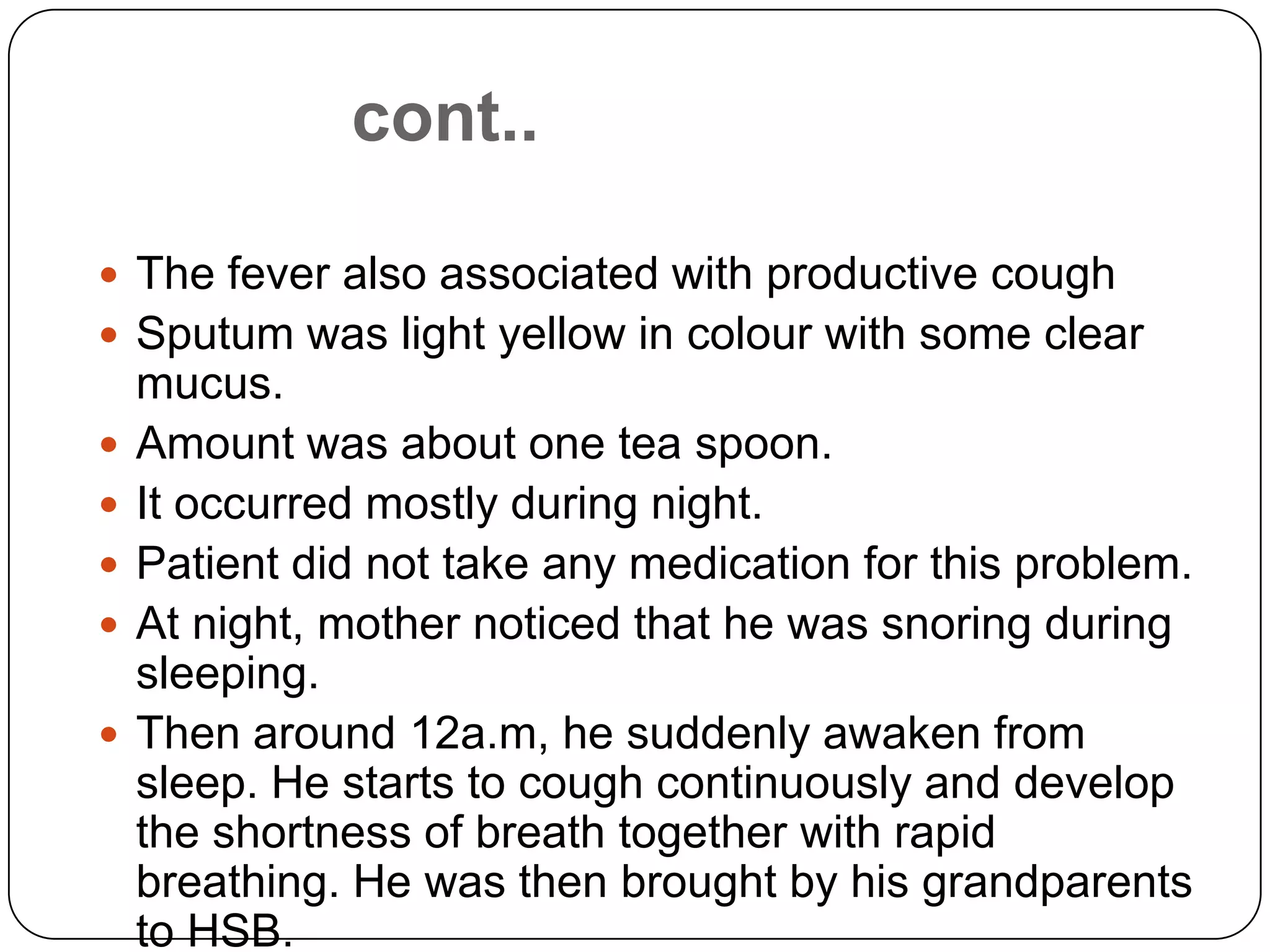
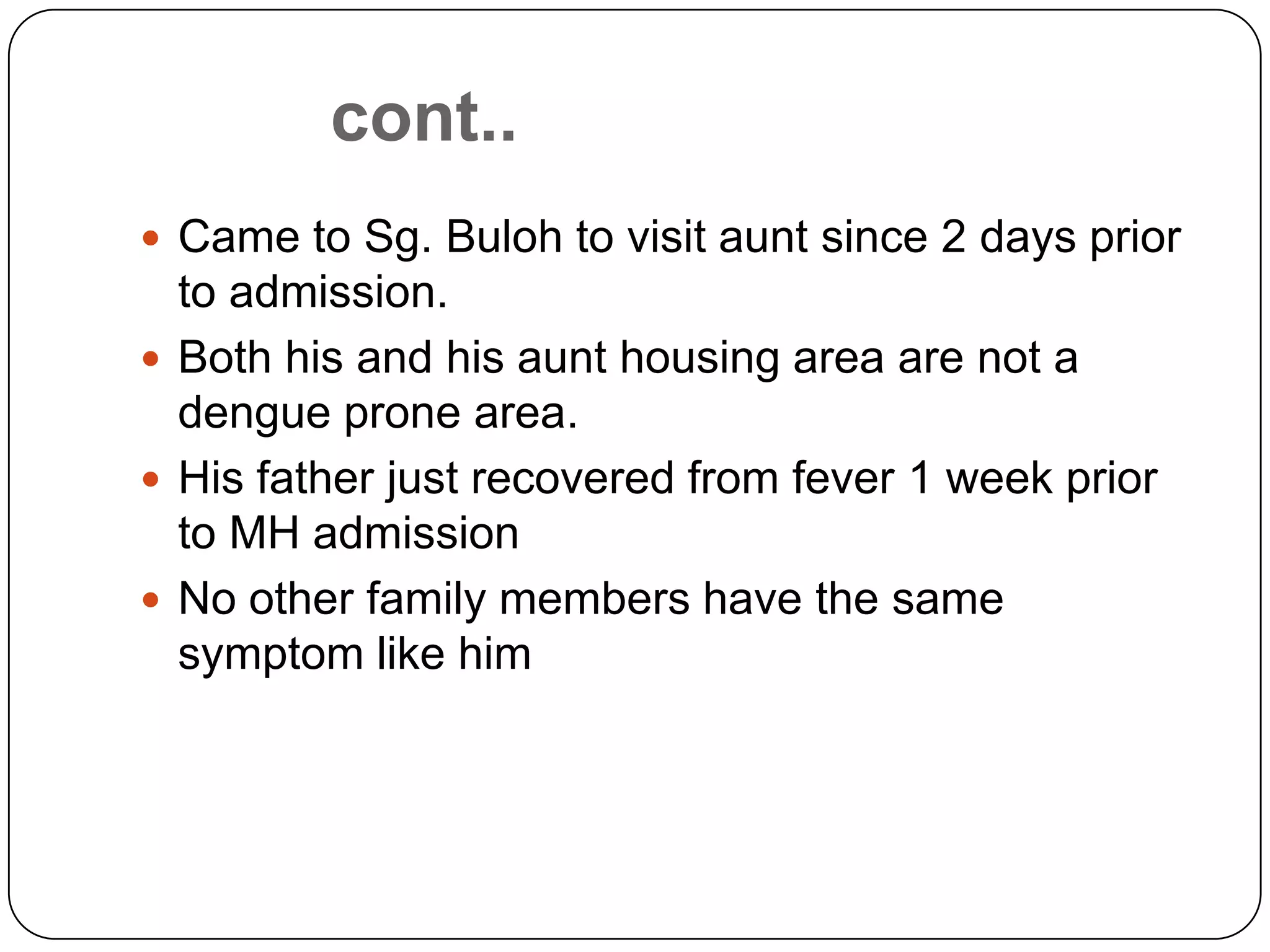
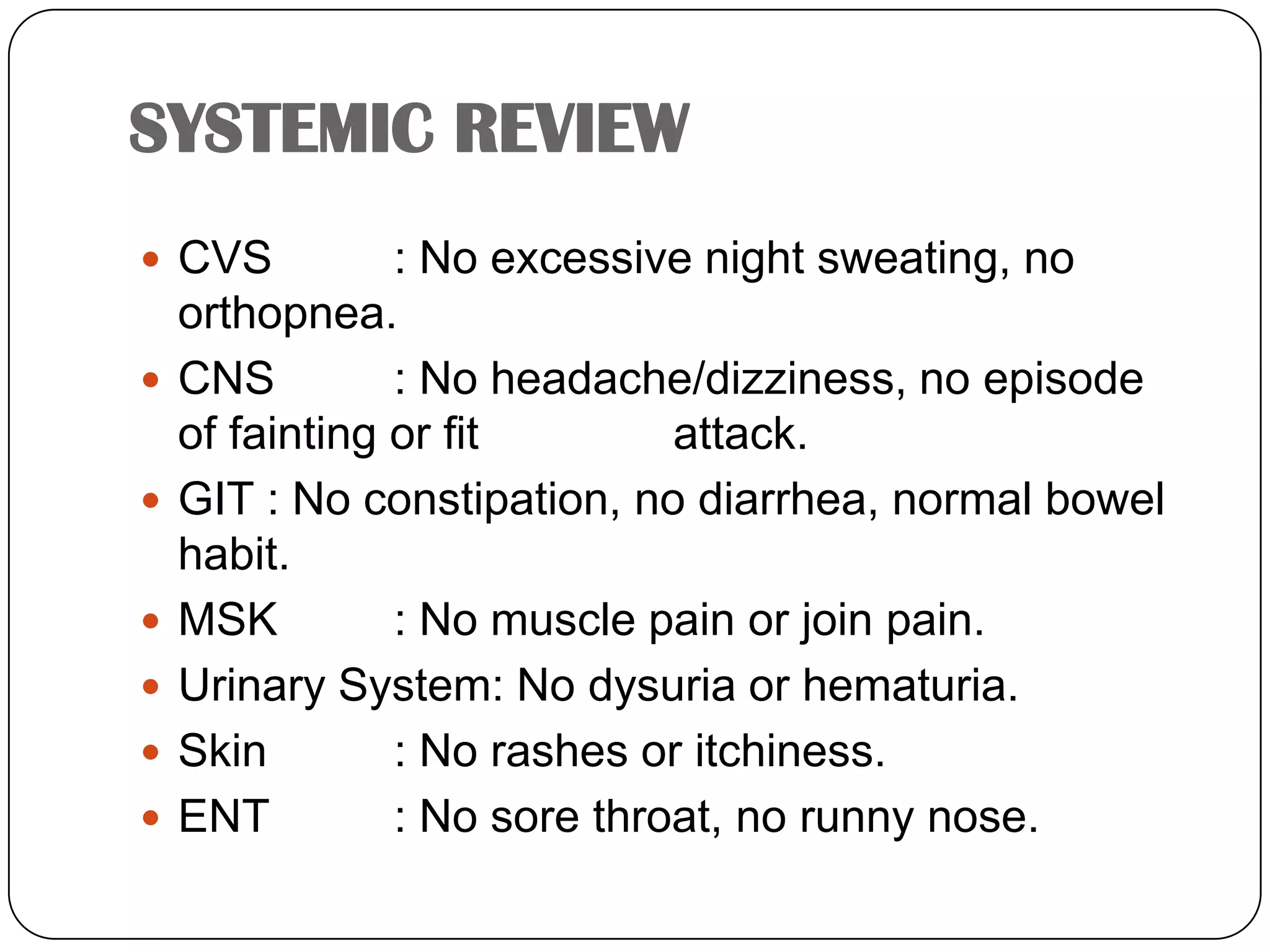
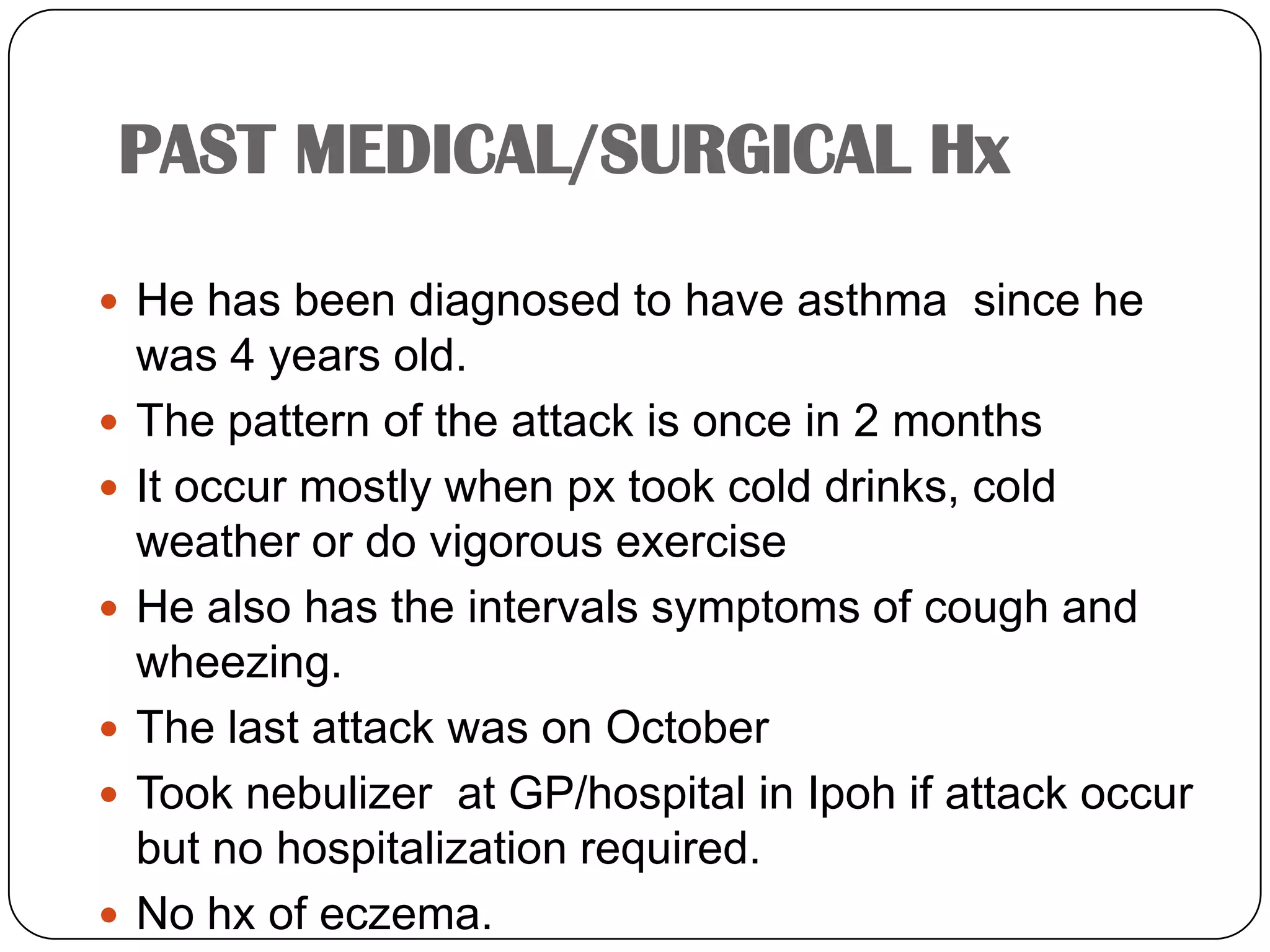
