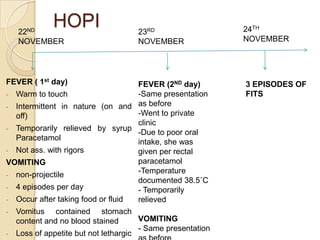
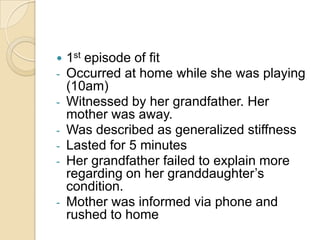
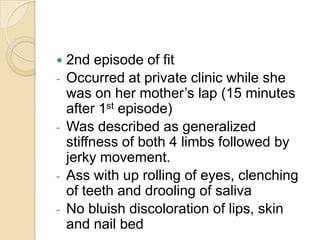
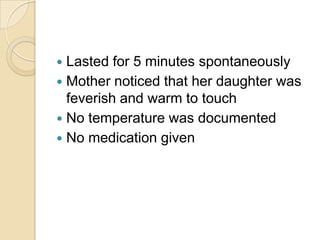
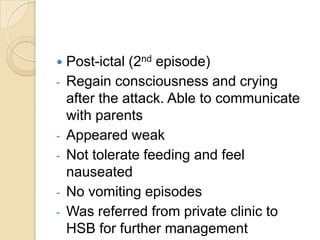
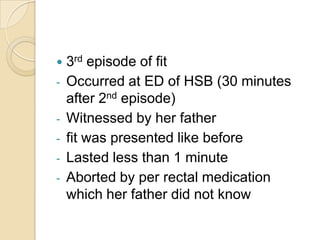
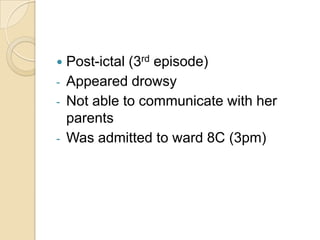
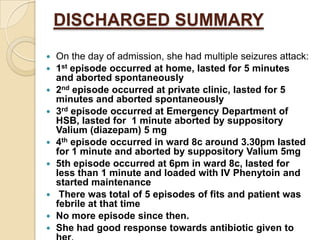
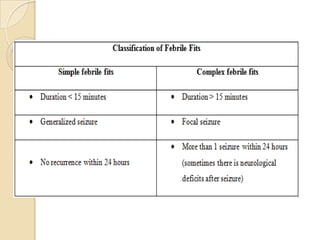
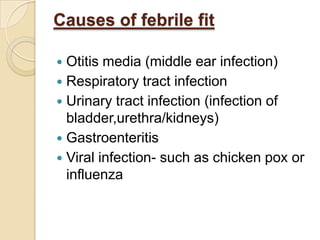
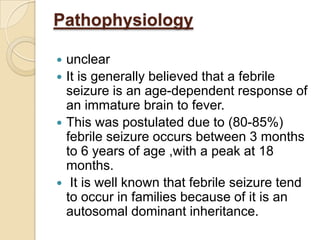
- FA, a 2-year-old Malay girl, was admitted to the hospital due to 3 episodes of seizures associated with 2 days of fever and vomiting.
