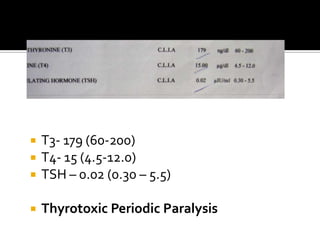
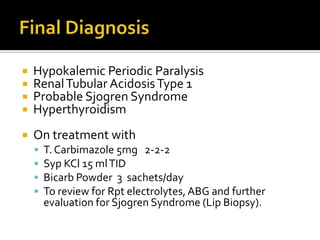
1. This patient presented with periodic paralysis caused by both hyperthyroidism (thyrotoxic periodic paralysis) and renal tubular acidosis. The hyperthyroidism prevented symptoms from manifesting until after delivery when potassium levels dropped further.
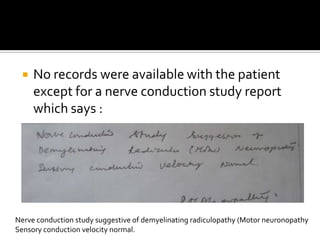
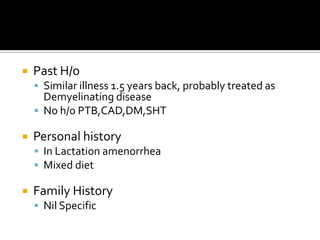
2. The initial nerve conduction study showed demyelination likely due to the previous episode being treated as a demyelinating disease.
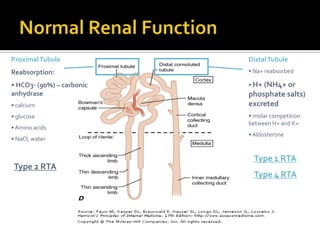
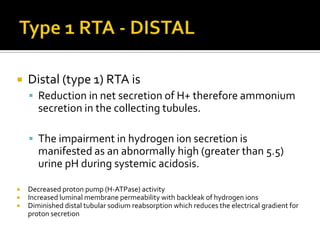
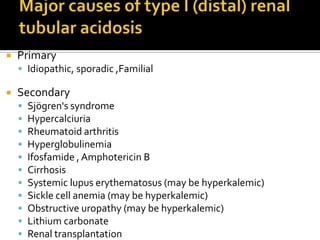
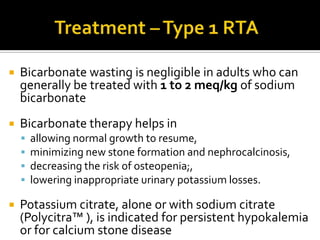
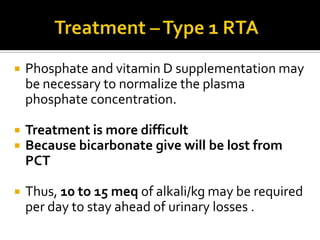
3. Going forward, the patient will need long-term management of their hyperthyroidism, renal tubular acidosis, and further evaluation for Sjogren's syndrome. Potassium and bicarbonate supplementation as well as thyroid medication will be required.
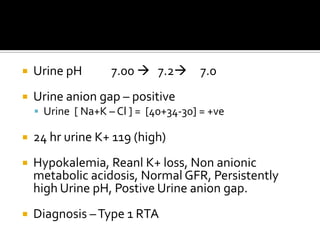
![Urine pH 7.00 7.2 7.0Urine anion gap – positive Urine [ Na+K – Cl ] = [40+34-30] = +veHypokalemia, Renal K+ loss, Non anionic metabolic acidosis, Normal GFR, Persistently high Urine pH, Positive Urine anion gap.Diagnosis – Type 1 RTA](https://image.slidesharecdn.com/m2case-110611040012-phpapp01/85/A-Case-of-Quadriparesis-23-320.jpg)
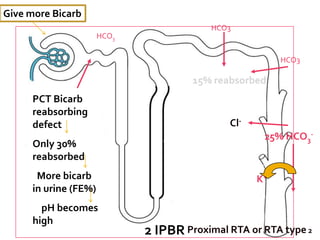
![1 IDHS[Type 1 impared distal hydrogen secretion]2 IPBR[Type 2 Impared proximal bicarbreabsorption]](https://image.slidesharecdn.com/m2case-110611040012-phpapp01/85/A-Case-of-Quadriparesis-46-320.jpg)
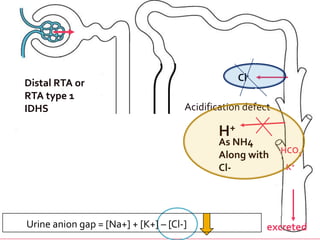
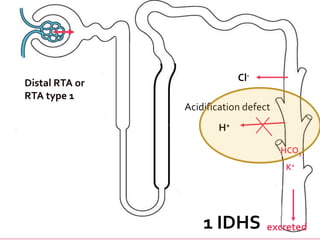
![Cl-Distal RTA or RTA type 1IDHSAcidification defectH+As NH4Along with Cl-HCO3-K+Urine anion gap = [Na+] + [K+] – [Cl-] excreted](https://image.slidesharecdn.com/m2case-110611040012-phpapp01/85/A-Case-of-Quadriparesis-63-320.jpg)