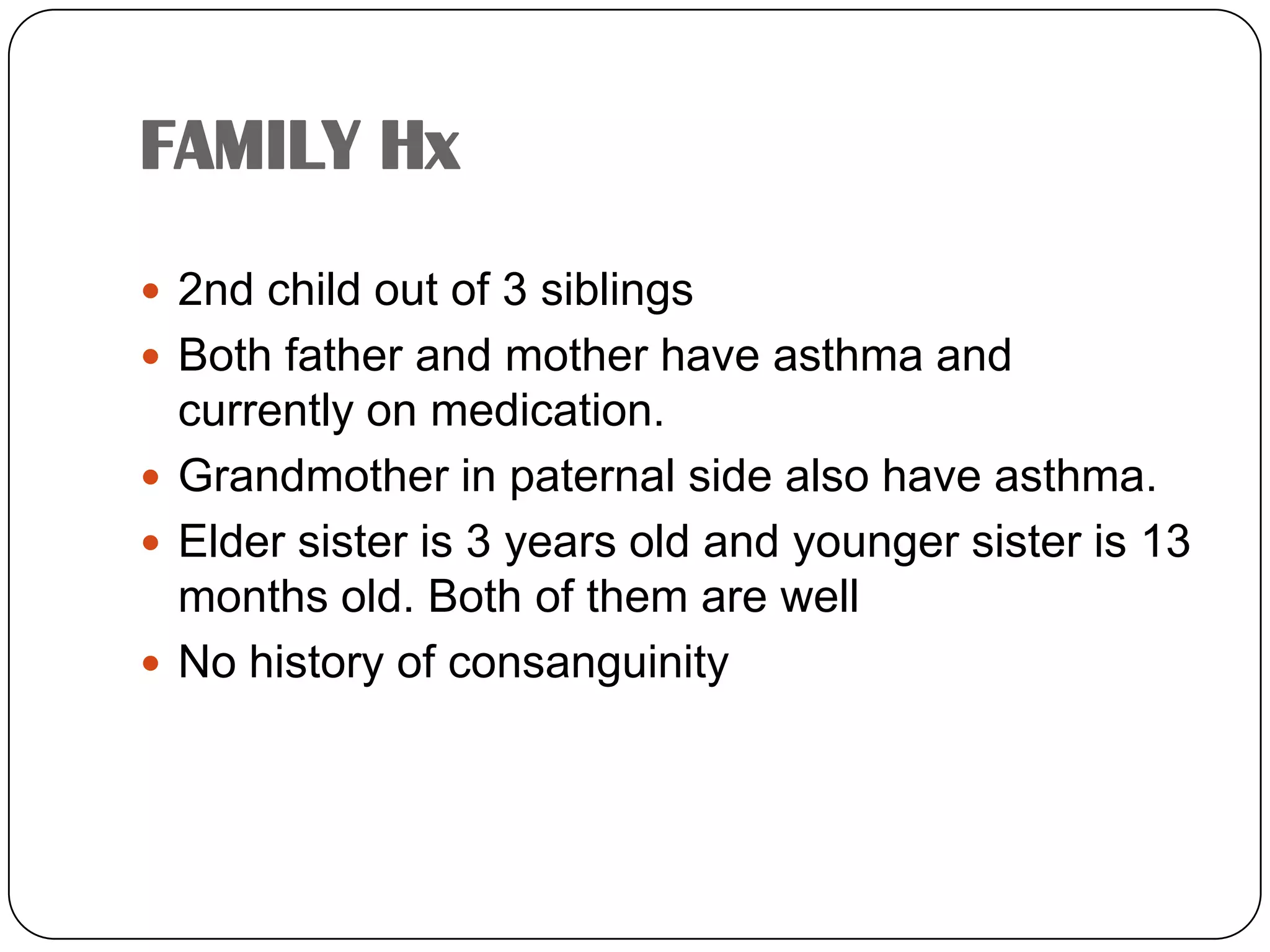
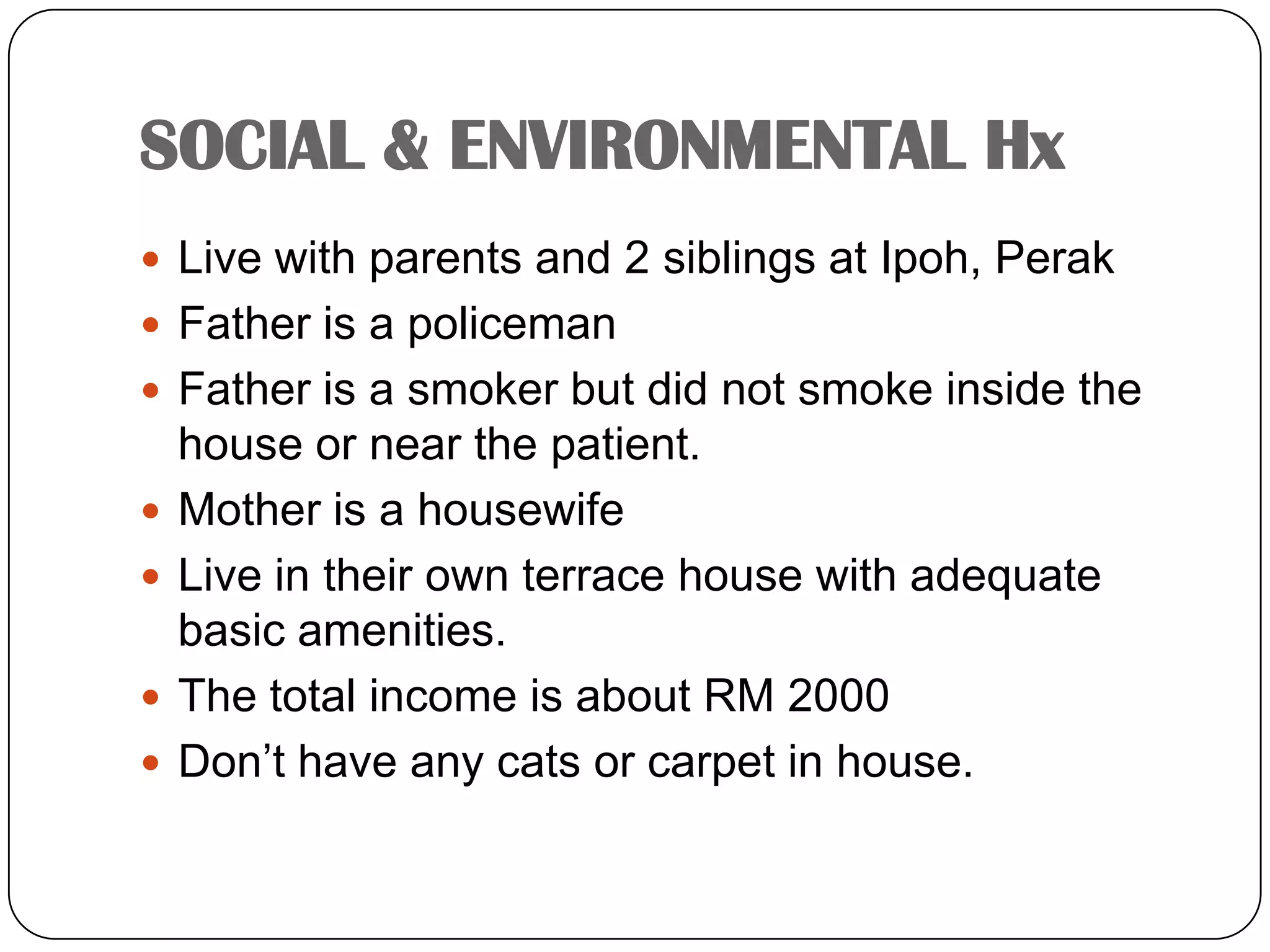
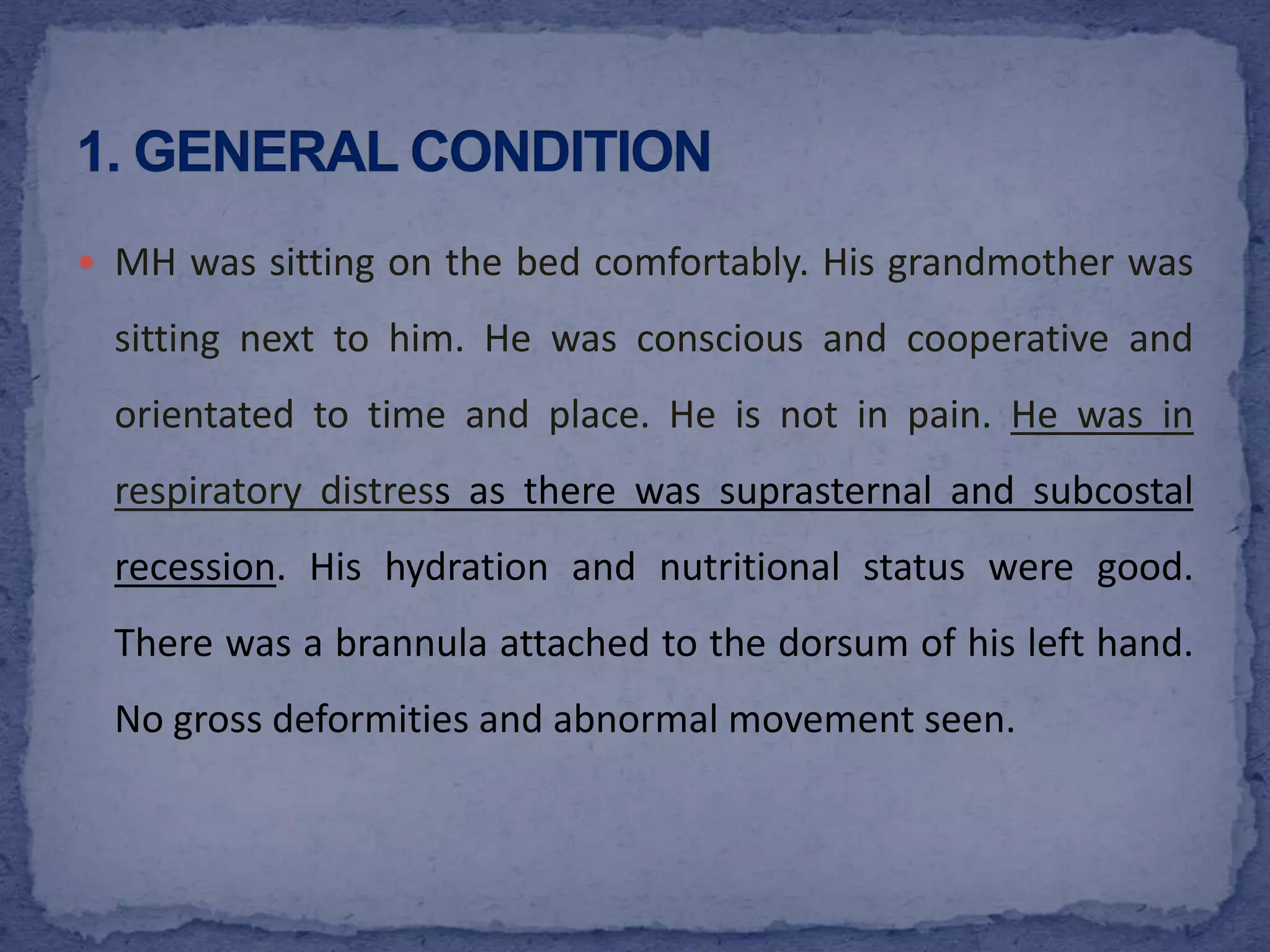