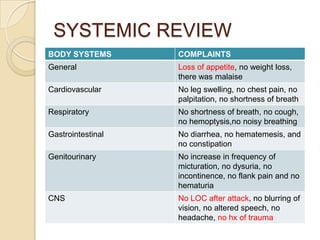
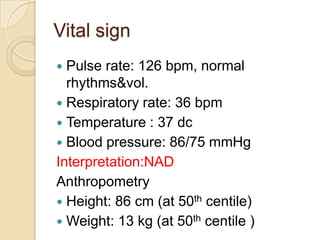
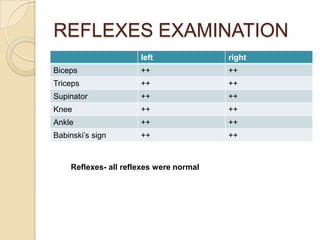
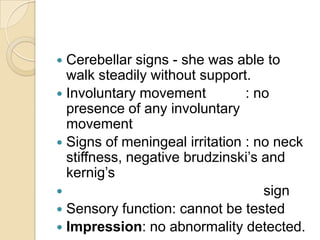
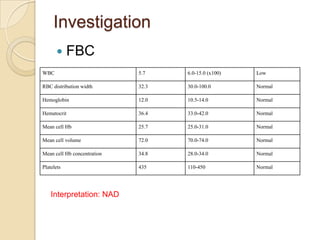
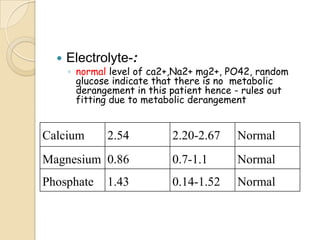
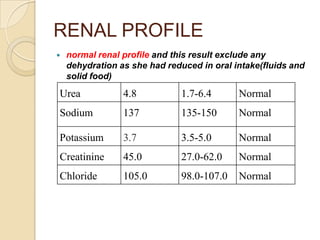
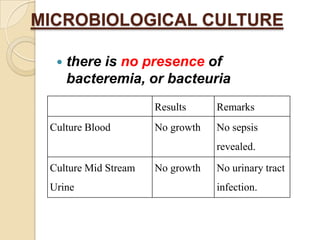
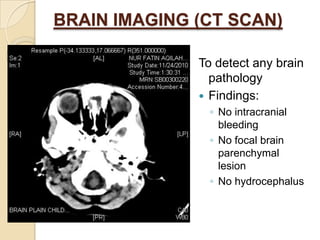
- On examination, she was conscious and alert with no abnormalities detected. Tests ruled out metabolic causes and infection.
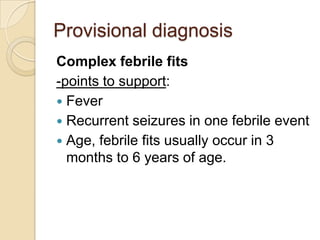
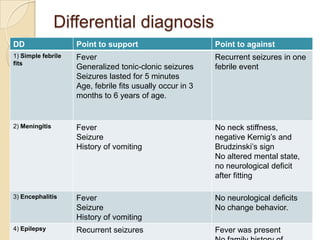
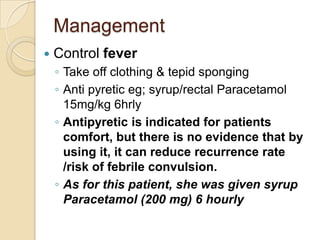
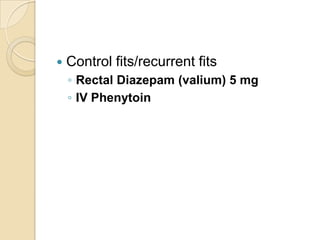
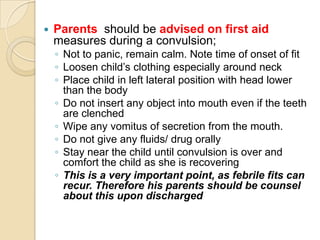
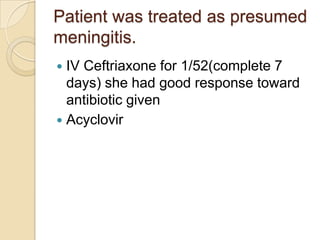
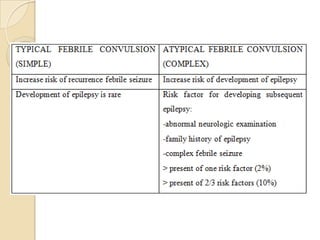
- She received antipyretics, anti-seizure medication, and antibiotics. No further seizures occurred and she improved with treatment. Her diagnosis was complex febrile seizures presumed to be caused by meningitis.