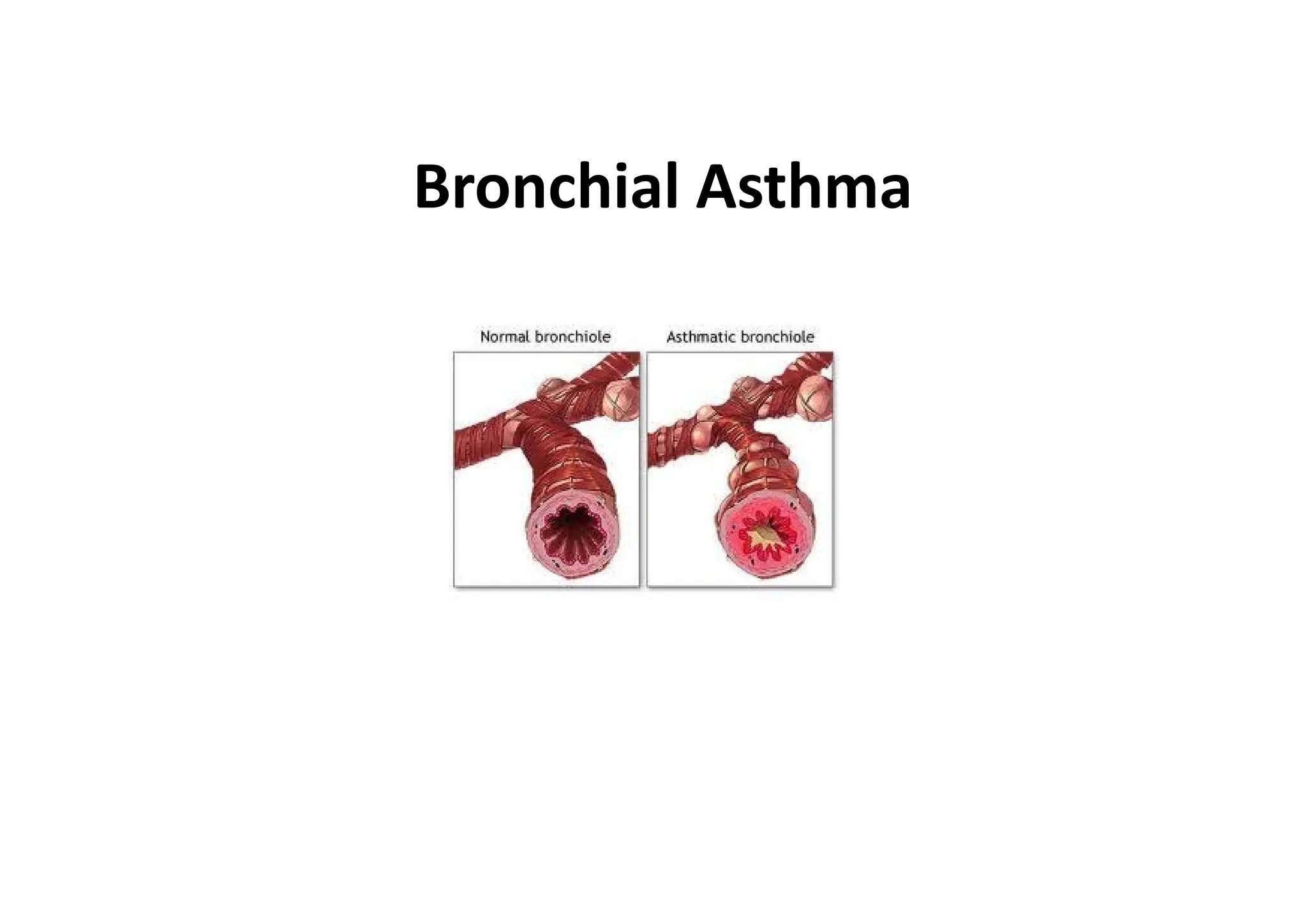
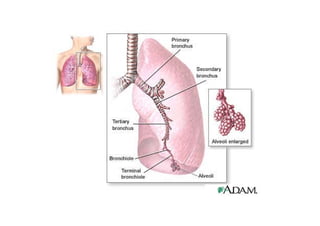
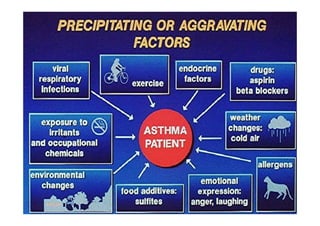
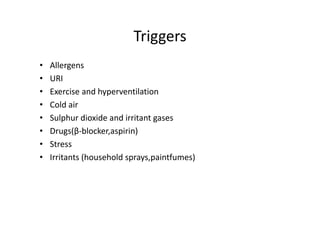
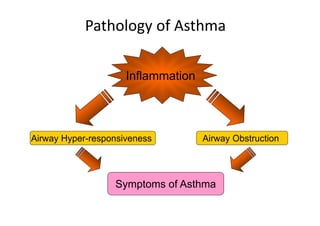
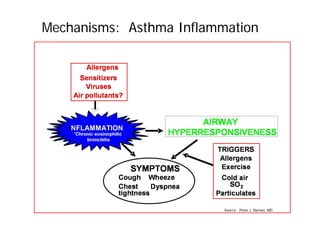
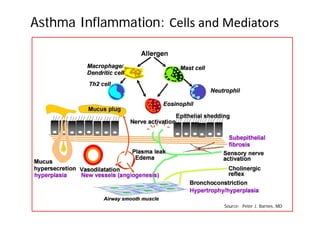
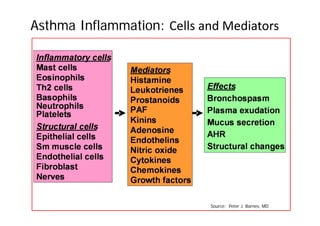
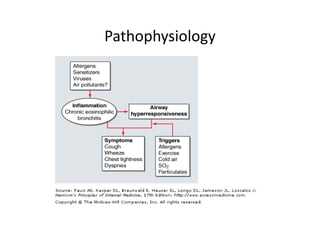
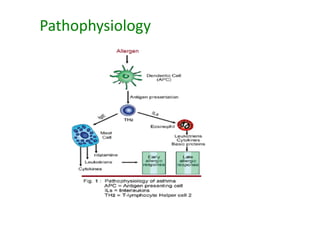
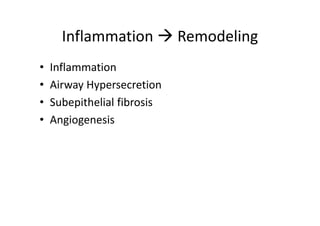
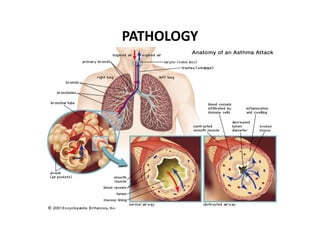
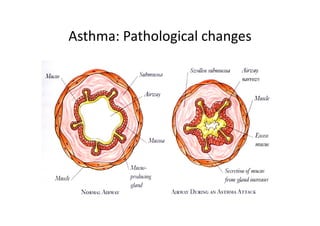
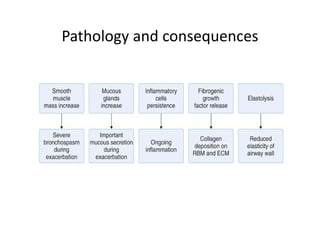
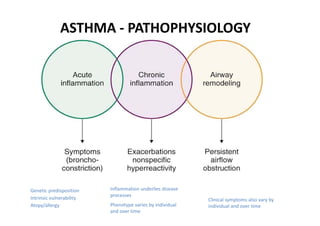