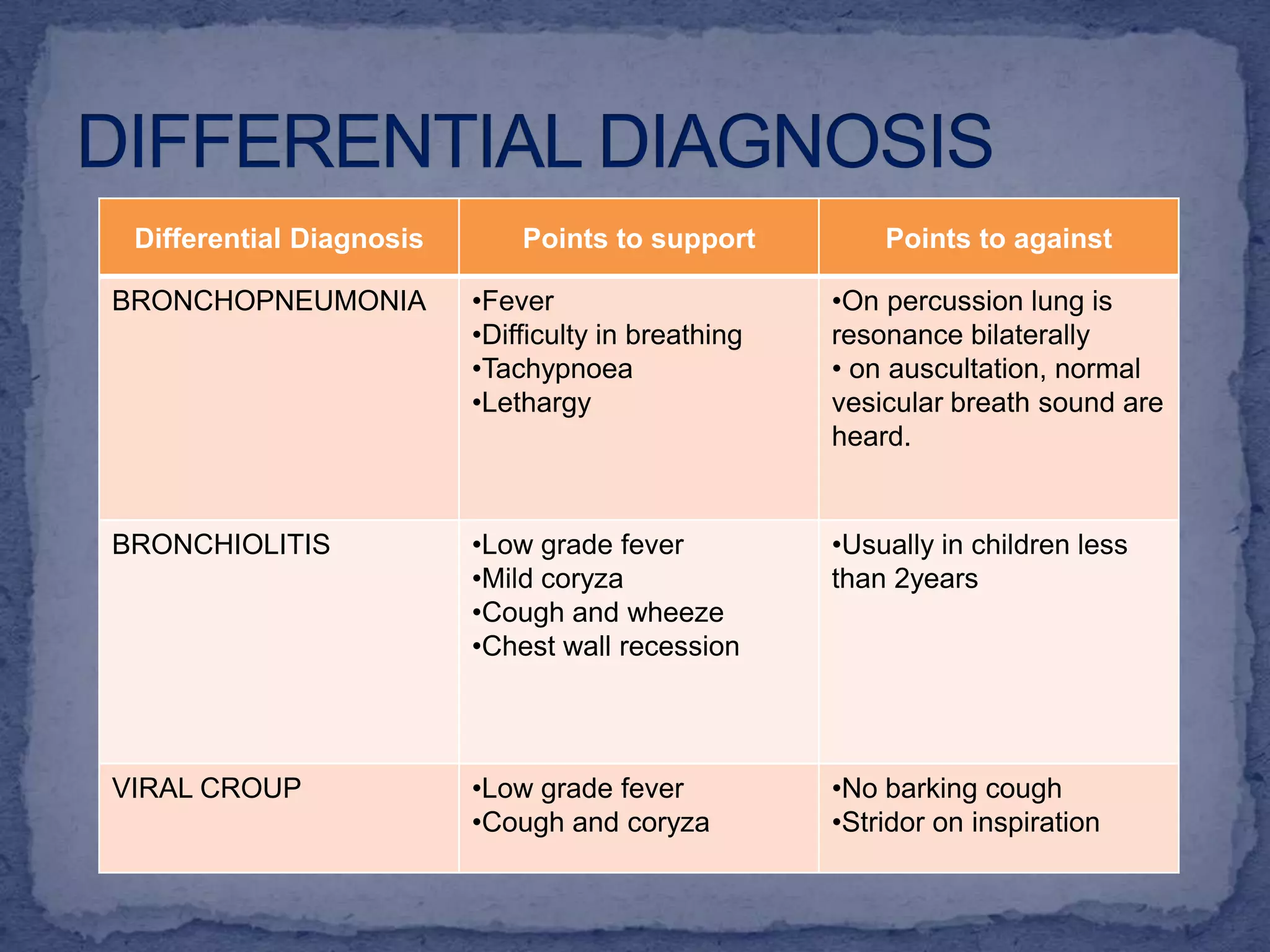
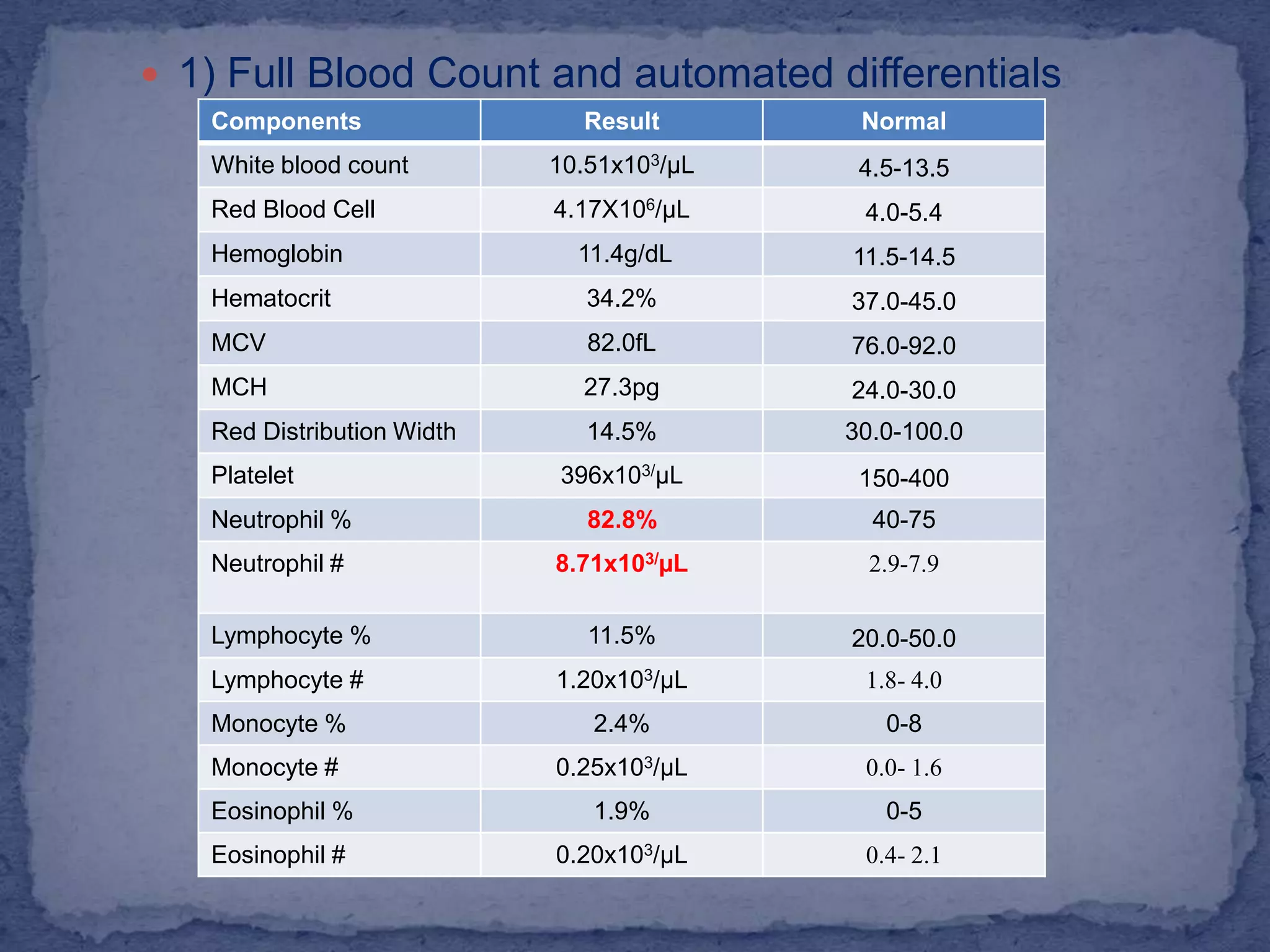
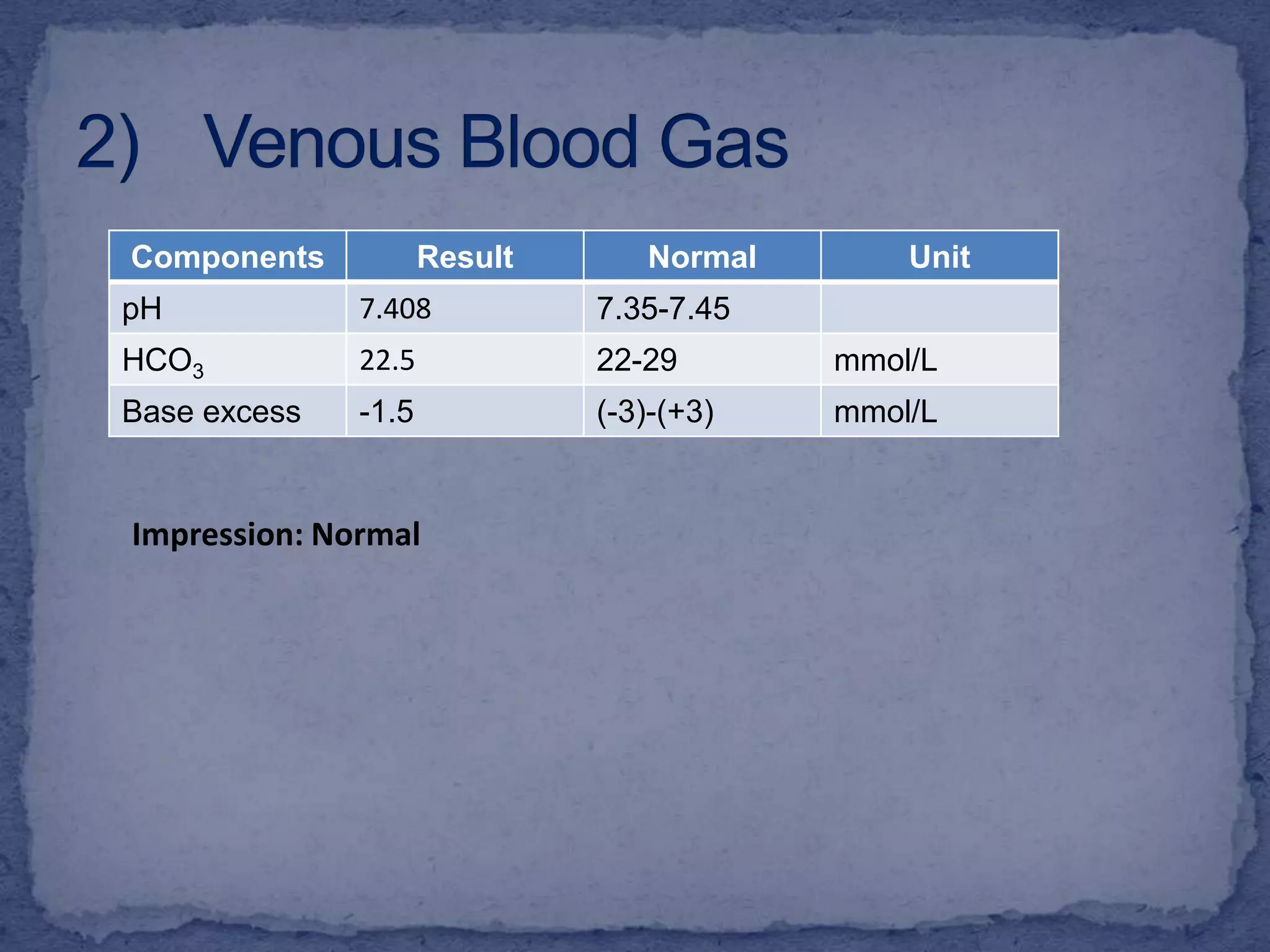
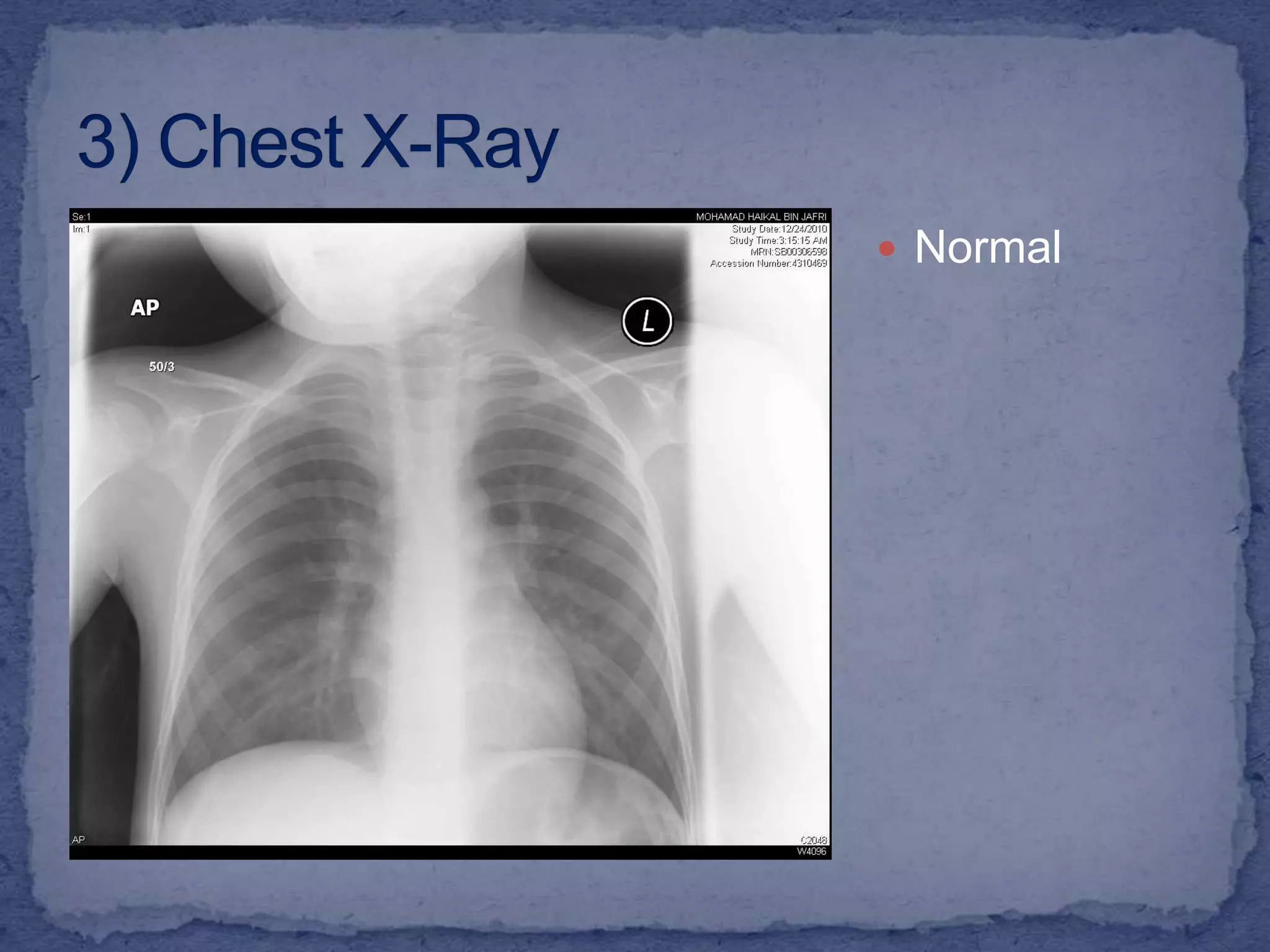
