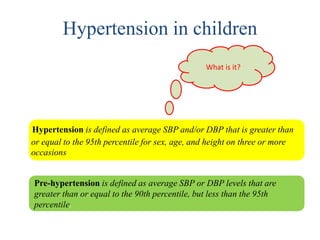
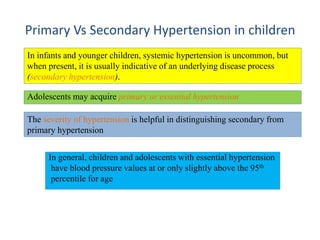
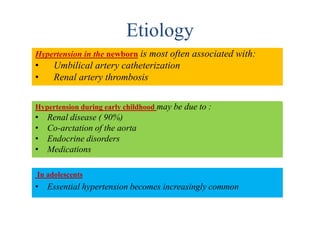
This document discusses approaches to diagnosing and treating hypertension in children. It defines hypertension and outlines stages of severity. In infants and young children, hypertension is usually secondary to an underlying condition, while adolescents can develop primary or essential hypertension. Evaluation involves measuring blood pressure properly, considering causes of secondary hypertension, assessing for target organ damage like left ventricular hypertrophy, and determining if hypertension is primary or secondary. Treatment involves lifestyle changes, weight management if overweight, and potentially medications to lower blood pressure below guidelines.









![Target-Organ Abnormalities in Childhood Hypertension
• Left ventricular hypertrophy (LVH) is the most common evidence of target-organ
damage (40%).
• Pediatric patients with established hypertension should have echocardiographic
assessment of left ventricular mass at diagnosis and periodically thereafter.
• LV Mass (g) = 0.80 [1.04 (IVS + LVED + LVPW)³ – (LVED)³] + 0.6
Left ventricular end-diastolic dimension (LVED), Intraventricular septal thickness (IVS),
Left ventricular posterior wall thickness (LVPW)
• The presence of LVH is an indication to initiate or intensify antihypertensive therapy.
Other target-organ abnormalities (such as determination of carotid intimal-medial
thickness and evaluation of urine for microalbuminuria) is not recommended for routine
clinical use.
A conservative cut point that determines the presence of LVH is 51 g/m² ͘⁷](https://image.slidesharecdn.com/pediatrichypertension-170215161201/85/Pediatric-hypertension-14-320.jpg)