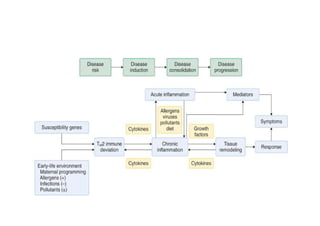
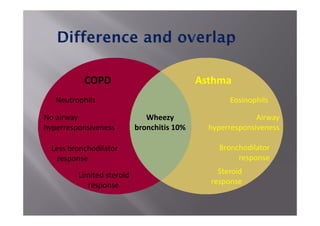
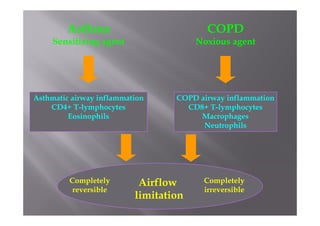
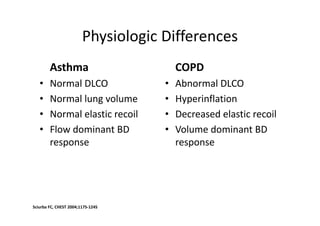
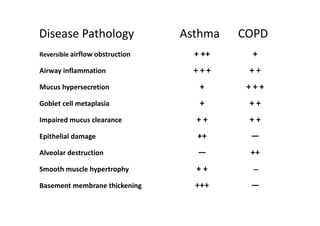
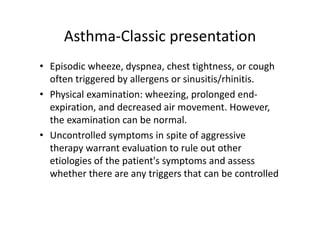
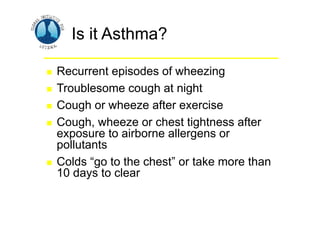
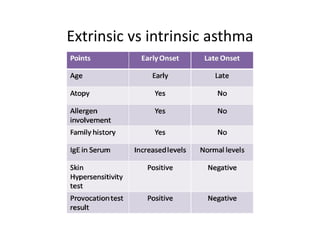
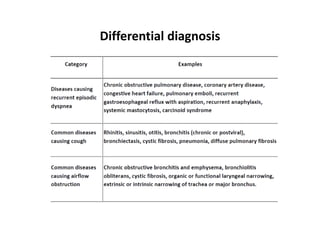
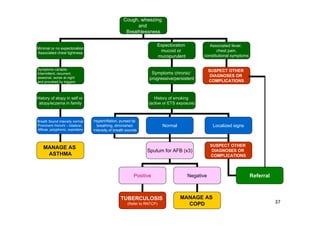
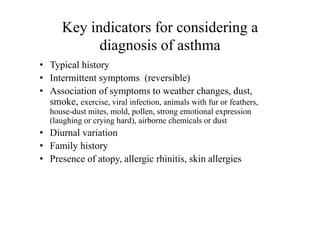
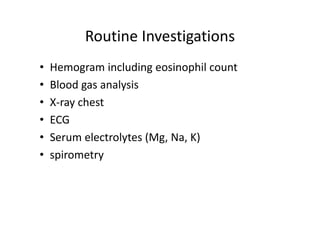
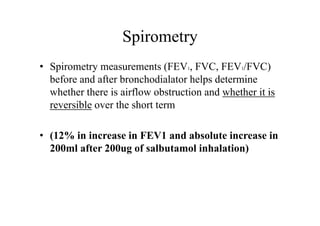
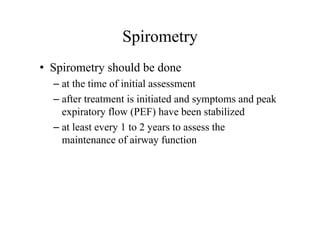