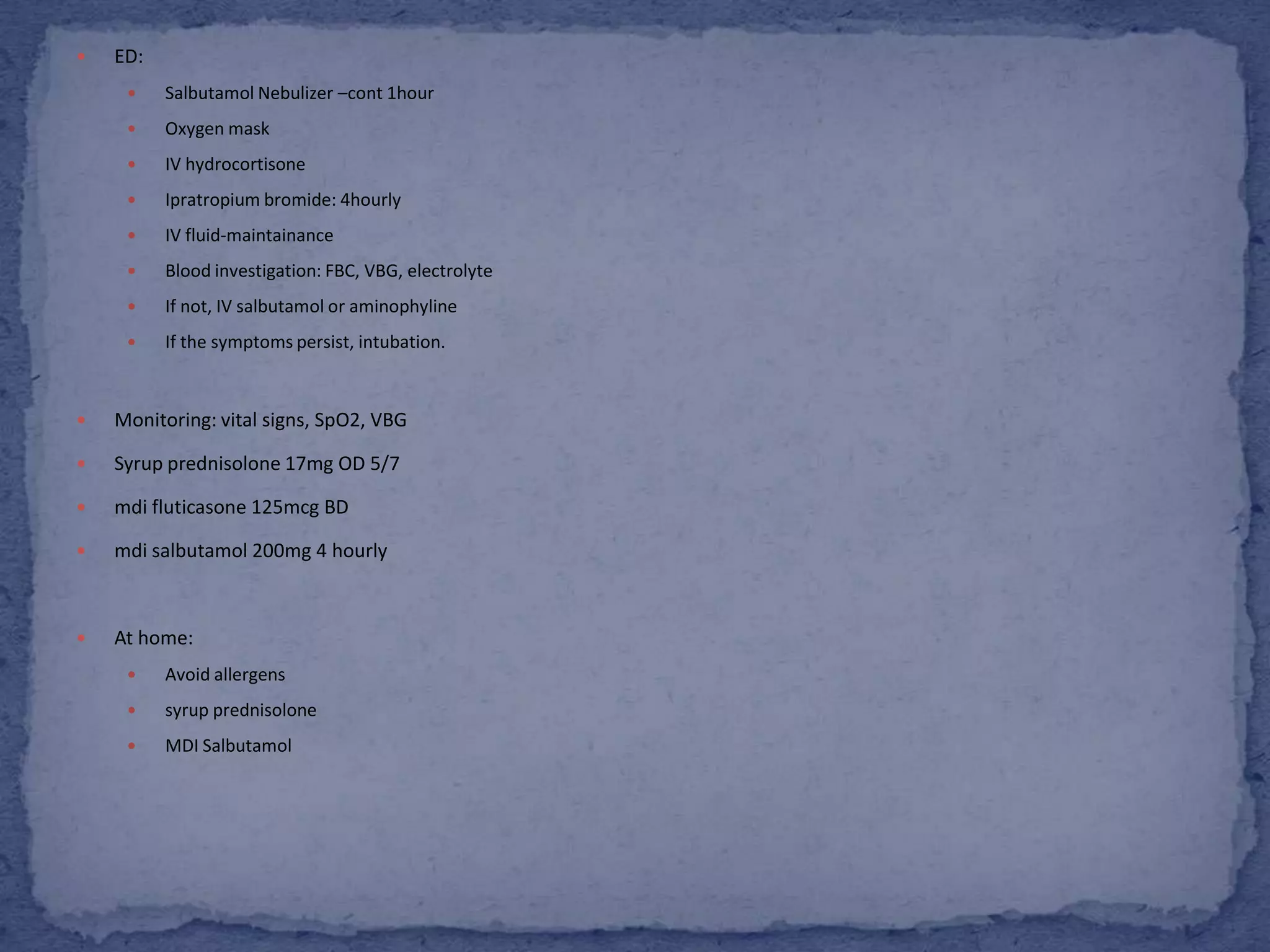
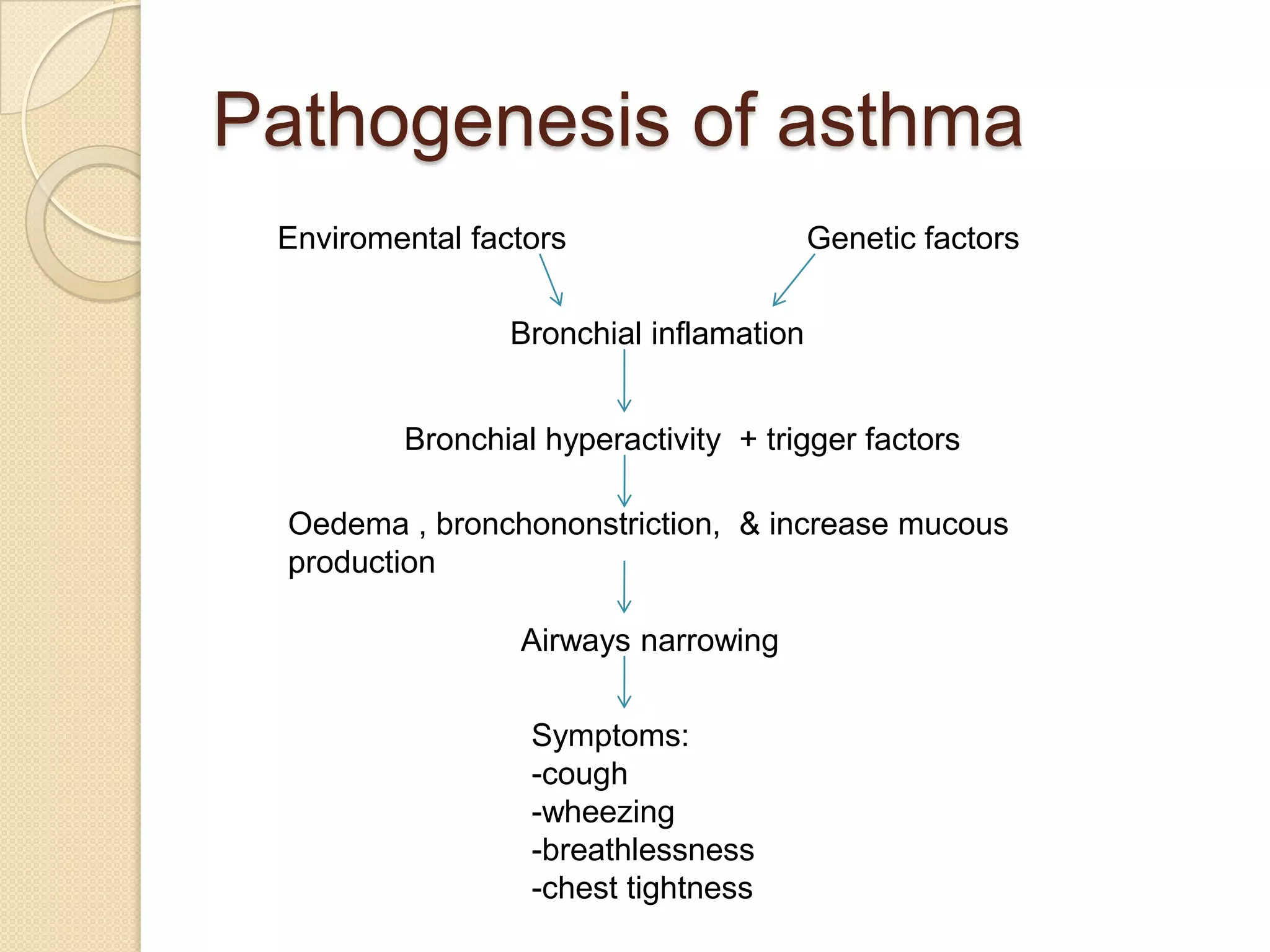
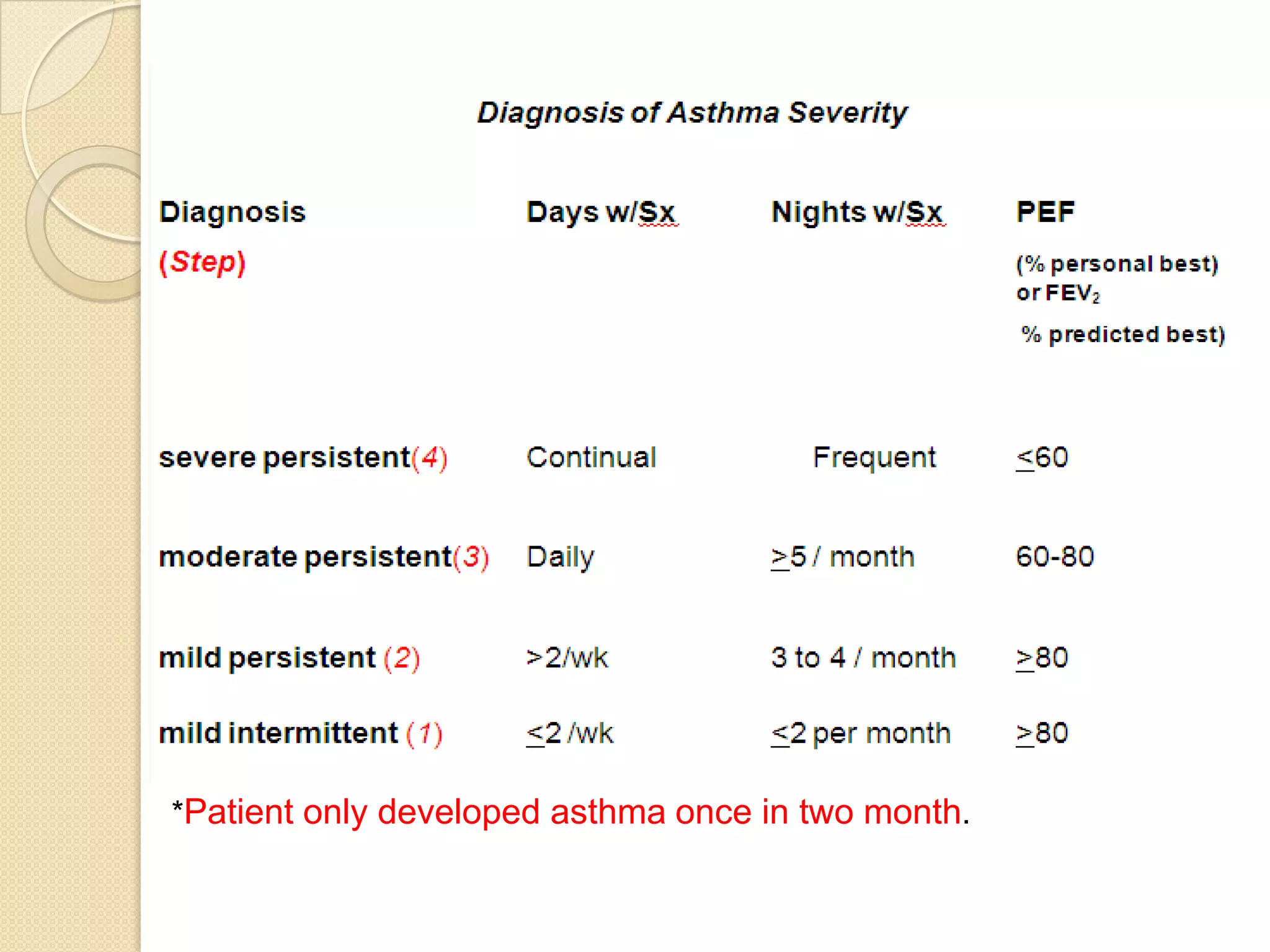
