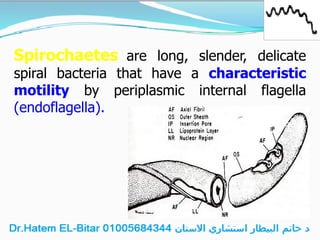
Spirochaetes are spiral bacteria including the pathogenic Treponema pallidum, which causes syphilis. The disease progresses through stages—primary, secondary, latent, and tertiary—each with distinct clinical symptoms and diagnostic methods, primarily relying on serology. Treatment typically involves penicillin, with various diagnostic tests available to confirm the infection at different stages.