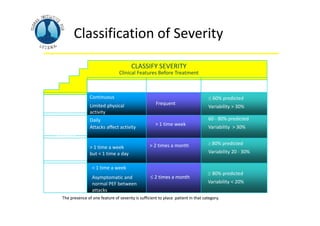
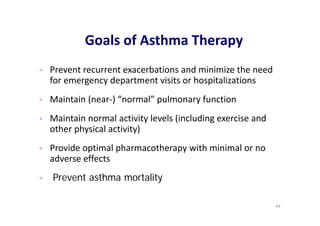
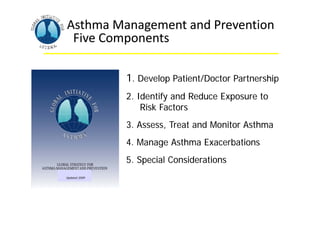
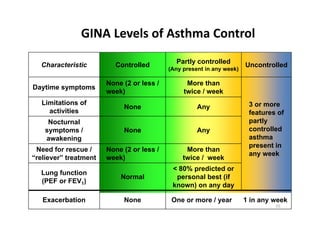
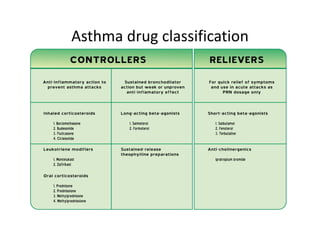
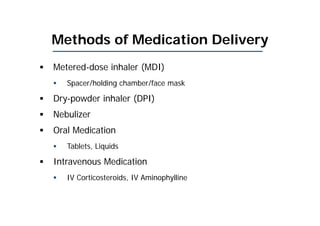
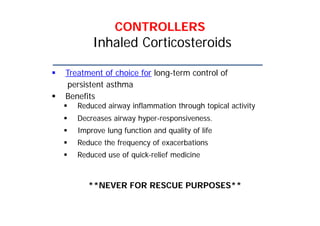
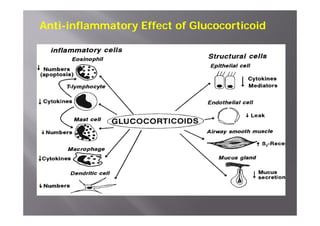
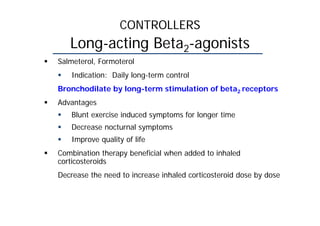
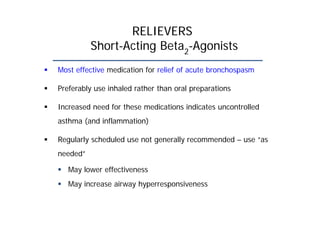
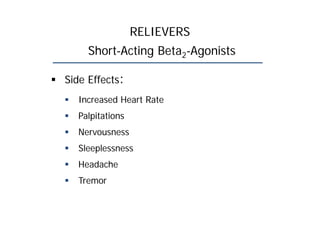
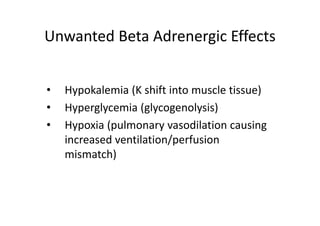
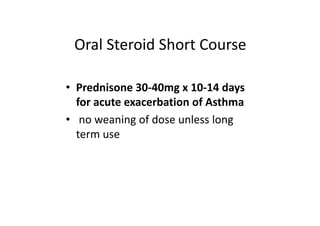
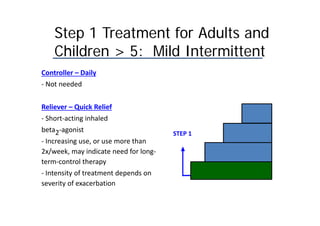
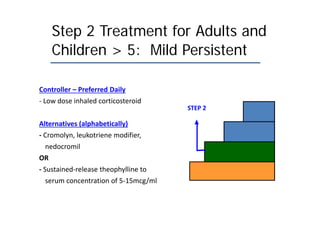
