This document discusses urinary tract infections (UTIs), including:
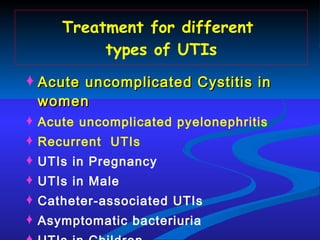
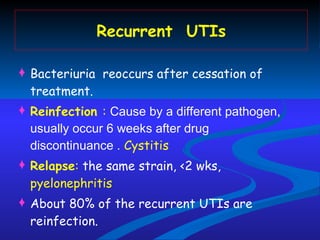
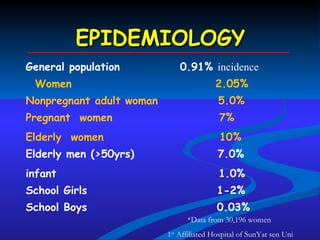
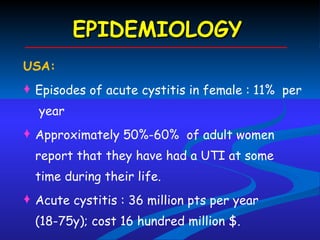
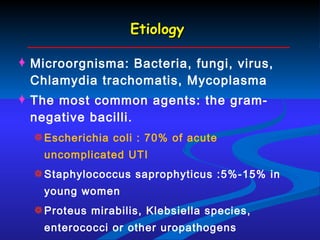
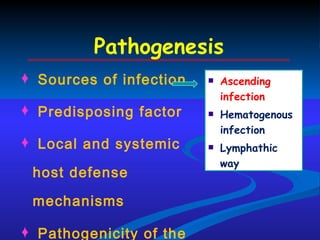
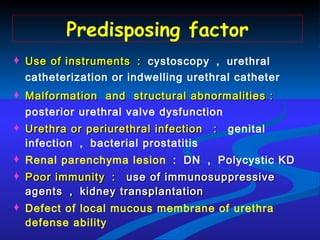
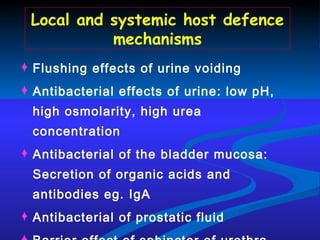
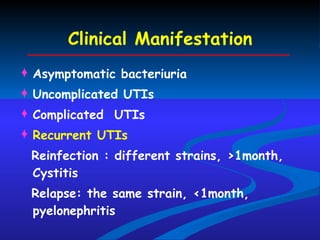
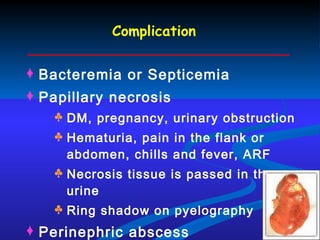
1. Definitions, epidemiology, etiology, pathogenesis, clinical manifestations, diagnosis, and treatment principles of UTIs.