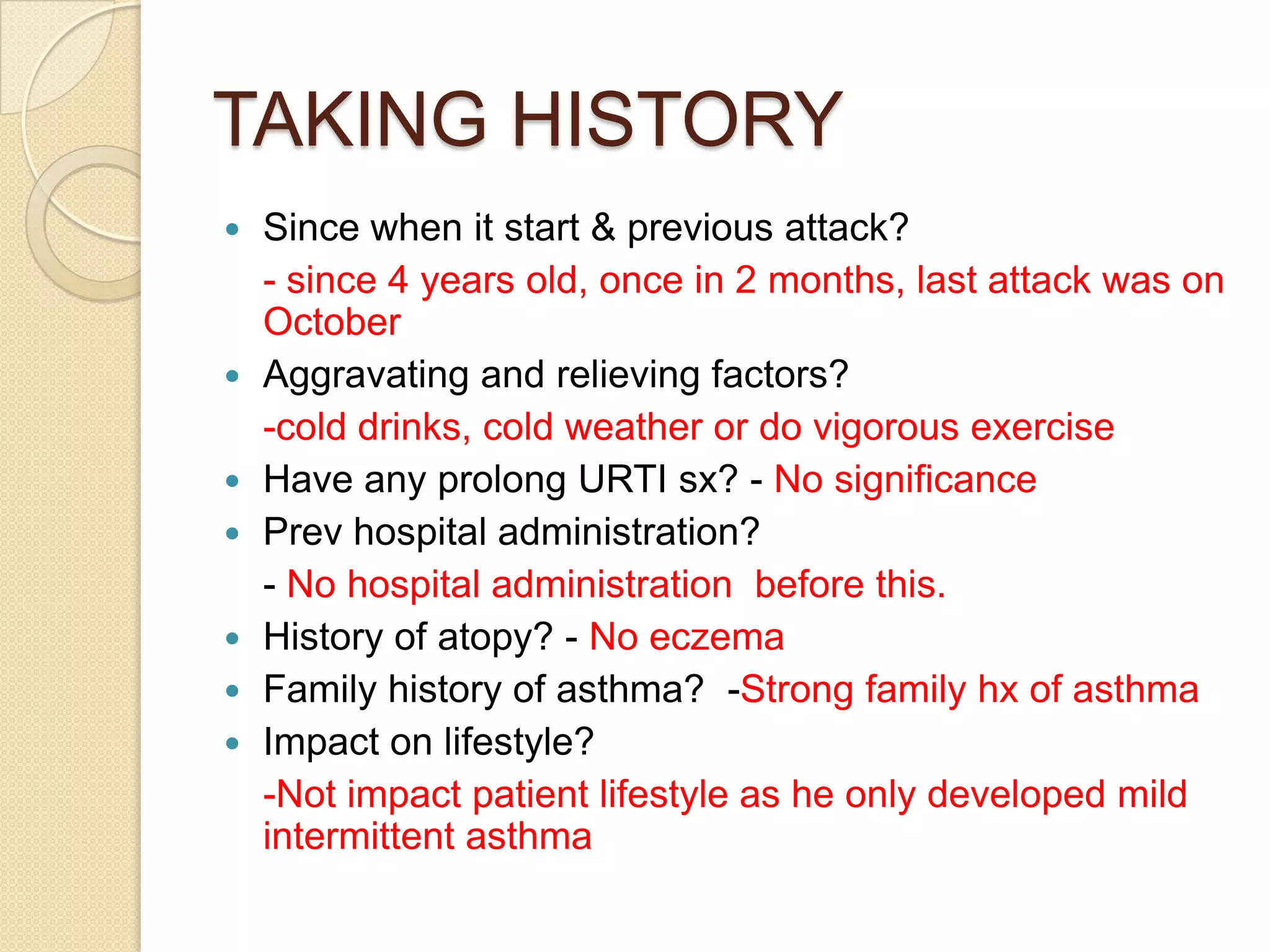
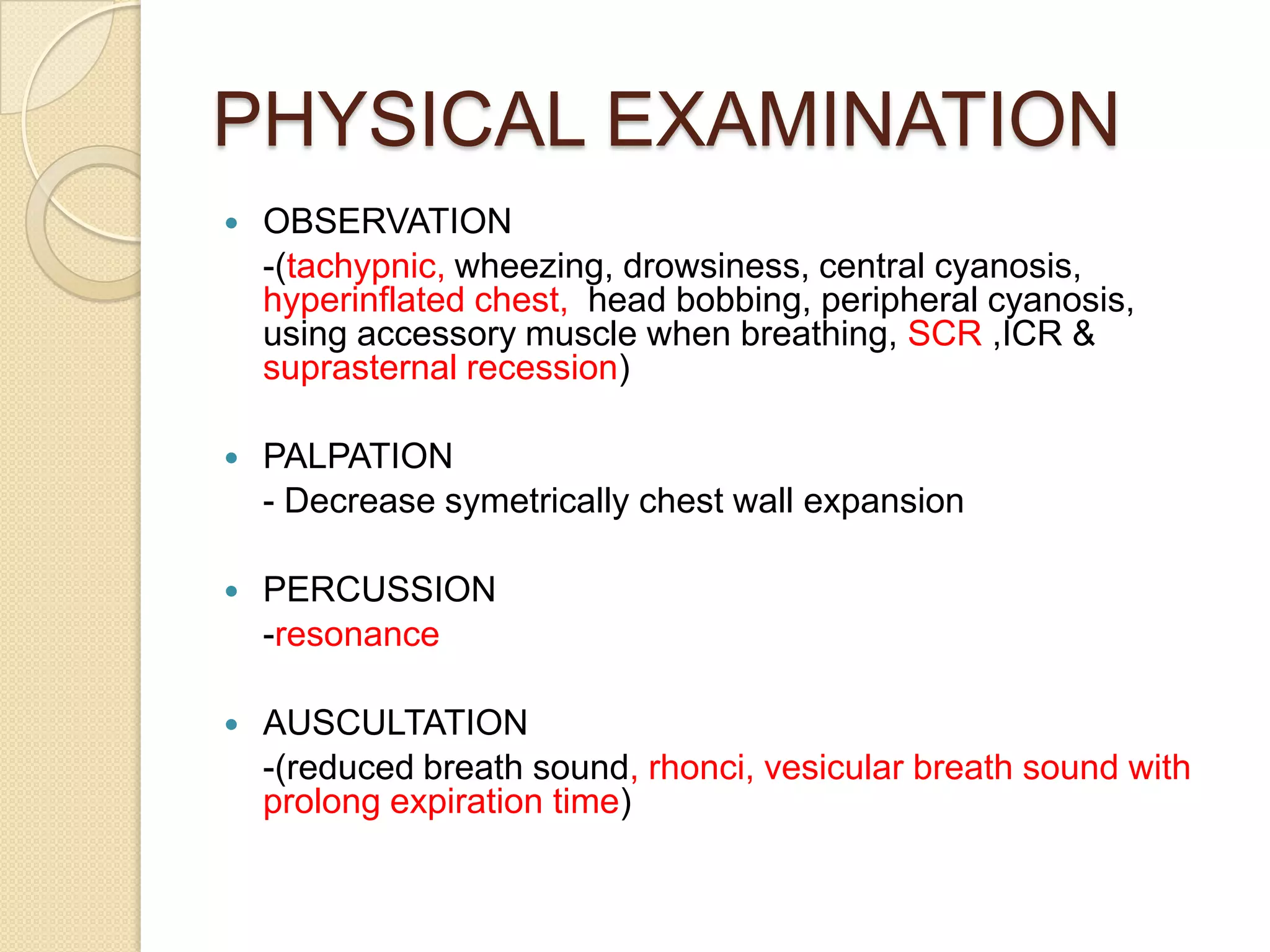
MH, a 6-year-old Malay boy with a history of asthma and G6PD deficiency, presented with fever, cough, and vomiting for one day followed by shortness of breath and rapid breathing. On examination, he had a barrel-shaped chest with suprasternal and subcostal recession, prolonged expiratory breath sounds, and rhonchi bilaterally. He was given a provisional diagnosis of an asthma exacerbation based on his history of asthma and current respiratory symptoms and signs. Differential diagnoses and further investigations were pending.