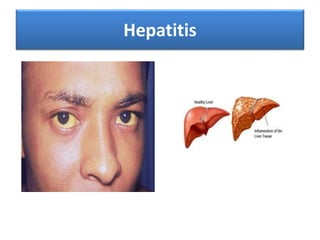
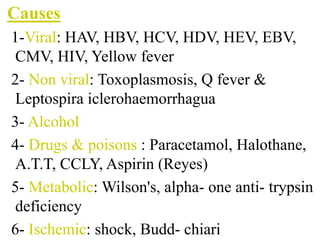
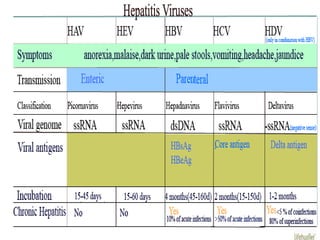
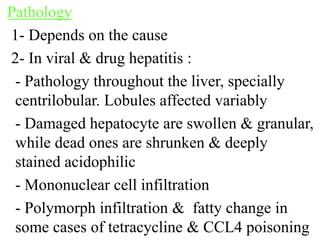
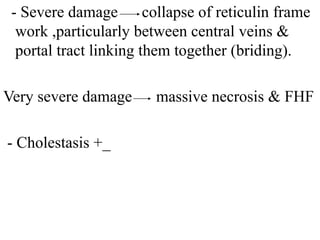
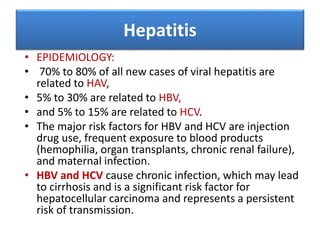
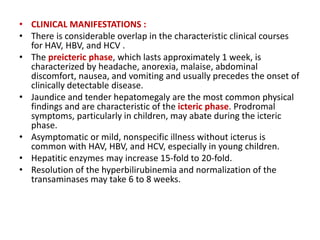
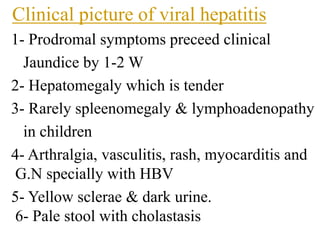
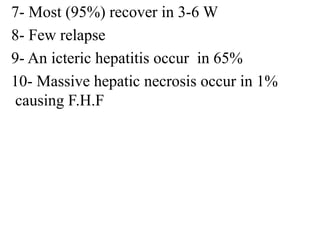
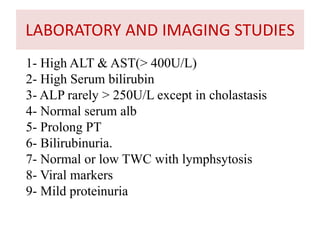
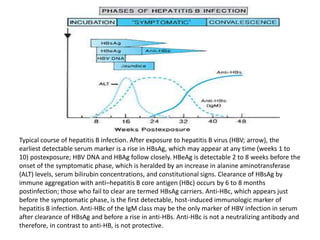
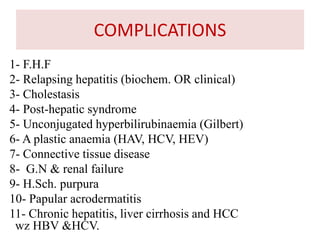
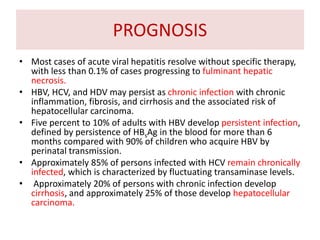
This document provides information about hepatitis including its definition, causes, pathology, epidemiology, clinical manifestations, laboratory/imaging studies, treatment, complications, prognosis, and prevention. It defines acute and chronic hepatitis. It describes the most common viral causes of hepatitis as HAV, HBV, HCV, HDV, and HEV. It discusses the clinical picture and typical course of viral hepatitis and laboratory findings. It covers hepatitis diagnosis and markers for HAV, HBV, and HCV. It addresses treatment approaches and vaccination for hepatitis B prevention. It also discusses fulminant hepatic failure as a rare but severe complication of acute hepatitis.