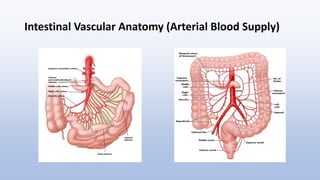
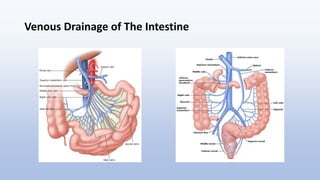
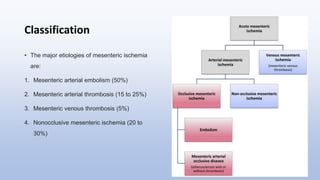
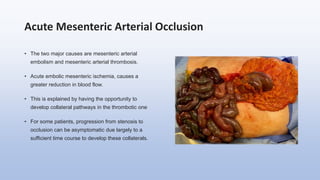
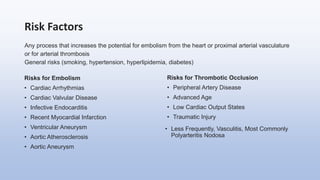
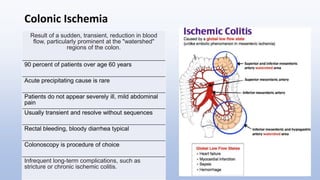
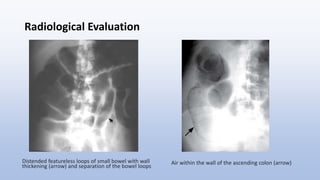
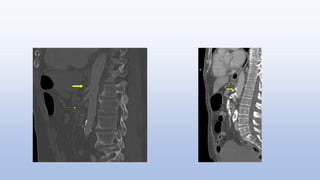
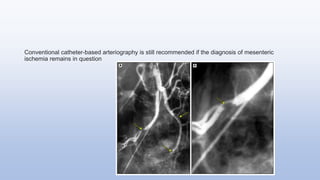
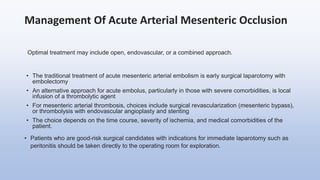
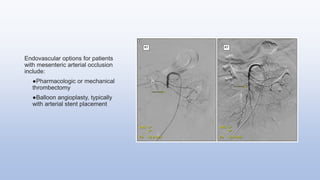
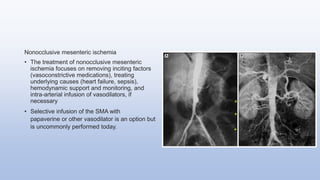
Mesenteric ischemia refers to reduced blood flow to the intestines, impacting both small and large intestines, with various causes including arterial or venous occlusion. It presents with symptoms like abdominal pain and may progress to severe complications; diagnosis relies on clinical suspicion and imaging. Management includes supportive care, surgical intervention, and long-term prevention of embolic events, as mortality rates can exceed 60% depending on the severity and timing of treatment.