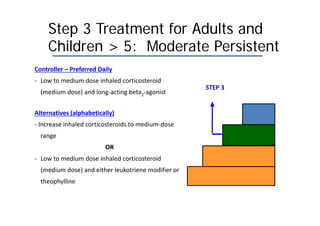
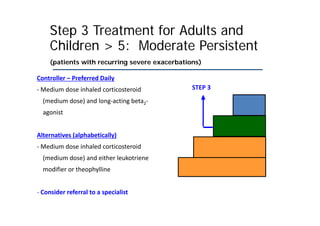
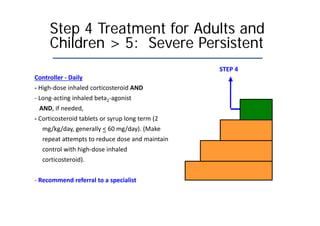
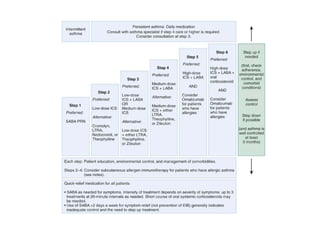
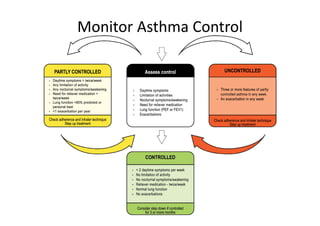
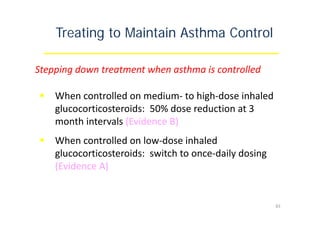
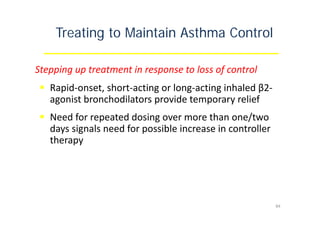
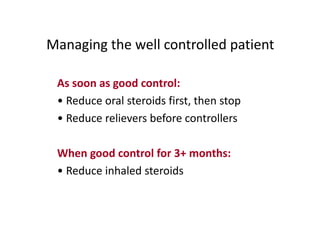
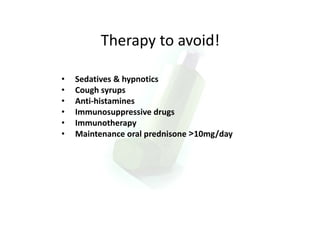
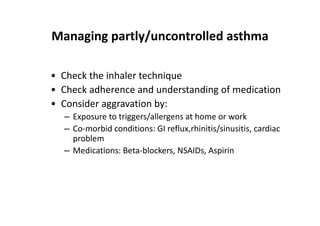
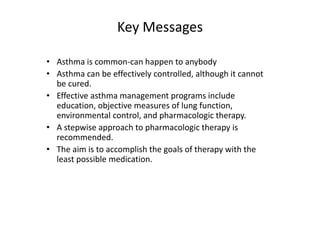
Bronchial Asthma is a chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness and coughing, especially at night or in the early morning. These episodes are usually associated with reversible airflow obstruction. Asthma is classified based on age of onset, triggers, and severity. The pathophysiology involves chronic airway inflammation and airway hyperresponsiveness leading to recurrent symptoms. Diagnosis is based on symptoms, examination findings, and confirmation of reversible airflow obstruction on spirometry. Treatment involves a stepwise approach using inhaled corticosteroids and bronchodilators to control symptoms and prevent exacerbations. The goals are to maintain normal lung function and activity levels while