This document discusses various urological malignancies including:
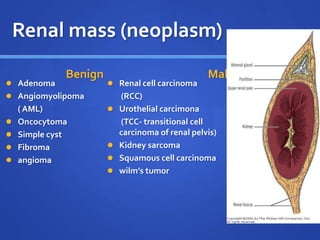
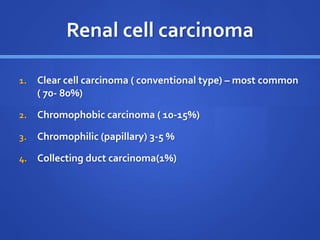
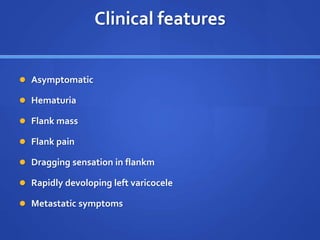
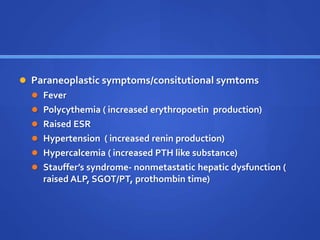
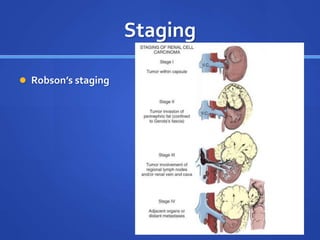
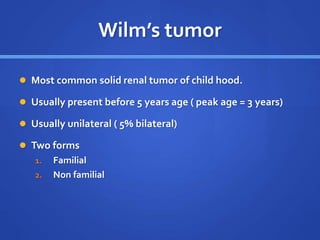
1. Renal masses like renal cell carcinoma which can be clear cell, chromophobic, or chromophilic subtypes. Symptoms include flank pain and masses. Treatment involves surgery or immunotherapy.
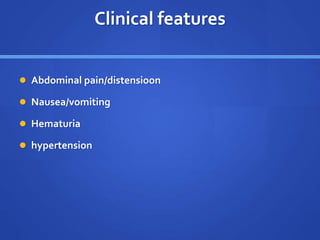
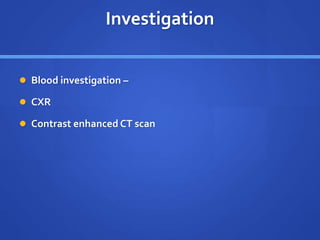
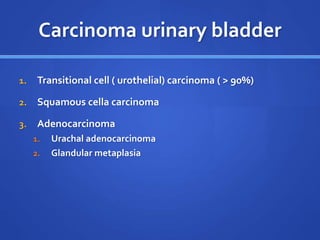
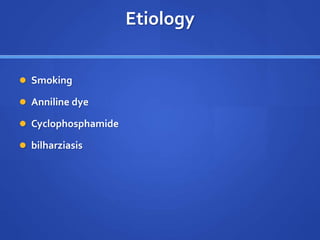
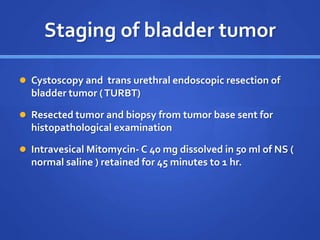
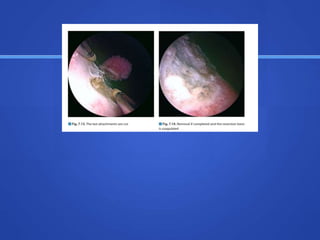
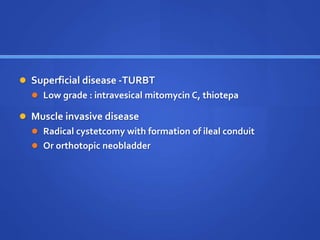
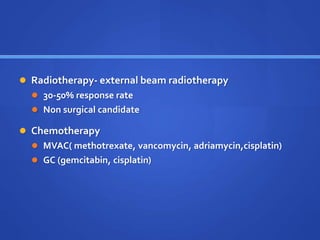
2. Bladder cancer which is usually transitional cell carcinoma caused by smoking. Symptoms include hematuria and can be staged from superficial to muscle invasive to metastatic. Treatment depends on stage.
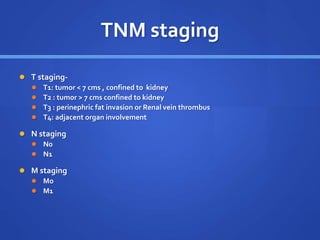
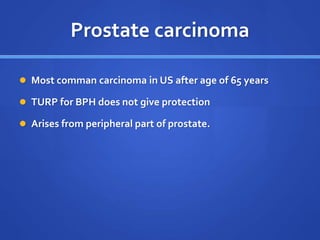
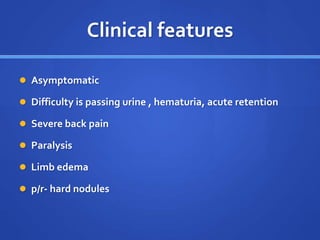
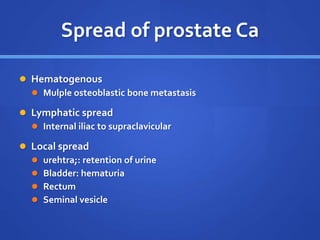
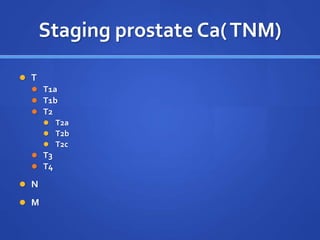
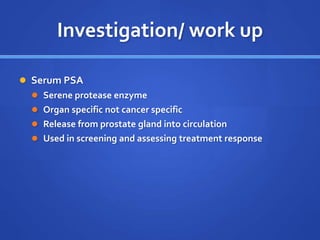
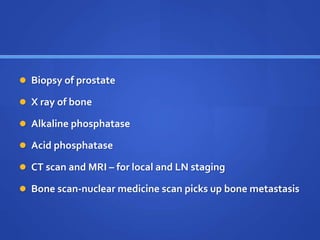
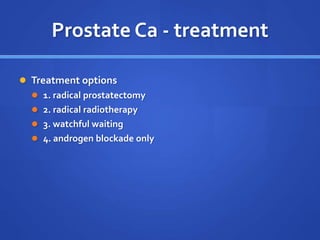
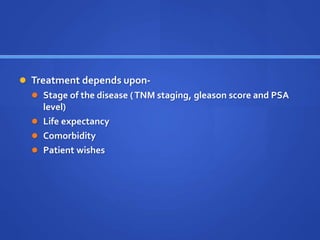
3. Prostate cancer which spreads via bone and lymph nodes and is staged using TNM. It is assessed using PSA and treated with surgery, radiation or hormone therapy depending on risk level.