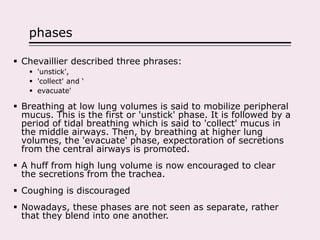
![Forced expiratory technique
A huff (also called the forced expiration technique [FET]
when combined with breathing control) is a maneuver
used to move secretions, mobilized by thoracic
expansion exercises, downstream towards the mouth.
Huffing helps moves sputum from the small airways to
the larger airways, from where they are removed by
coughing.](https://image.slidesharecdn.com/airwayclearancetechniques-200926130638/85/Airway-clearance-techniques-15-320.jpg)
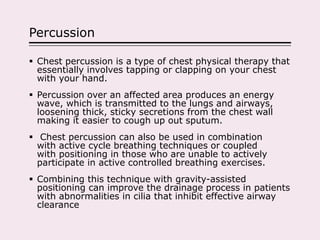
![Procedure
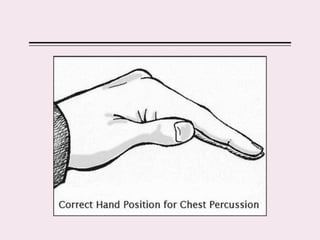
Chest percussion is performed with cupped hands which strike's
the patient chest wall in an alternating rhythmic manner over the
lung segments being drained.
This loosens the thick, sticky secretions from the walls of the lung
allowing them to move more freely into the larger airways,
especially when used with associated gravity positioning.
To improve the efficacy of treatment the following guidelines are
recommended[5]:
Patient should be in a comfortable or painless position.
The technique is applied over a towel to ensure it does not feel
uncomfortable.
Therapist should try to keep shoulders, elbows and wrist loose and mobile
during the manoeuvre.
Duration: Several minutes or until the patient needs to alter the position to
cough
https://www.youtube.com/watch?v=1ZRk55sHJ1I
https://www.youtube.com/watch?v=vxFUPdFc1eM](https://image.slidesharecdn.com/airwayclearancetechniques-200926130638/85/Airway-clearance-techniques-31-320.jpg)


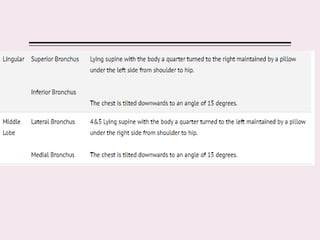
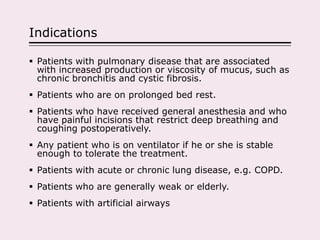
![Indications
Pre-operative screening of patients at risk of postoperative
complications to obtain a baseline of their inspiratory flow
and volume
Presence of pulmonary atelectasis
Conditions predisposing to atelectasis such as:
Abdominal or thoracic surgery[4]
Prolonged bed rest
Surgery in patients with COPD
Presence thoracic or Abdominal binders.
Lack of pain control
Restrictive lung disease associated with a
dysfunctional diaphragm or involving respiratory
musculature
Patients with inspiratory capacity less than 2.5 litres
Patients with neuromuscular disease or spinal cord injury](https://image.slidesharecdn.com/airwayclearancetechniques-200926130638/85/Airway-clearance-techniques-66-320.jpg)