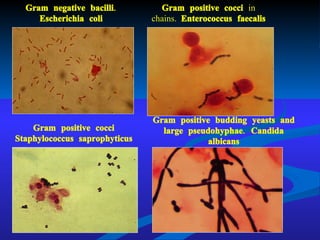
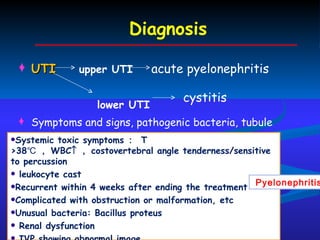
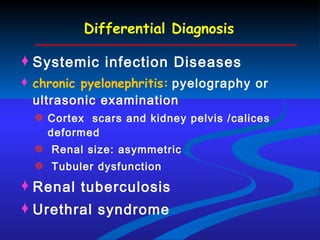
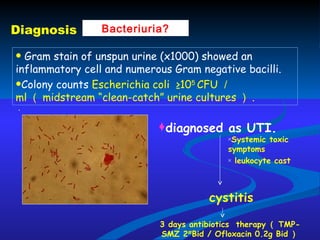
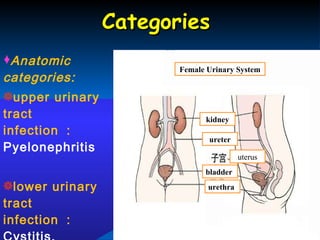
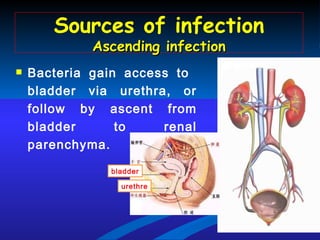
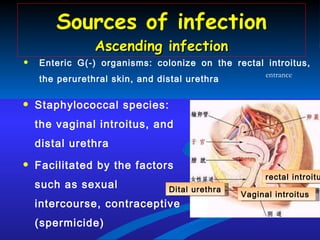
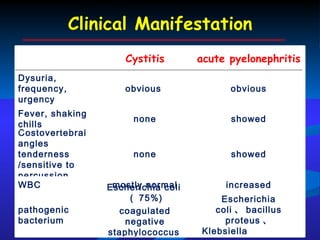
2. UTIs can be classified as upper (e.g. pyelonephritis) or lower (e.g. cystitis) depending on infection location. Escherichia coli is the most common causative agent.
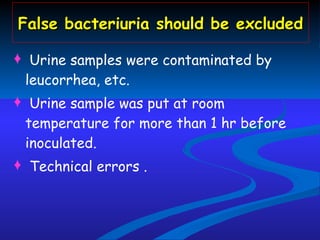
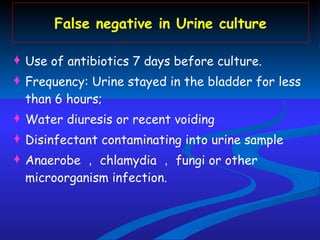
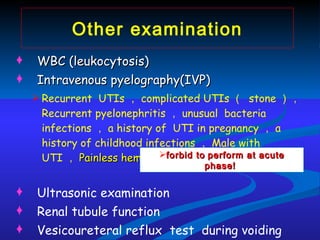
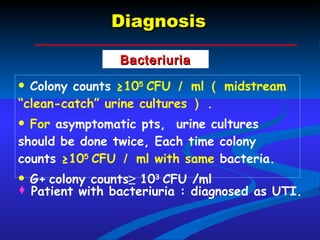
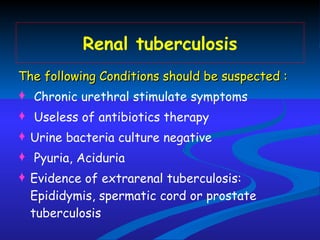
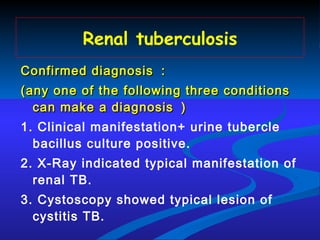
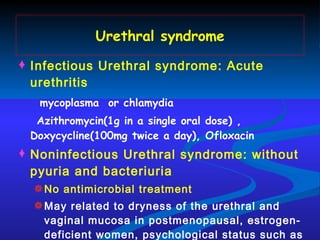
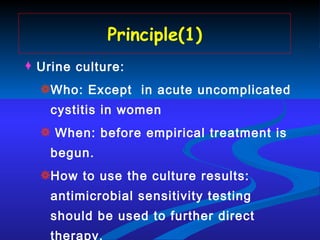
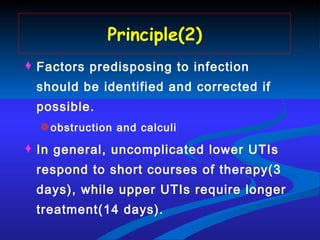
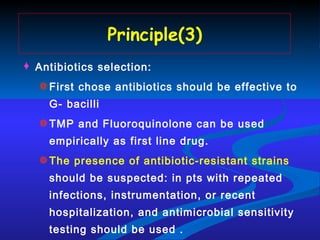
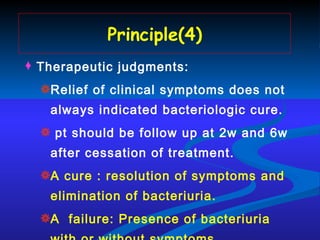
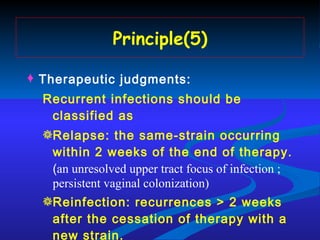
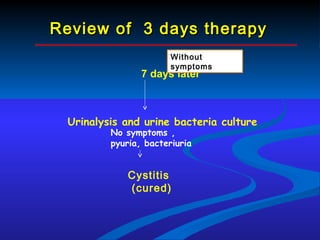
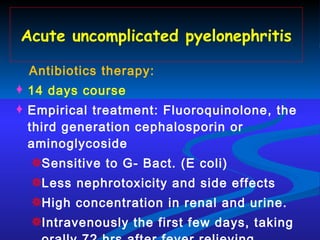
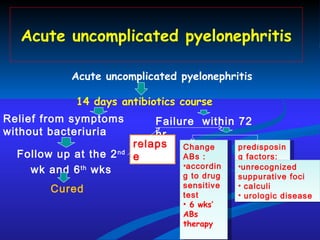
