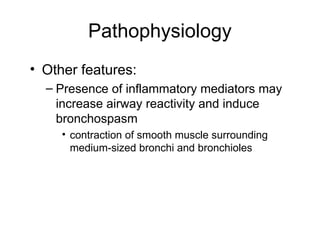
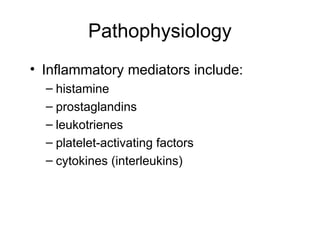
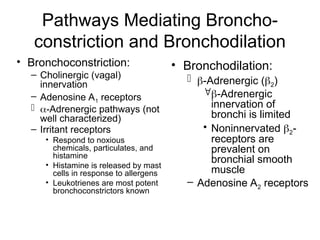
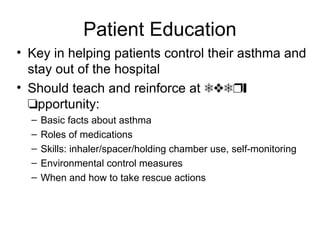
Asthma is a prevalent chronic inflammatory disease of the airways, affecting 15-20 million individuals in the US and leading to significant morbidity and mortality. It is characterized by recurrent episodes of symptoms like wheezing and breathlessness, with distinct types classified as extrinsic (allergic) and intrinsic (non-allergic). The management of asthma includes environmental control, pharmacologic therapy, regular monitoring, and patient education to prevent exacerbations and maintain normal lung function.