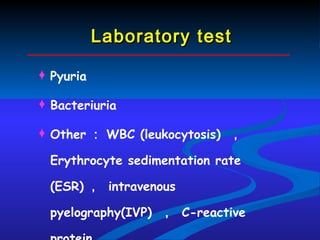
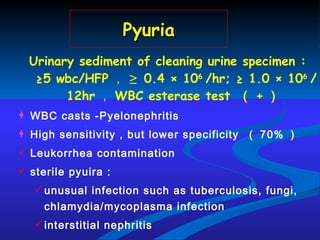
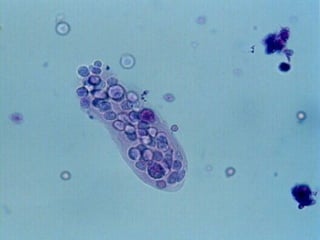
3. Diagnosis involves urine culture and microscopy to detect bacteria and white blood cells. Treatment depends on infection type and culture sensitivities.
![Urinary Tract Infection Department of Nephrology,the First Affiliated Hospital , Sun Yat-sun University Qiongqiong Yang [email_address]](https://image.slidesharecdn.com/utienglishppts-100510225624-phpapp01/75/Uti-english-ppts-1-2048.jpg)
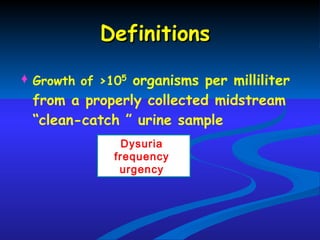

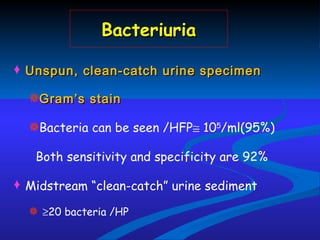
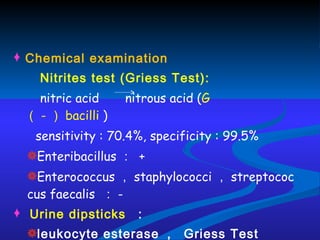
![Bacteriuria Suprapubic bladder aspirates : bacteria growth on the culture dish ( qualitative culture , Golden standard ) Voided midstream “clean-catch” urine sample Qualitative culture Colony counts ( Quantitative culture ) ≥ 10 5 CFU [colony forming unit] /ml G+ ≥10 3 CFU /ml 10 4 -10 5 CFU /ml suspicious , need reexamination 10 4 CFU /ml contaminative significant](https://image.slidesharecdn.com/utienglishppts-100510225624-phpapp01/85/Uti-english-ppts-23-320.jpg)